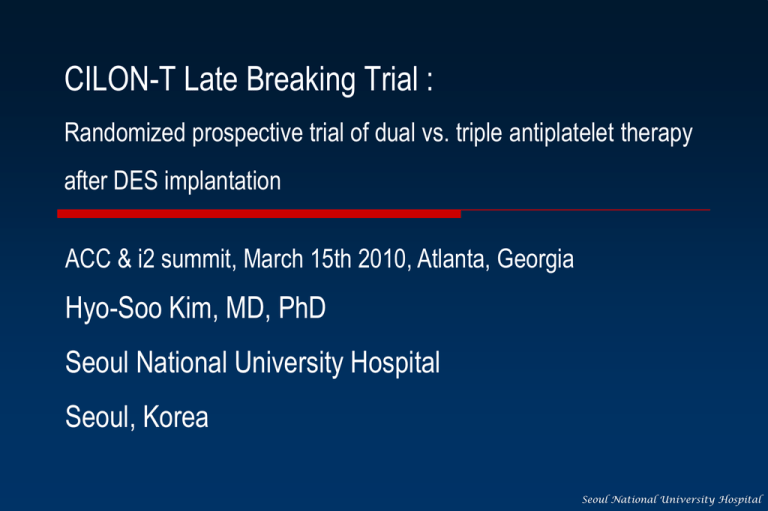
CILON-T Late Breaking Trial :
Randomized prospective trial of dual vs. triple antiplatelet therapy
after DES implantation
ACC & i2 summit, March 15th 2010, Atlanta, Georgia
Hyo-Soo Kim, MD, PhD
Seoul National University Hospital
Seoul, Korea
Seoul National University Hospital
Nothing to disclose
Seoul National University Hospital
CILON-T trial
CILostazol-based triple anti-platelet therapy ON Ischemic
Complication after drug-eluting stenT implantation
Multicenter, prospective, randomized trial
PROBE
(Prospective Randomized Open-label Blinded Evaluation)
Principal investigator
Hyo-Soo Kim, MD, PhD
Clinical trials identifier
NCT00776828
Seoul National University Hospital
CILON-T trial : participating centers
Centers
Investigators
Seoul National University Hospital
Hyo-Soo Kim, MD, PhD
Seoul National University Bundang Hospital
In-Ho Chae, MD, PhD
Konyang University Hospital
Jang-Ho Bae, MD, PhD
Korea University Guro Hospital
Seung-Woon Rha, MD, PhD
Chungbuk University Hospital
Myeong-Chan Cho, MD, PhD
Seoul National University Hospital
Background of the CILON-T trial
I. Accumulating evidences suggest the relationship
between clopidogrel resistance & clinical events.
II. Recent studies reported the value of using VerifyNow
(PRU) in predicting clinical events.
III. Efficacy of adding cilostazol in reducing clinical events has
been reported in the registry or small randomized
controlled study of specific subpopulation.
Seoul National University Hospital
Background of the CILON-T trial
Efficacy of adding cilostazol on DAT in reducing
clinical events or PRU value has not been tested
•
in the real-world all-comer patients with DES implantation
•
at the level of large randomized controlled study.
Seoul National University Hospital
Assessed for eligibility (n=976)
Randomization (n=960)
TAT (n=477)
Atorvastatin
(n=241)
Rosuvastatin
(n=236)
DAT (n=483)
Atorvastatin
(n=242)
3 Withdrawal at patient request
14 Withdrawal at clinician’s judgment
3 Failed PCI
TAT (n=457)
2 Withdrawal at patient request
19 Withdrawal at clinician’s judgment
4 Failed PCI
DAT (n=458)
915 patients with successful PCI & follow-up
at 6 month
- Cardiovascular death, nonfatal MI, ischemic stroke, TLR
- Platelet (P2Y12) reaction unit
Rosuvastatin
(n=241)
CILON-T Trial Endpoints
Primary Endpoint
Composite of clinical outcomes within six months
(cardiac death, MI, ischemic stroke & TLR)
Secondary endpoint
PRU level measured at discharge & 6 mo after the index procedure
All cause of death, stent thrombosis, and each component of primary
endpoint at six months
Safety Endpoint
Bleeding complications according to TIMI criteria
The incidence of drug discontinuation
Heart rate
Seoul National University Hospital
Key participation criteria
Inclusion criteria
Age 18~80yrs
All-comers : patients with native de-novo coronary artery lesions
for which DES implantation was feasible
Exclusion criteria
Hepatic dysfunction (GOT/GPT >*3 UNL)
Renal dysfunction (Scr>2.0mg/dl or on dialysis)
LV dysfunction (EF <30%)
Uncontrolled hematological disease
Patients taking warfarin or other anti-platelet agents
Allergy to study medications
Seoul National University Hospital
RESULTS
Seoul National University Hospital
