Therapeutic Apheresis in Neurological Disease
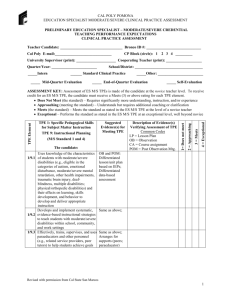
advertisement

The Role of Therapeutic Apheresis in Neurological Disorders Vishesh Chhibber, MD November 15, 2013 Disclosure • I have no actual or potential conflict of interest in relation to the content of this presentation The Role of Apheresis • Several autoimmune neurological disorders can be treated with TA • Usually a protein in the plasma (often an autoantibody) is being removed • Most common procedure performed is TPE – Immunoadsorption (IA) is also utilized • In some disease indications, it is not clear why TPE is beneficial Evidence Based Guidelines • The American Academy of Neurology (AAN) published updated evidence-based guidelines in 2011 • ASFA published the 6th edition of their evidence based guidelines in 2013 AAN Guidelines • Previous AAN assessment was in 1996 • Controlled clinical trials (in humans) • Data from observational studies and case reports was not included in the analysis as this was considered class IV evidence Cortese I et al. Neurology 2011;76:294-300 ASFA • Previous ASFA guidelines were published in 2010 • Considered all published evidence (including observational studies and case reports) • Assigned a category and a recommendation grade for each indication Schwartz J et al. J Clin Apher 2013;28:145-284 Schwartz J et al. J Clin Apher 2013;28:145-284 Schwartz J et al. J Clin Apher 2013;28:145-284 Disorders that will be discussed today Schwartz J et al. J Clin Apher 2013;28:145-284 Technical Details of TPE • 1-1.5 Plasma volumes • Albumin (5%) used as the replacement fluid • Donor plasma added as a portion of the replacement fluid if patient at risk of coagulopathy/bleeding (e.g. daily TPE) • Number and frequency of TA procedures will depend on the disease/indication Acute Disseminated Encephalomyelitis (ADEM) • Acute inflammatory demyelinating disease of the CNS • Immune response to myelin (or other autoantigens) • Presents with acute encephalopathy – altered mental status, hemiparesis, ataxia, motor deficits, may progress to coma Acute Disseminated Encephalomyelitis • Usually – monophasic – seen in children and young adults – lasts 2-4 weeks – follows a viral infection or a vaccine • Lesions in subcortical region with sparing of periventricular areas – Resolution of lesions on repeat MRI (complete or partial) Therapy • Corticosteroids (first line therapy) – 1/3 fail • In patients that do not respond to steroids, TPE or IVIG can be used – 3 to 6 TPE with 1-1.5 volume replacement using 5% albumin performed daily or every other day • In patients that respond to TPE, improvement is noted soon after initiation of TPE Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN: Possibly effective in acute CNS demyelination (includes MS, ADEM, and NMO) if steroid therapy fails • ASFA: Category II with a recommendation of 2C Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Neurological Disease Conditions CNS PNS Acute ADEM AIDP (Guillain-Barre) Chronic MS NMO CIDP MG Acute Inflammatory Demyelinating Polyneuropathy (Guillain-Barre Syndrome) • Most common general paralytic disorder • Acute motor and sensory deficiency involving the peripheral nerves • Caused by a complement binding IgM antibody to peripheral nerve myelin • RCT’s have shown – Less time to recovery – Greater extent of neurological recovery The GBS Study Group. Neurology 1985;35:1096 -1104 French Coop. Group on TPE in GBS. Ann Neurol 1987;22:753-761 Therapy • TPE is considered first line therapy – 5 or 6 TPE with 1-1.5 volume replacement using 5% albumin performed every other day – Exchange 200-250 mL of plasma per Kg over 10-14 days • Alternatively IVIg may be used with similar efficacy – higher cost – may not be as effective in patients with axonal involvement Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN: TPE is effective in severe AIDP (impaired ability to walk, requirement of mechanical ventilation) and should be offered to these patients. In milder disease, it is probably effective and should be considered. • ASFA: Category I with recommendation grade of 1A – Category III with a recommendation grade of 2C has been assigned for TPE post IVIG Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Neurological Disease Conditions CNS PNS Acute ADEM AIDP (Guillain-Barre) Chronic MS NMO CIDP MG Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) • Chronic autoimmune demyelinating disease of the peripheral nervous system • Symmetric sensory loss and muscle weakness • Progressive or Relapsing course • Believed to be an autoimmune disorder but the pathogenesis is not fully understood Therapy • Improvement seen with immunomodulating and immunosuppressive therapy • Corticosteroids, TPE and IVIg have been used • 60-80% respond to initial therapy • Response to therapy is short lived (improvement often wanes after about 2 weeks) • Therapy should be initiated early to prevent inflammatory demyelination and axonal degeneration Therapy • TPE performed 2-3 times per week until improvement is noted – 1-1.5 volumes using 5% albumin – Taper TPE as tolerated to a maintenance schedule – Maintenance frequency varies between patients (weekly to monthly) • Alternatively IVIg may be used with similar efficacy • Corticosteroids may be used for maintenance (after initial therapy with TPE) Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN: TPE is effective in CIDP and should be offered as short-term therapy • ASFA: Category I with recommendation grade of 1B Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Multiple Sclerosis (MS) • Relapsing/progressive CNS disorder that presents in early adulthood • Pathogenesis not fully understood – believed to be an autoimmune disorder that involves both the cellular and humoral immune systems and results in white matter demyelination – oligoclonal bands in the CSF • Heterogenous with variable prognosis Multiple Sclerosis (MS) • Presents with sensory deficits, diplopia, optic neuritis (unilateral), extremity weakness, bowel/bladder symptoms • Several