Stroke, CVA, Aphasia PowerPoint ALS-ILS-BLS

Stroke, CVA and Aphasia
Silver Cross EMS System
July 2012 Continuing Medical Education
Written and Presented by: Leslie Livett RN MS
Provena Saint Joseph Medical Center
Acknowledgements
• Northwest Community EMS System
• EMS Region 8 CME comittee
• Jamie Rademacher, RN, Stroke Coordinator, Silver Cross
Hospital, New Lenox, IL
• Leslie Barna RN MSN CNRN Stroke Coordinator, Provena Saint
Joseph Medical Center, Joliet, IL
• National Aphasia Association
• Reid Hospital and Healthcare Services, Richmond, IN
• Brookfield Police Department
Objectives
• Review brain anatomy, physiology and vascular supply
• Review difference between ischemic/thrombotic and hemorrhagic stroke
• Review signs and symptoms of stroke and highlight differences in special populations
• Review Region 7 Standard Operating Procedures for stroke
• Discuss aphasia as related to stroke/CVA and field implications
• (ALS only) Strip O’ the Month: Prolonged QT intervals and
Torsades
Stroke, aka Brain Attack
• A sudden, catastrophic event
• Focal neurologic impairment
• Most often caused by occlusion or rupture of an artery that supplies a specific region of the brain
Statistics
• In the US, almost 800,000 people suffer new or recurrent strokes each year (ASA, 2009)
– 55% die or survive disabled
• 3rd leading cause of death in developed nations (behind heart disease and cancer)
• $68.9 billion cost of treatment and disability (2009)
• Death / Disability rates higher in African-Americans
• 60% of strokes happen to males
• Strokes in females more likely to be fatal
• Most preventable of catastrophic conditions
Lifestyle Risk Factors
• Tobacco use
• Obesity, elevated cholesterol, elevated lipids
• Physical
• Excessive alcohol intake
• Use of illegal drugs, particularly cocaine in any form or any injected drug
Barriers to Stroke Care-Why?
• Knowledge
• Financial
• Educational needs
• Ethics
• Research
• Man power
“TIME IS BRAIN”
• 2 million
brain
cells dying every minute
• Public doesn’t understand that strokes are nearly “curable” if transport happens quickly
A & P Review - Lobes
• Cerebrum
– Largest, most developmentally advanced
– Higher functions
• Cerebellum
– Balance, movement, coordination
• Brainstem
– Final pathway between cerebral structures and the spinal cord
– Automatic functions (respiration, heart rate, blood pressure, wakefulness)
A & P Review - Layers
• Gray matter
– aka cerebral cortex
– 20 mm thick (3/4”)
– Contains centers of cognition, personality and complicated movements
• White matter
– Network of fibers that enable the regions of the brain to communicate with each other
A & P Review – Control Centers
Circle of Willis
• Actually the Oval of
Willis
• Joins the two systems before they enter the brain
• When either system is blocked, collateral circulation may occur through this loop
Major Brain Arteries
Anterior Cerebral Artery Middle Cerebral
Artery
Posterior Cerebral Artery
Classification of Stroke
Ischemic – Embolic
• Partial or complete blockage of a cerebral artery from embolic material,
– generally composed of cholesterol, plaque, blood, air, or tumor tissue that migrates to the brain
• Often occur without warning
• Symptoms may fluctuate
– due to continuing movement of the embolic matter within the blood vessel
Hemorrhagic - Subarachnoid
• Aneurysms, arteriovenous malformations and other vascular hematomas may bleed
– producing a subarachnoid hemorrhage
• Especially prevalent in 35 to 65-year-olds
• Accounts for ~ 7% of all strokes
Hemorrhagic – Intracerebral (ICH)
• Small, deeply penetrating arteries in brain tissue susceptible to loss of elasticity in chronic htn
• The expanding mass of blood can grow to the size of a golf ball or larger
– Can project 2 to 3 cm into the brain tissue
• The mass causes pressure on cerebral tissues and nerves
– leading to death of neurons
• The hematoma can disturb normal intracranial dynamics
– causes a sudden rise in intracranial pressures
Transient Ischemic Attack
• “mini-stroke” or TIA
• Defined as transient focal brain ischemia without radiologic evidence of infarction
• TIA a strong indicator of possible future stroke
– American Stroke Association guidelines recommend approaching TIA with the same urgency as stroke
• 15% of strokes preceded by a TIA ignored by patients
• After TIA, 12% experience stroke within 30 days, and up to
17% within 90 days
– 25% of TIA patients die within a year
Signs and Symptoms
• Carotid Region
– visual disturbance (ophthalmic artery)
– Contralateral motor or sensory deficits to face or limbs (MCA/ACA)
– Aphasia (MCA)
– Homonymous hemianopsia (MCA)
• Vertebrobasilar Region
– nausea/vomiting
– dysphagia/dysarthria
– dizziness/vertigo/gait disturbance/ataxia
– numbness/weakness of face
– nystagmus
– ”Locked-in” syndrome
• quadriplegia/weakness face and pharyngeal muscles
Key Concept for EMS
• WHEN WAS THE PATIENT LAST SEEN
NORMAL?!
