C19_Michael Barrington
advertisement
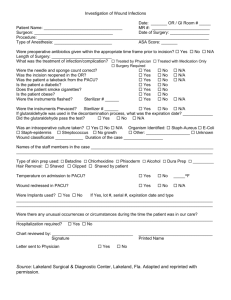
Regional Anaesthesia Techniques for DaySurgery CSM 2011 Dr Michael Barrington Department of Anaesthesia St Vincent’s Hospital, Melbourne Attributes of the ideal anaesthetic for day-surgery High quality analgesia low pain score low incidence of side-effects long duration Efficient Patient acceptance Range of techniques available Central neural blockade (CNB) Peripheral nerve blockade (PNB) Local infiltration analgesia (LIA) CNB and PNB result in: decreased pain scores in PACU decreased requirement for PACU analgesia CNB was not associated with decreased PACU time with reduced nausea Ambulatory Surgical Unit (ASU) discharge was increased by 35 mins Peripheral Nerve Blockade increased ability to bypass PACU (OR14) decreased PACU time (24 mins) decreased risk of nausea (OR 0.17) increased patient satisfaction not associated with decreased discharge ASU Entire diamond lies to the right of line, RR = 1, indicating that ultrasound guided blocks are more likely to be successful Shoulder surgery Ambulatory shoulder surgery Ultrasound-guided techniques: interscalene (n = 515) supraclavicular (n = 654) blocks Pain score (VAS) in PACU 0/10 Need for IV analgesia in PACU 0.6% Time in PACU 168 mins Body mass index 22 kg/m2 Volume of local anaesthetic 50 mls Hospital for Special Surgery Side-effects/complications Hoarseness 26% Dyspnoea 8% Pneumothorax 0% LA toxicity 0% The role of Ultrasound Low dose efficacy studies (both single shot and continuous infusions) Dose reduction Severe hypotension following interscalene block Bilateral upper limb block in PACU Differential diagnosis: Bezold-Jarisch reflex Anaphylaxis Intrathecal spread Epidural spread Hand surgery Infraclavicular block (ICB), chloroprocaine compared with GA (LMA, desflurane) and wound infiltration in RCT PACU nurses “blinded” to technique scored patients for readyness for PACU discharge 76% of patients who received ICB met criteria for PACU bypass compared to 25% in the GA group None of the patients in the ICB group requested pain medication in hospital compared to 48% in the GA group Patients receiving ICB were able to ambulate earlier 82 min vs 145 min with GA Results from St Vincent’s Hospital, Melbourne Data obtained from 933 patients (received 1216 PNBs) Median (worst) pain score 1.1 Most common pain score 0 757 (81%) required no analgesia in PACU Average time to readiness for discharge 25 mins 464 (50%) achieved discharge criteria on PACU arrival Breast surgery Unilateral breast surgery without reconstruction Randomised to single-shot paravertebral block (PVB) or continuous (PVB) 0.1 %, 0.2% or saline infusion for 48 hrs Validated pain assessment instruments including McGill Pain Questionnaire No clinically significant difference in: degree of postoperative pain Nausea Mood state Level of symptom distress Return to normal activity Patients having unilateral breast surgery without reconstruction were randomised to receive either GA alone or combined GA and PVB Multilevel blocks T1 - T6 PVB Ropivacaine 5mg/kg + Adrenaline (350mg maximum) was used Pain was study endpoint Pain scores were lower following PVB at one hour and at three hours, but not at later time points Pain scores were higher in PVB at 24 hrs compared to GA alone Hernea surgery Inguinal hernea repair Randomised to GA or paravertebral blockade Patients randomised to paravertebral blockade had improved outcomes including analgesia and recovery Inguinal hernea repair Randomised to transversus abdominis plane block or conventional ilioinguinal/ileohypogastric nerve blocks (n= 273) Ultrasound techniques: Reduced pain scores at 4, 12 and 24 hours No difference in PACU, Postoperative day 1 or thereafter Wound infiltration • 1. Single injection wound 2. Continuous local anaesthetic wound infusions • • • 3. High volume local anaesthetic wound infiltration Need for procedure specific randomised controlled trials • • 1. Single injection wound 2. Continuous local anaesthetic wound infusions • • 3. High volume local anaesthetic wound infiltration Need for procedure specific randomised controlled trials Wound infiltration Efficacy should be procedure specific Single injection of local anaesthetic at completion of surgery reduce analgesia - short duration only Choice of local anaesthetic important Catheter type Adjuvants Note anatomical location of infiltration Sites of wound catheter placement Intraperitoneal Intraarticular Subfascial Subcutaneous Intrapleural Substernal Knee Arthroscopy One of the most common lower limb ambulatory surgical procedures Multitude of intraarticular agents used for postoperative analgesia (opiates, NSAID, local anaesthetics) Peripheral blocks Four groups: 0.9 % saline, bupivacaine 0.25%, ropivacaine 0.2%, ropivacaine 0.75% No difference within LA groups 40% of patients receiving placebo had motor block Low dose (4 - 5 mg) compared with intermediate dose and high dose (10 - 15mg) Low dose requires unilateral positioning of patient Associated with reduced discharge times Ambulatory arthroscopic surgery of the knee Spinal anaesthesia Randomised to prilocaine 20 mg or plain bupivacaine 7.5 mg In summary Wide range of regional techniques available for ambulatory techniques Large number of studies supporting these techniques for various surgical procedures Efficacy vs effectiveness vs cost-effectiveness in our own practice is important In summary Evidence supports PNB upper limb surgery Choice of ideal regional anaesthesia technique for ambulatory trunk surgery unclear RA for ambulatory lower limb surgery is a challenge - motor block Thank you for your attention