Extreme MAKEOVER - Connecticut Speech-Language
advertisement

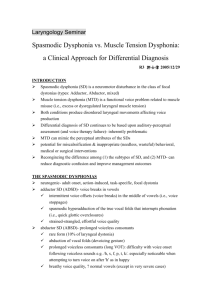
Extreme MAKEOVER Larynx edition Diagnosis and Treatment of Muscle Tension Dysphonia Starr Cookman, M.A., CCC-SLP “A rose by any other name . . . ” Functional Dysphonia – Vocal disruption without organic cause – Also called: Hyperfunctional Dysphonia Psychogenic Dysphonia (Aphonia) Non Organic Dysphonia Vocal Hyperfunction Muscular Tension Dysphonia Hyperkinetic Dysphonia Laryngeal Tension-Fatigue Syndrome Laryngeal Isometric Dysphonia Classification System, Koufman & Blalock 1991 Functional Dysphonia (Umbrella Term) – 6 Subtypes Conversion Habituated Hoarseness Inappropriate Falsetto Vocal Abuse Syndromes Post Operative Dysphonia Relapsing Aphonia Vocal Abuse Syndromes Tension Fatigue Syndrome Bogart-Bacall Syndrome Nodules Reinke’s Edema Vocal Process Ulcer/Granuloma Muscular Tension Dysphonia (MTD) Morrison – “Inability of the arytenoids to come together” Posterior Glottal Gap Over-specificity later corrected – MTD separated into 4 types Type Type Type Type 1 2 3 4 = = = = PGG Ventricular Compression Anterior-Posterior Compression Spincteric Larynx Challenges “Functional Dysphonia” – Implies voluntary “misuse” of the larynx – Not descriptive Subtypes are numerous – Over classification – No evidence of generalization into voice clinics Proposed Classification System Umbrella Term: Muscle Tension Dysphonia (Aphonia) – Vocal disruption resulting from an imbalance of laryngeal musculature – Advantages Descriptive Does not imply etiology Easier for patient 4 Subtypes of MTD Psychogenic Habituated Compensatory Contributory Psychogenic MTD Onset – Sudden – Can be linked to psychologically disruptive event – No concomitant URIs Progression – Usually little to no change over time Psychogenic MTD (cont.) Voice quality – aphonic, whispery, monotone, constant, severe dysphonia, glottal fry, vegetative tasks are normal Acoustic Studies – Yanigahara hoarseness rating 3-4 – Elevated perturbation measures – Abnormal fundamental frequency Psychogenic MTD (cont.) Laryngeal Presentation – Structure = normal – Function = Arytenoids held open, arytenoids pressed, ventricular compression, sphincteric supraglottis, arytenoids mobile EMG – Normal Response to speech therapy – Excellent Habituated MTD Etiology – Associated with laryngeal disturbance Chemical exposure Upper respiratory infection Laryngeal Trauma Reflux Laryngeal Surgery Habituated MTD (cont.) Progression – Extended course – Consistent voice quality across time/settings – Patient complains of laryngeal pain/ fatigue – Secondary gain may be present Habituated MTD (cont.) Voice Quality – glottal fry, breathiness, roughness, diplophonia, sustained phonation worse than conversation, abnormal pitch/register (falsetto), vegetative tasks are normal – Acoustics – Yanigahara 2 - 3 – Elevated perturbation – Range restrictions Habituated MTD (cont.) Laryngeal Presentation – Structure = normal – Function = poor vibratory coordination, poor vocal fold closure, ventricular compression, anterior - posterior compression EMG – normal Response to speech therapy – Excellent Compensatory MTD Onset – Laryngeal event (URI/Trauma/Surgery), aging process, compromised pulmonary status Progression – Consistent dysphonia including veg tasks – Some change over time is possible – Patient complains of increased effort and fatigue Compensatory MTD (cont.) Voice Quality – Breathy, diplophonia, glottal fry Acoustic Findings – Abnormal fundamental frequency – Yanigahara 1-4 – Variety of perturbation measures Compensatory MTD (cont.) Laryngeal Findings – Structure = normal – Function = poor vocal fold closure, posterior glottal gap, sluggish arytenoid movement, asymmetry VF vibratory characteristics EMG – Abnormal (Haglund, et. al. 10 of 18 “functional dysphonia” patients = abnormal EMG of CT and/or TA) Compensatory MTD (cont.) Response to speech therapy – Variable “unloading” tension may help diagnostic clarity and surgical result Usually underlying pathology (usually glottic insufficiency) needs to be addressed as well Contributory MTD Onset – gradual, after extensive vocal use, yelling, screaming, poor vocal hygiene Progression – No fluctuations – Worsens if not treated – Worsens with use – Patient complains of pain/fatigue/increased effort Contributory MTD (cont.) Vocal Quality – raspy, rough, breathy, normal prosody, increased rate, dysphonia consistent across task and environment, loud speech, hard glottal attacks, sustained phonation similar to speech Acoustic Findings – Normal to low Fo, restricted range (usually high restrictions), Yanigahara type 1-2, elevated perturbation Contributory MTD (cont.) Laryngeal Presentation – Structure = Pathology nodules, edema, posterior contact ulcers/granuloma, polyps – Function = vibratory restrictions, arytenoid movement well coordinated, posterior glottal gap, mild ventricular compression and/or mild anterior-posterior compression Contributory MTD (cont.) EMG – normal Response to speech therapy – variable Contributory MTD (cont.) Jiang and colleagues, 1998 Ann Otol Rhinol & Laryngol (107) – Computer modeling of laryngeal vibration Normal Tense (tension in TA) Nodule – Findings Intraepithelial mechanical stress increases at the midpoint of the membranous vocal folds under condition of muscular tension Describing Laryngeal Configuration Formerly MTD types 1-4 Use descriptive terms – PGG – Ventricular Compression – Anterior-Posterior Supraglottic Compression – Sphincteric Glottis Additional type: Thyroarytenoid Tension? Posterior Glottal Gap Considered a normal finding for many females Problematic when seen in conjunction with nodules or poor vibratory characteristics Describe extent of gap Ventricular Compression Mild - Severe Usually symmetrical Can be primary source of phonation Anterior-Posterior Supraglottic Compression Mild - Severe Normal finding at extremes of range for singers Best diagnosed with flexible endoscopy Normal for some vowels Sphincteric Glottis Both ventricular and AP compression View of vocal folds obscured Rare Usually Compensatory MTD or conversion MTD Clinical Application of Classification System Replace “Functional Dysphonia” with “Muscle Tension Dysphonia” Describe type of MTD as one of 4 types Describe glottic/supraglottic configuration Example – “Patient presents with habituated muscle tension dysphonia s/p URI as characterized by moderate ventricular compression” Diagnostic Considerations for MTD Intake Interview Perceptual Evaluation Acoustic Evaluation Aerodynamic Evaluation Medical Evaluation Videolaryngostroboscopy Laryngeal and cervical neck palpation Diagnostic Probes Intake Interview Special attention to . . . – – – – Onset Progression – previous treatment modalities Anxiety/stress factors and management Vocal load Tools – VHI (Jacobson) – Vocal Tract Discomfort (VTD) scale (Mathieson, et.al., 2009, J of Voice) Build rapport through unconditional positive regard; reflecting; listening; non-judgmental affect Vocal Tract Discomfort Scale (VTD) Mathieson, et.al., 2009 J of Vx Frequency of sensation/sympt. Burning 1 2 3 4 5 6 1 2 3 4 5 6 2. Tight 1 2 3 4 5 6 1 2 3 4 5 6 3. Dry 1 2 3 4 5 6 1 2 3 4 5 6 4. Aching 1 2 3 4 5 6 1 2 3 4 5 6 5. Tickling 1 2 3 4 5 6 1 2 3 4 5 6 6. Sore 1 2 3 4 5 6 1 2 3 4 5 6 7. Irritable 1 2 3 4 5 6 1 2 3 4 5 6 8. Lump in the Throat 1 1 2 1. 0 = never 2 = sometimes 4 = often 6 = always Severity of sensation/sympt 2 3 4 5 6 3 4 5 6 Intake Interview Common PT. complaints – – – – – – – – – Hoarseness Vocal fatigue Vocal strain Pain on or after phonation “Tightness” in throat Voice loss Unable to project Globus Loss of pitch range Perceptual Evaluation Visual tensions – jaw; forehead; SCM; larynx GRBAS scale Breath behaviors Glottal attacks, rate of speech, throat clearing, inappropriate intensity, fry tone, low pitch, Look for task specificity Perceptual Evaluation Perceptual worsening of dysphonia for SD for voiced vs. voiceless consonants; no change for MTD Perceptual worsening in SD from sustained /a/ to connected speech; MTD no change – Roy, el.al., (2007) Folia Phoniatric Logo and (2005) Laryngoscope Acoustic Evaluation Fo; MTD; Fo range; MDVP (jitter, shimmer and variation; degree of unvoiced signal) S:Z Spectrograph – ADSD vs MTD (Roy, et.al., Laryngoscope, 2008; Sapienza, et.al., 2000 J of Voice) – Phonatory breaks (complete interruption of phonation within a word) ADSD > MTD – SD – increase dysphonia with increase in task complexity MTD vs. SD (cont.) Spectrograms from ADSD vs MTD differenciated with 94% and 98% accuracy by SLP raters – Rees, et. al., (2007) Oto. HN Surgery Spectrograph: Diagnostic Tool ADSD MTD Aerodynamic Evaluation PAS – Subglottal pressure cmH2O Above NL – Glottal airflow mL/s Below NL – Estimated Laryngeal Resistance cm/H2O/L/s Above NL Medical Evaluation Contributions to MTD – Tissue sensitivity – Neurological abnormality – Pulmonary abnormality – Glottic insufficiency Common medical findings – GERD 49% – Allergies 37% Altman, et.al. 2005, J of Vx. N = 150 MTD Stroboscopy Glottic Configuration – Ventricular Compression – A-P supraglottic compression – Sphincteric glottis – PGG – Glottic constriction on inspiration (n=15 MTD; 15 controls) Vertigan, et.al., 2006, Laryngoscope Stability Stroboscopy (cont.) Other findings Paresis or paralysis VF atrophy Secondary lesions (location) Primary lesions Diagnostic Probes Stroboscopy (cont.) Pattern of Muscular Tension – Few aberrant laryngeal behaviors appeared unique for spasmodic dysphonia versus muscle tension dysphonia – Patterns of laryngeal tension did seem to differentiate – SD = intermittent; associated with phonetic variability – MTD = consistent from task to task Tremor only found with SD Leonard & Kendall, 1999. Laryngoscope Palpatory Evaluation Determine sites and levels of muscle tenderness, tension and resistance Hyoid and Larynx elevated Some cases larynx is forcibly depressed Larynx resists lateral displacement TH space constricted and painful to the touch (less so with ADSD) Submandible bulging/tight SCMs tight and tender Diagnostic Probes Laryngeal Relaxation Humming Vegetative Manip Tasks Psychogenic MTD Habituated MTD Compensatory MTD Contributory MTD Y N N Y Y Y Y Y Y N N N Y Y Y N Treatment for MTD Efficacious Differentiates SD from MTD 1 to 25 sessions of trp – More severe cases tend to need fewer sessions Treatment Protocol Medical management of irritation – Few cases of PPI curing MTD (Mesuda, et.al., 2007, Japanese journal with a big long name, n=3) Education/Counseling Direct therapy Education/Counseling Listen – Cue to relatable aspects of Pt. – Determine vocal intelligence – Establish open body language – Be prepared for tears Reassure – We do not think this is “in your head” Show Treatment Modalities Direct Therapy – Manual Circumlaryngeal Therapy (MCT) – LMRVT – Breath and Alignment Retraining – Auditory Masking – Biofeedback – Shaping from Vegetative Tasks – Estill Voice Training System MCT Goal: Relax excessively tense peri-laryngeal and laryngeal musculature inhibiting norm. phon. Massage = relax & reduce discomfort Based on Aaronson laryngeal musculoskeletal reduction approach (1990) circular movements made with thumb/finger applied to TH space from ant. to post. as well as over thyroid cart. Larynx coaxed side-to-side and down Vocalizations are coached and shaped to speech MCT Benefits shown in literature – Dcrs perceptual severity ratings – Dcrs perturbation values – Dcrs first three formants – Improved maximum phonation time – Roy and colleagues (1993, 1997 & 2001) MCT Dysphonia Severity Index reduced – DSI = weighted MPT, highest Fo, Lowest dB and jitter Van Lierde, et.al., in press, J of Voice. n=10 MTD. No change in Ab brthg tx grp. Also, Van Lierde, et.al., 2004, J of Vx. N = 4) MCT 111 female MTD pt. demo improved speech continuity (changes in VT) – diphthong 2nd formant slope increased – Vowel Space Area incrsd – Vowel Artic Index incrsd – Global speech rate incrsd – Dromey, et.al., 2008, JSLHR – Roy, et.al., 2009, J of Comm Dis. Laryngeal Massage Therapy Differs from CMT: – – – – T-H space not directly addressed Patient silent Patient’s rate VTD before and after Primarily bimanual Goal: reducing laryngeal height and hyperengaged supralaryngeal musculature Reduction of RAP and VTD severity and frequency (Mathieson, et.al., 2009, J of Voice. N = 10 MTD) Lessac-Madson Resonant Vx Tx (LMRVT) Cranial/facial sympathetic vibration MTD seems to prevent Works directly with filter Works indirectly with source Breath/Alignment Retraining Reduce cervical/neck tension – Abdominal, rather than cervical displacement during inhalation – Adjust alignment to head/neck (ears over shoulders) – Stretches – Self massage – jaw/larynx/SCMs – Improve breath flow Auditory Masking Disrupts auditory feedback loop Encourages return to normal muscular coordination Facilitator by Kay Elemetrics, SoundPro by Resound, audiometer. Biofeedback Surface EMG – Elevated peri-oral and peri-laryngeal EMG activity before and during phonation in MTD population (Hocevar - Boltezar, et. al. 1998) – Evidence that patients can reduce this activity using EMG biofeedback (Stemple, et. al. 1980) Phonatory Aerodynamic System Endoscopy – Improved “vocal intelligence” for some Vegetative Tasks Yawn Throat Clearing Coughing Gargle Grunt Giggle Sigh Cry Laughter Animal Sounds Hum Estill Voice Training System Jo Estill, Singer/Speech Pathologist Laryngeal and vocal tract positioning for different singing styles 11 manipulations – 4 source – 6 filter (pharynx, tongue, soft palate, aryepiglottic space) – False Fold Retraction Intervention Strategies by MTD Type Compensatory – Un-loading (LMT; RVT; Education; breath/alignment) Contributory – Un-loading (LMT; RVT; Education; breath/alignment) Psychogenic – MCT/LMT combo Habituated – MCT/LMT combo If Therapy Fails Reconsider Diagnosis Experimental techniques – Botox injection to ventricular folds – Lidocaine bath Referrals – – – – – – Otolaryngology Psychology Neurology Pulmonology Allergy Gastroenterology