Breast Pain and Nipple Discharge
advertisement

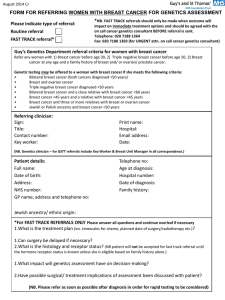
Breast Pain and Nipple Discharge Philip Turton Consultant Breast, Oncoplastic, and Aesthetic Breast Surgeon Leeds General Infirmary Mastalgia alone or in combination with lumpiness is the commonest reason for referral to a breast clinic Pain alone 17% Lumpiness and pain 33% Non painful lump 36% Nipple discharge 5% Family history 3% 50% Breast Pain Theory Imbalance of essential fatty acids Hormonal stimulation Endogenous sensitivity of some breast lobules Almost never associated with malignancy with normal examination Breast Pain Non breast mastalgia should be differentiated by a good history Consider: Angina, GS, Cervical spondylosis, Cervical rib, oesophageal erosions, lesions and achalasia, rib fracture, torn/strained muscle, pleuritic pain, pneumonia, pulmonary lesion, Tietz’s syndrome Non-cyclical pain Unrelated to the menstrual cycle Described as tight, burning or sore Constant or intermittent Usually affects one breast, in a localized area, but may spread more diffusely across the breast Usually affects postmenopausal women in their 40s and 50s Cyclical Breast Pain Clearly related to the menstrual cycle Described as dull, heavy or aching Often accompanied by breast swelling or lumpiness Usually affects both breasts, UOQs, +/- radiates to axilla Intensifies during the two weeks leading up to the start of your period, then eases up afterward Usually affects premenopausal women in their 20s and 30s and perimenopausal women in their 40s Mastalgia: Taking a good history Age, FH, parity Previous history of breast problems: cysts, pain, biopsies, cancer, surgery (BBA, BBR, mastopexy) Previous breast imaging- what, why and when When was last period? Menstrual irregularities Usage of OCP, depot, mirena coil, progesterone only pill Breast Pain Assess the pain: pain chart if not straightforward Site, type, intensity, duration of symptoms frequency previous occurrence Current impact on QOL Specific concerns eg cancer FIGURE 3.1 Back to Chapter 3 thumbnails Back to Contents FIGURE 3.2 Back to Chapter 3 thumbnails Back to Contents Examination NB: re-examine after next period if presenting in the week prior to menstruation Examination: Mirror signal manoeuvre!! Examination: Mirror signal manoeuvre!! Examination: Mirror signal manoeuvre!! Who can be managed initially in primary care Bilateral symmetrical cyclical pain, which resolves following menstruation Recent onset breast pain, with normal examination in young patient Male patients with simple tender gynaecomastia Normal examination and recent normal breast imaging If in doubt, please refer Treatment Educate and Reassure Refit bra if obvious problem/ sports bra helps in short term Topical NSAID gel Avoid caffeine completely Evening primrose oil: 1gm od or BD for minimum of 3-months, with good compliance If on HRT- reduce If recently started COCP - reassure If mirena/prog only pill, consider other Breast Pain Who to refer: “anything atypical” 1. Pain associated with definite signs: eg dominant or discrete lump, palpable focal thickening: will have triple assessment 2. Patients who have previously had breast cancer Rib met, lung met, LR 3. Persisting pain, same quadrant for 3months Mammo + targetted USS normal or B9 changes carries almost 100% Hospital Treatment of Severe Mastalgia Tamoxifen 10-20mg OD, 4-months Use on days 5 to 21 of cycle most effective S/E hot flushes, vaginal dryness Very rare: DVT Treatment Danazol 100mg tds, 4-months Inhibits pituitary gonadotrophins (FSH & LH) Stimulates androgenic pathways S/E: acne, oily skin, hirsuitism, weight gain, voice change, thrombosis Treatment Bromocriptine 2.5mg OD, 4-months Stimulates dopamine receptors in the brain and inhibits release of prolactin Avoid in post-partum period (MI, CVA, HT) S/E drowsiness, headache, postural hypotension, nausea, dizziness, dry