patterns of disease: relapsingremitting, chronic progressive (primaryprogressive, secondary-progressive, progressive-relapsing) Therapy • High dose corticosteroids • In patients with severe acute MS without response to steroids, consider TPE – 5 to 7 TPE with 1-1.5 volume replacement using 5% albumin performed over 14 days • Other disease modifying therapies include: interferon beta-1a, glatiramer acetate, IVIG, rituximab, cyclophosphamide, azathioprine, mitoxantrone, natalizumab Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN: Possibly effective in acute CNS demyelination (includes MS, ADEM, and NMO) if steroid therapy fails • ASFA: Category II with a recommendation of 1B in acute CNS demyelination – Category III with a recommendation grade of 2B has been assigned for chronic progressive MS Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Neurological Disease Conditions CNS PNS Acute ADEM AIDP (Guillain-Barre) Chronic MS NMO CIDP MG Neuromyelitis Optica (NMO) • Aka Devic’s disease (Previously considered a form of MS) • Women are affected more commonly • Typically, patients are in their 30’s but seen at all ages • Autoimmune disorder that results in inflammatory demyelination of the CNS • Primarily involves the spinal cord & optic nerve Neuromyelitis Optica • Progressive disease – Incomplete recovery after each relapse leads to residual deficits – 5 years: 30% mortality and 50% are wheelchair bound or have severe visual deficits • Recently associated with an IgG autoantibody to aquaporin-4 (a water channel found on the foot processes of astrocytes) – aka NMO-IgG Lennon et al. J Exp Med 2005;202:473-477 NMO Diagnostic Criteria Wingerchuk et al. Neurology 2006;66:1485-1489 Therapy • High dose corticosteroids (first line therapy) • TPE is initiated if no improvement or progression after steroid administration – 5 TPE with 1-1.5 volume replacement using 5% albumin performed daily or every other day • More likely to see benefit if TPE is initiated early in the course Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN: Possibly effective in acute CNS demyelination (includes MS, ADEM, and NMO) if steroid therapy fails • ASFA: Category II with recommendation grade of 1B in acute NMO – Category III with a recommendation grade of 2C has been assigned for maintenance therapy Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Myasthenia Gravis • Autoimmune disorder that results in disruption of neuromuscular transmission • Antibody to the acetylcholine receptor on the post synaptic motor end plate • Results in muscle weakness – Extraocular and bulbar – Generalized (trunk and extremities) Therapy • Cholinesterase inhibition – e.g. pyridostigmine – Stronger action potentials of the muscles • Corticosteroids and azathioprine for immunosuppresion • Surgical thymectomy – Beneficial if thymoma present • TPE TPE • TPE used in moderate/severe cases or prior to thymectomy – 1-1.5 volumes with replacement using 5% albumin • The number and frequency of TPE depends on the patient’s disease • Induction with 225 mL/kg over 1-2 weeks • Long-term maintenance may be required Schwartz J et al. J Clin Apher 2013;28:145-284 Guidelines • AAN – “There is insufficient evidence to support or refute the use of plasmapheresis for myasthenia gravis” • ASFA: – Moderate-severe disease: Category I with a recommendation grade of 1B – Prethymectomy: Category I with a recommendation grade of 1C Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Discrepancy between AAN and ASFA • ASFA reviewed all of the published evidence • AAN did not consider evidence from observational studies or case reports – “…reexamination of the methodologies may be warranted due to the failure, in some cases, to account for overwhelming anecdotal evidence or evidence from uncontrolled studies. Thus it may be the case that Class IV evidence should be considered when it is both abundant and consistent, especially when higher standards of evidence cannot feasibly be obtained for either ethical or other reasons” http://www.neurology.org/content/76/3/294/reply#neurology_el_42491 Natalizumab • Used to treat relapsing-remitting MS • Monoclonal antibody against α4-integrin – Entry of WBC into the CNS • PML is a life threatening complication of natalizumab therapy – Opportunistic CNS infection by the JC virus Natalizumab Clearance • Natalizumab has a long half life & may be detectable >12 weeks after the last dose • TPE has been used to hasten the removal • May provide significant benefit by restoring ability of WBCs to enter the CNS – TPE decreases the drug levels and T ½ – Shorter time to immune reconstitution – Clinical improvement Khatri et al. Neurology 2009;72:402-409 Guidelines • AAN – Initial data suggests TPE may be useful in restoring leukocyte function by removal of natalizumab – Additional studies are necessary to see whether this results in any benefit in patients with infectious complications • ASFA: Category III with a recommendation grade of 2C Cortese I et al. Neurology 2011;76:294-300 Schwartz J et al. J Clin Apher 2013;28:145-284 Adverse Consequences of TPE • Immune Reconstitution Inflammatory Syndrome (IRIS) – Inflammatory response – Symptom exacerbation – Enlargement of MS lesions • IV Corticosteroid therapy may be of benefit Schroder et al. Arch Neurol 2010;67:1391-1394 Additional Use of TPE in Natalizumab Clearance • Natalizumab is usually used as monotherapy • Alternate therapy may be necessary if MS patient is not responsive to natalizumab • Adding a second immunosuppressive therapy may place patient at increased risk of infection • Neurologists may request TPE to hasten clearance prior to initiating another drug Summary • TPE plays an important role in the treatment of several autoimmune neurological disorders • Therapy should be based on evidence based review of the literature • The AAN and ASFA have published evidence based guidelines regarding the use of TA • Additional studies are necessary to determine the optimal role of TA in several neurological disease conditions Questions?