Clinical profiles of patients
TAT (n=457)
DAT (n=458)
p
62.8±9.6
62.8±9.2
0.999
Men
321 (68.6%)
326 (68.3%)
0.935
Hypertension
291 (64.5%)
305 (66.9%)
0.454
Diabetes mellitus
160 (35.5%)
147 (32.2%)
0.303
Diet
24 (5.3%)
17 (3.7%)
OHA
103 (22.8%)
116 (25.4%)
33 (7.3%)
14 (3.1%)
107 (23.7%)
122 (26.8%)
0.470
Previous PCI
29 (6.4%)
39 (8.6%)
0.225
Previous CABG
8 (1.8%)
13 (2.7%)
0.281
Age, yrs
Insulin
Current smoker
Clinical diagnosis
0.748
Stable angina
168 (41.3%)
153 (37.1%)
Unstable angina
174 (42.8%)
196 (47.6%)
Acute myocardial infarction
42 (10.3%)
42 (10.2%)
8 (1.9%)
5 (1.2%)
Total cholesterol
176.1±39.4
177.4±4.31
LDL cholesterol
104.7±34.6
107.9±40.2
Silent ischemia
0.62
Seoul National University Hospital
0.20
Profiles of Medication at Discharge
TAT
(n=457)
DAT
(n=458)
Pvalue
Aspirin
99.8 (449)
99.8 (451)
0.997
Statin
98.9 (451)
100 (451)
0.259
Beta-blocker
52.9 (239)
51.6 (232)
0.691
ACE inhibitor or ARB
37.6 (169)
45.8 (207)
0.012
Calcium channel blocker
26.0 (117)
27.2 (123)
0.680
Nitrates
42.7 (187)
42.7 (193)
0.728
2.7 (12)
2.0 (9)
0.488
Medication at discharge
Proton pump inhibitor
Seoul National University Hospital
Angiographic profiles of patients
TAT (n=457) DAT (n=458)
Lesion locations
LAD
LCx
RCA
Left main
ACC-AHA lesion classification
A
B1
B2
C
Ostial lesions
Calcified lesions
Bifurcation lesion
Thrombus on angiography
220 (48.4%)
91 (20.2%)
105 (23.1%)
23 (5.1%)
222 (49.3%)
107 (23.5%)
124 (27.6%)
13 (2.9%)
p
0.166
0.633
12 (2.8%)
126 (29.7%)
55 (13.0%)
231 (54.5%)
112 (24.5%)
105 (24.1%)
145 (31.7%)
34 (7.8%)
10 (2.3%)
126 (29.1%)
46 (10.6%)
251 (58.0%)
109 (23.8%)
128 (29.3%)
132 (28.8%)
38 (8.7%)
0.802
0.092
0.556
0.637
Seoul National University Hospital
Procedural profiles of patients
TAT (n=457) DAT (n=458)
P
Lesion length, mm
21.1±13.4
22.2±13.9
0.244
MLD, mm
0.75±0.49
0.79±0.50
0.246
Reference vessel diameter, mm
2.96±0.52
2.93±0.52
0.416
No. of stent / lesion
1.23±0.51
1.18±0.44
0.164
Post-procedural MLD, mm
2.29±0.51
2.23±0.51
0.107
Type of stents
0.102
Paclitaxel-eluting (TAXUS)
228 (49.9%)
225(49.1%)
Zotarolimus-eluting (Endeavor)
194 (42.5%)
207 (45.2%)
156 (34.1%)
163 (35.6%)
Multi-lesion intervention
0.64
Seoul National University Hospital
Results: P2Y12 reaction unit (PRU): TAT vs DAT
PRU
340
p < 0.001
p < 0.001
TAT
DAT
300
260
220
255.7
232.1
180
206.6
210.7
140
100
At discharge
After 6 months
Seoul National University Hospital
Results: Change of PRU for 6 months : TAT vs DAT
P2Y12 reaction unit (PRU)
TAT
DAT
p < 0.001
p =0.23
At discharge
6 mo
At discharge
6 mo
Seoul National University Hospital
Results: Clinical outcomes depending on PRU value
Composite of
CD, nonfatal MI,
ischemic stroke & TLR
Composite of
CD, nonfatal MI
& ischemic stroke
TLR
p=0.077
p=0.486
p=0.037
Seoul National University Hospital
Results: Clinical outcomes depending on anti-plt regimen
TAT (n=457)
DAT (n=458)
p
39 (8.5%)
42 (9.2%)
0.73
4 (0.9%)
6 (1.3%)
0.75
0
3 (0.7%)
0.25
Nonfatal MI
4 (0.9%)
3 (0.7%)
0.73
Ischemic stroke
5 (1.1%)
4 (0.9%)
0.75
TLR
30 (6.6%)
32(7.2%)
0.79
Stent thrombosis
3 (0.7%)
5 (1.1%)
0.73
Death, nonfatal MI, ischemic stroke
13 (2.8%)
13 (2.8%)
1.0
CD, nonfatal MI, ischemic stroke
9 (2.0%)
10 (2.0%)
1.0
Primary endpoint