mouth, fibrotic reactions Treatment GnRH analogues, Decrease FSH/LH (after initial surge) S/E: Hot flushes, sweating, vaginal dryness, loss of libido Breast Pain Treatment of non-cyclical breast pain Usually as for cyclical More likely to use oral NSAID early on Often due to duct ectasia; more common after menopause Is there a chance that cancer can be present? Rare in absence of palpable thickening, or lump. Ensure breast looks & feels normal, and no obvious palp LN Repeat examination after 6-weeks Questions? Nipple Discharge Causes Physiological Duct ectasia Mild inflammation Post-partum Papilloma DCIS, Inv ca Abscess Very rare: endocrine cause, joggers nipple Papillomas and duct ectasia commonly arise in the sub areola segment Duct ectasia An aberration of development & involution Women >50 Nipple discharge, retraction, doughy palpable mass Discharge cheesy/ white Slit-like nipple retraction Management conservative or surgical Surgical = total duct excision Nipple Discharge Taking a History When Spontaneous, or on Squeezing Frequency & duration Consistency & quantity: spotting on bra, or staining through to blouse Blood stained Current medication: phenothiazines, haloperidol, methyldopa Colour Usually always insignificant: multi-duct Brown and haem negative Green White, creamy Investigate: single duct Brown and haem negative but persistent Brown and haem positive Serous Blood stained Galactorrhea NB: Use the standard urinalysis sticks History Associated breast symptoms or signs Any lump Any changes near the NAC Nipple inversion, nipple eczema Adjuncts to assess risk Parity FH of breast or ovarian ca Previous breast problems, abnormal breast biopsies For galactorrhea: amenorrhea/headache/visual Examination Apart from the nipple discharge, examination is usually normal Look for the rarely associated signs of a sinister cause Indrawing, lump, sub-areola thickening Investigation of new nipple discharge Advise to cease expression Mammogram/USS if persists Review in 2-3 months If persistent bilateral, do serum prolactin Investigate further in breast clinic Investigation Nipple fluid: haem test If positive do Hadfields procedure Nipple fluid: smear onto a slide for cytology Epithelium should not be seen ie should be “negative for epithelial cells” If positive for epithelial cells indicates higher possibility of papilloma or DCIS, therefore do Hadfields procedure to send tissue to pathologist Investigation >35: Mammo and USS of NAC <35: USS of NAC Guided biopsy Eg USS guided core or FNAC of ?intraduct papilloma NB: Any clinically palpable lump must always be biopsied even if mammo and USS are normal Treatment Diagnostic Surgery Uncommon: microdochotomy/Ductoscopy “Hadfield’s Procedure” Sub areola excision of the major breast ducts, which is sent for histology S/E: nipple sensation, nipple necrosis, infection Therapeutic operation Where results of Hadfields procedure show DCIS/Inv ca: Usually mastectomy & IBR Treatment of non-significant nipple discharge Advise not to squeeze the nipple to look for further discharge If persists and is nuisance can refer for further investigation Would tend to do a therapeutic Hadfields Ie the purpose is to stop the discharge with the operation instead of doing it for diagnostic assessment alone Key Points Breast Pain: Most do not need referring, reassure, educate Refer: not settling, focal nodularity, lump Nipple Discharge: Most are physiological or duct ectasia Refer: watery or blood stained Handouts: please email me on eplt@aol.com Any breast related queries: philip.turton@leedsth.nhs.uk NHS secretary: Angela Mathie: 0113 3922250 Spiculate mass right breast Normal left breast USS of Right Breast Cancer, and USS core, confirming needle through lesion MRI of Right Breast Cancer, revealing multifocality Biopsy: The Mammotome Handouts: please email me on eplt@aol.com Any breast related queries: philip.turton@leedsth.nhs.uk