Pruritus in Pregnancy - Family Medicine Resident Presentations
advertisement

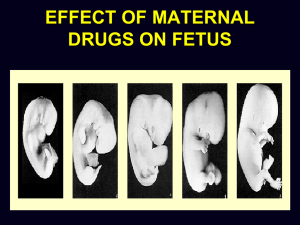
Pruritus in Pregnancy Carol Mendez, MD Albert Einstein College of Medicine Montefiore Medical Center Department of Family and Social Medicine April 29, 2010 Pruritus in Pregnancy • Normal skin changes: linea nigra, melasma, striae distensae. • Unrelated to pregnancy: flare of preexisting dermatosis • Without rash – Intrahepatic cholestasis of pregnancy • With rash – Related to pregnancy • Early onset, trunk & limbs involved: atopic eruption • Late onset, predominant abdominal involvement – Polymorphic eruption of pregnancy – Pemphigoid gestationis Intrahepatic Cholestasis of Pregnancy • Occurs in 3rd TM • Incidence 1 in 100 to 150 pregnancies, #2 cause of jaundice in pregnancy • Pruritus without primary lesions • Only secondary excoriations/prurigo nodularis • Elevated total serum bile acid levels • Prematurity, fetal distress, stillbirths • Spontaneous resolution after delivery • Synonym: pruritus gravidarum Causes and Pathogenesis • Unclear • Probably increased hepatic sensitivity to estrogen • Risk factors: hepatitis C virus associated with ICP Clinical Picture-ICP • Symptoms are worst at night • Trunk, Palms and Soles • Jaundice, clay colored stools, dark urine – 20%-50% of patients • Steatorrhea can lead to vit. K malabsorption and prolongation of PT risk of hemorrhage. • LAB: mild-moderate elevation of transaminases, marked elevation in alkaline phosphatase • Bile acid levels 10-100x normal Fetal risks with ICP • Distress, still birth and preterm delivery • Neonatal respiratory distress syndrome • Placental anoxia from vasoconstriction of placental chorionic veins from toxic bile acids and meconium. • Can be reduced by tx and delivery b/t 36-38 weeks with favorable lung maturity and cervix. Treatment of ICP • Mild: symptom relief with emollients and topical antipruritics. – Systemic antihistamines are not useful – Ursodeoxycholic acid (UDCA)-naturally occuring hydrophilic bile acid that enhances excretion of hydrophobic bile acids, other hepatotoxic compounds, and sulfated progesterone metabolites. • Controls pruritus and serologic abnormalities • Works faster than cholestyramine, safe for mother and fetus • May result in decreased fetal mortality associated with ICP – Plasmapheresis – Cholestyramine may be effective up to 50% • May precipitate vit K worsening coagulopathy Prognosis • Recurrence in subsequent pregnancies: 60% to 70% • Use of oral contraceptives • Resolves within the first month after delivery Early onset-trunk and limbs involved Atopic Eruption of Pregnancy • • • • • Very common, incidence 1 in 300 to 450 20% exacerbated atopic dermatitis 80% firm manifestation Lab: elevated IgE levels No maternal or fetal risk Cause of AEP • Unknown • Reported cases of increased IgE • Cholestasis Clinical Course-AEP • Onset during 2nd and 3rd TM • Discrete, excoriated papules, predominnately on extensor surfaces and occasionally on abdomen. • May last for weeks to months after delivery with variable recurrence in subsequent pregnancies. Treatment of AEP • Topical corticosteroids • Ultraviolet B light therapy • Benzoyl Peroxide Late onset-3rd TM Predominant Abdominal Involvement • Polymorphic Eruption of Pregnancy (Pruritic Urticarial Papules and Plaques of Pregnancy) – Abdominal striae sparing umbilicus – No fetal risk • Pemphigoid Gestationis – Vesiculo-bullous eruption on urticated erythema – Periumbilical involvement – Small for dates babies Polymorphic Eruption of Pregnancy (PUPPP) • • • • • • • Papular urticarial eruption Mostly in primiparous women Begins within abd. striae, sparing umbilicus Resolves spontaneously & rapidly postpartum No maternal or fetal risk Rarely recurs Incidence is 1 in 120 to 240 pregnancies Causes of PEP/PUPPP • Association with multiple gestation • Rapid, late stretching of abdominal skin Clinical presentation- PEP • Late 3rd TM and immediate postpartum period • Intensely pruritic erythematous papules, 1-3 mm, quickly coalescing into urticarial plaques. • Tiny vesicles, 2mm, may occur in the plaques, but bullae are absent. • Begin in abd. striae and spread in days to abdomen, buttocks, thighs, upper inner arms, and lower back. • Spearing periumbilical area, face, breasts, palms, and soles. No mucus membrane lesions. PUPP Striae Treatment of PEP/PUPPP • Potent topical corticosteroids, tapered off after 1 week of therapy. • Severe cases: prednisone 10-40mg/d • Oral antihistamines generally ineffective. • Resolution 7-10 days after delivery • Majority of women don’t have a recurrence. Pemphigoid Gestationis • Incidence is 1 in 50,000 • Intensely pruritic vesiculobullous eruptions on urticated erythema with periumbilical involvement • Late 3rd TM or immediate postpartum period. • Lesions begin within or adjacent to umbilicus. • Increased risk of small for gestational age births, risk of prematurity and 5% of babies have urticarial, vesicular, or bullous lesions-resolve spontaneously. • Dx: 2 skin biopsies for histology and direct immunofluorescence • Synonyms: – gestational pemphigoid – Herpes gestationis Pathophysiology of PG • Production of autoantibody with potential crossreactivity between placental tissue & skin. • 100% incidence of anti-human leukocyte antigen (HLA) antibodies • Subepidermal blisters on H&E stain • Immunofluorescence microscopy: linear C3 depositions along dermal-epidermal junction Clinical Course-PG • Abrupt onset of intensely pruritic urticarial lesions on the trunk progressing in generalized fashion spreading along face, mucous membranes, palms, and soles. • A flare at delivery in 75% of cases. • Recurs with subsequent pregnancies, menstruation, and use of oral contraceptive. • Complete resolution in weeks to months postpartum. Pemphigoid Gestationis Treatment of PG • Suppressing blister formation and relieving pruritus. • Prednisone, 20-40mg/d, higher doses may be required, tapering to lowest effective dose. • Refractive cases: cyclophosphamide, pyridoxine, dapsone, cyclosprine, gold, methotrexate, and plasmapheresis. • No available controlled trials • Follow up: risk for development of Grave’s dz. Conclusion • Pruritus in pregnancy can be due to a flare of conditions before conception or related to pregnancy specific dermatoses. • Generalized pruritus without a rash should prompt an evaluation for ICPbile acids. • If pemphigoid gestationis is suspected, skin biopsies are needed. – Antepartum fetal monitoring may be indicated. • Goal of treatment otherwise is symptom relief. Reference • Olin, Stephen T. “Dermatoses of Pregnancy.” Family Medicine Obstetrics. Ed. Stephen D. Ratcliffe, et al. 3rd ed. Philadelphia, PA: Mosby Elsevier, 2008. 317-321. Print. • Woff, Klaus and Richard Allen Johnson. Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. New York: McGraw Hill, 2009. Print. • “Cholestasis of Pregnancy.” DynaMed. 01 Mar. 2010. Web 24 Apr. 2010 • Pictures are from UpToDate online 18.1, “Dermatoses of Pregnancy”. Web 29 Apr. 2010