CD, nonfatal MI, ischemic stroke and TLR
Secondary endpoint
Death from any cause
Cardiac death
Seoul National University Hospital
Results: Clinical outcomes depending on anti-plt regimen
Triple anti-PLT regimen
Double anti-PLT regimen
Composite of
CD, nonfatal MI
& ischemic stroke
Composite of
CD, nonfatal MI,
ischemic stroke & TLR
TLR
p=0.818 for log-rank test
p=0.742 for log-rank test
p=0.701 for log-rank test
9.2%
7.2%
8.5%
6.6%
2.0%
2.0%
DAT
458
452
450
425
416
DAT
458
452
451
449
447
DAT
458
458
449
426
418
TAT
457
450
449
428
418
TAT
457
452
452
451
448
TAT
457
450
449
429
421
Seoul National University Hospital
Distribution of PRU in pts with MACCE
Seoul National University Hospital
PRU value versus Anti-PLT regimen to predict MACCE
Composite of
CD, nonfatal MI,
ischemic stroke & TLR
Composite of
CD, nonfatal MI
& ischemic stroke
TLR
Seoul National University Hospital
Subgroup analysis : TAT vs DAT
Baseline characteristics
HR
95% CI
0.78
1.02
0.37-1.60
1.34
0.64
0.69-2.58
0.32-1.29
0.66
3.41
0.39-1.13
1.12-10.4
Lesion length
≥ 28mm
<28mm
0.79
0.70
0.34-1.84
0.38-1.31
Reference vessel diameter
<2.75mm
≥2.75mm
0.80
0.85
0.38-1.69
0.45-1.60
Diabetes
Yes
No
Age
≥ 65 yr
<65 yr
Sex
Male
Female
0
TAT better
1
0.57-1.83
2
DAT better
Seoul National University Hospital
Results: Safety outcomes : TAT vs DAT
Variable
TAT (n=457)
DAT (n=458)
Bleeding complications
P
0.511
Major
2 (0.4%)
1 (0.2%)
Minor
1 (0.2%)
0 (0%)
30 (6.6%)
3 (0.7%)
<0.001
Baseline
69.7±11.9
69.2±12.7
0.62
6 months
73.3±12.0
68.4±13.7,
<0.001
Drug discontinuation
Heart rate, /min
Seoul National University Hospital
Results: Independent predictors for MACCE
(Cox-regression analysis)
Risk factor
Unadjusted HR (95% CI)
Adjusted HR (95% CI)
1.75 (1.07~2.86)
1.90 (1.05~3.43)
1.42 (1.04~1.93)
1.63 (1.12~2.37)
Use of cilostazol
0.91 (0.59~1.41)
0.88 (0.50~1.56)
Diabetes mellitus
1.22 (0.78~1.91)
1.53 (0.86~2.73)
Lesion length ≥28mm
(vs. <28mm)
High PRU level
(every increase of tertile)
Female
0.65 (0.39~1.10)
0.64 (0.33~1.24)
Hypertension
1.31 (0.81~2.13)
1.29 (0.67~2.52)
Age
1.02 (0.99~1.04)
1.01 (0.97~1.04)
Diagnosis of AMI
0.62 (0.25~1.53)
1.01 (0.36~2.86)
Seoul National University Hospital
Study limitations
Open-label study, but with blinded evaluation
Platelet reactivity measured by single method
Not powered to verify the effect of cilostazol on the hard
endpoint, such as CD, nonfatal MI or stent thrombosis
Seoul National University Hospital
Summary of CILON-T randomized controlled trial
TAT achieved lower PPR (post-treatment platelet reactivity)
than DAT.
But it did not necessarily reduce MACCE within six months after
DES implantation,
because there were substantial numbers of hypo-responders
even to TAT.
The importance of PPR is reflected by the finding that the
patients with low PPR (PRU < 210 unit) did not develop any
thrombotic event (CD, MI, or ischemic stroke) irrespective of
anti-platelet regimen.
Seoul National University Hospital
Conclusion of CILON-T randomized controlled trial
Tailored decision on the adjunctive use of cilostazol
according to PPR (post-treatment platelet reactivity)
may be important to reduce clinical events in patients
with DES implantation.
Seoul National University Hospital