Hepatoma 18 AUG
advertisement
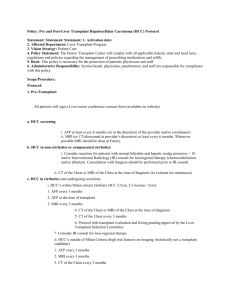
HEPATOCELLULAR CARCINOMA Monton HCC in Thailand • • • • Most common cancer in Thai male Incidence 5 x 100,000 / year Male : female = 3-8:1 Age > 40 yr HCC in Thailand • 60-90% associated with cirrhosis • Risk factor – – – – HBV 35-85% HCV 18.6% Alcohol ~10% etc. aflatoxin Multisteps carcinogenesis CIRRHOSIS AFLATOXIN INITIATION PHASE HBV HBC ALCOHOL PROMOTION PHASE Cause of death • Hepatic failure • GI bleeding • Cancer death 39-45% 13.8-23.3% 10% Diagnostic criteria EASL conference 2000 • Cyto-histological criteria • Non-invasive criteria(cirrhosis) 1.Radiological criteria : 2 imaging - focal mass > 2 cm - 1 imaging show hypervascularization 2.Combined criteria - 1 imaging mass >2cm,hypervascularization - AFP > 400 ng/ml Staging • No standard staging system • Most system focus on 1.performance status 2.tumor characteristics intrahepatic and extrahepatic 3.liver function • French,CLIP,BCLC,CUPI,TNM Treatment • Curative – Surgery – Liver transplantation – Percutaneous : PEI,RFA • Palliative – TACE – Hormone – Systemic chemotherapy Surgery • First choice in non-cirrhotic pt • 5yr survival ~ 50% • High recurrent rate : 50% in 3yr • Suspect undetected micrometastasis • 4,000-10,000 baht Liver transplantation • Cure underlying cirrhosis • 5yr survival ~ 70% • Milan criteria • 1 mass • 3 mass , < 5 cm , < 3 cm • Less available • Long term immunosuppression • 300,000 – 500,000 Baht Percutaneous • • • • • Alternative in unresectable tumor No destruction to non-tumor tissue Can do in cirrhosis Tumor seeding is problem PEI : percutaneous ethanol injection – 2,000 baht • RFA : radiofrequency ablation – 40,000 baht TACE • Transarterial chemoembolization • Palliative treatment • Principle – Cytotoxic agent(doxorubicin/cis) + lipiodol – Embolization • Improvement in 2yr survival • 10,000 – 30,000 baht Contraindication of TACE • Decompensated cirrhosis particularly bilirubin > 2 mg/dl • Encephalopathy • Reverse or absent portal flow • Tumor burden > 50% of liver • Renal failure • Active infection Systemic therapy • Hormonal rx – not improve survival • Systemic chemotherapy – not improve survival compared with best supportive care Future trends • Antiangiogenic agent – Vascular endothelial growth factor inhibitor • Immunotherapy – Tumor specific effector T-cell • Gene therapy – Intratumoral immunomodulatory cytokine Problem • • • • Most patients are unresectable High recurrent rate after surgery Cannot detect micrometastasis Early detection of HCC is appropriate HCC surveilance • Focus on cirrhotic patients • Tumor doubling time ~ 6 mo • Tools are 1. AFP 2. Ultrasonography AFP • Produced from – Fetal liver cell – Yolk sac • Normal range 10-20 ng/ml • AFP increases in – exacerbation of chronic viral hepatitis (20-250 ng/ml) – Germ cell tumor AFP cut-off Cut-off sens spec NPV PPV 20 200 400 60 22.4 17.1 89.4 99.4 99.4 97.7 25.1 Trevisani et al,J Hepatol,2001 USG • Sensitivity USG CT MRI 79.4 87.6 88.9 Yao et al,J Hepatol,2001 Surviellance & recall strategy USG/AFP q 6mo liver nodule 1-2cm >2cm FNAB AFP>400 imaging no nodule <1cm AFP^ AFP- spiralCT USG/3mo no HCC HCC surveillance/6mo Bruix J et al. J Hepatol,2001 Thank you