– If at all possible, pin down the time of the attack
Note: BLS and ALS stroke SMO’s are nearly identical, due to not wanting to waste time in transport
Stroke Assessment
Differential Diagnosis of Stroke
• Seizure
• Complicated migraine
• Mass lesion
• Demyelinating disease
• Inflammation
• Hypoglycemia
Diagnostic Studies (in hospital)
• Non-contrast CT brain or MRI
• Blood glucose
• Serum electrolytes/renal function
• ECG
• Cardiac enzymes
• PT/PTT/INR
• Oxygen saturation
Stroke in Special Populations
• Women
– Stroke kills twice as many women as breast cancer every year
– Women can have unique stroke symptoms
– Face and limb pain
– Hiccups
– General weakness
– Nausea
• Young people and children
– CDC notes increased risk of stroke among younger population including children and teens
– Young adults with stroke are often misdiagnosed
– Majority of cases are mistaken as inner ear disorder; also alcohol intoxication, migraine, and vertigo
Extended IV t-PA Window to 4.5 hours
• Used to be 2-3 hours before patient couldn’t get t-PA anymore.
• But American Stroke Guidelines expanded IV t-PA window in May 2009
– For certain candidates
• ADDITIONAL IV t-PA EXCLUSION CRITERIA FOR 3-4.5
HRS
-Over 80 years old
-NIHSS > 25
-History stroke and diabetes
-On any Oral anticoagulation
Endovascular Procedures
• Neuro Endovascular Surgeon
• Neuro Endovascular suite
• IA-t-PA
• Clot retrieval device
• Goal: recanulazation of vessel
Pre Post
• 1 min. of brain ischemia can kill 2 million nerve cells and 14 billion synapses
• IMPORTANT !
1. Patients need to access 911 as soon as symptoms are recognized
2. EMS must rapidly assess patients and recognize stroke
3. EMS must notify receiving facility ASAP so Stroke Team can be activated
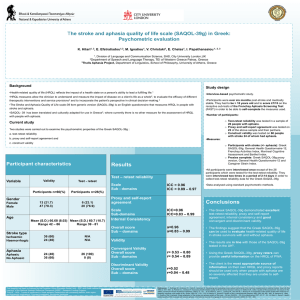
APHASIA
Objectives
• What is Aphasia
• Stroke and other causes of Aphasia
• How do you communicate with a patient with
Aphasia
• EMS implications
• Community Resources
What is Aphasia
• Aphasia is an impairment of language.
– An acquired communication disorder that impairs a person’s ability to process language, but does not affect intelligence.
• Impairs ability to speak and understand others.
– Most people with aphasia experience difficulty reading and writing.
Types of Aphasia
• Global Aphasia – Most severe form
– Produce few recognizable words
– Understands little or no spoken speech
– Can neither read or write
• Usually patient has suffered a stroke
• May rapidly improve if the damage has not been too extensive.
• Greater brain damage, more severe and lasting disability.
Types of Aphasia
• Broca’s Aphasia – speech output severely reduced
– Limited mainly to short utterances, less than four words
– Vocabulary access limited
– Formation of sounds laborious/clumsy
– May read and understand speech, but can’t write.
– Halting and effortful quality of speech
Types of Aphasia
• Mixed non-fluent aphasia-
– Sparse and effortful speech resembling Broca’s
– Limited in comprehension of speech
– Patients do not read or write beyond an elementary level
Types of Aphasia
• Anomic Aphasia – inability to supply words for things.
– Significant in nouns and verbs
– Understand speech well, read adequately
– Poor writing ability
What causes Aphasia
• Most common cause of aphasia is stroke
• About 23 – 40% of stroke survivors acquire aphasia.
• Estimated one million people in US have acquired aphasia, or 1 in 250 people.
What causes Aphasia
• More common than Parkinson’s Disease, cerebral palsy or muscular dystrophy.
• About 1/3 rd of severely head-injured persons have aphasia.
Recovery from Aphasia
• After stroke – If symptoms last longer than 2-3 months, complete recovery is unlikely
– People continue to improve over a period of time
– Slow process for both patient and FAMILY
– Need to learn compensatory strategies for communicating
EMS Do’s and Don’ts
• Do not immediately assume aphasia patient is drunk or mentally ill/challenged.
• Always check blood sugar, just in case.
• Talk to patient as an adult, not as a child
• Minimize or eliminate background noise
• Use all modes of communication
– Speech/writing/drawing/yes-no responses
Communication
• Give them time to talk and permit a reasonable amount of time to respond
• Accept all communication attempts
• Keep your own communication simple but adult
• Simplify sentence structure and reduce your rate of speech
Communication
• Keep your voice at a normal level and emphasize key words
• Augment speech with gesture and visual aids when possible
• Repeat statements when necessary
• Do not attempt to finish the patients statement for them
Resources
• Windshield / Window sticker
– Part of national campaign
– Patient places sticker in the left rear passenger side of car
– For home, placed at front or rear entrance
Silver Cross EMS Strip o’ the Month
• Prolonged QT intervals and Torsades de
Pointes
QT INTERVAL and
TORSADES de POINTES:
Today’s patients receive the benefit from many advances in medical technology and research.
Among those benefits are multiple new drug therapies.
QT INTERVAL and TORSADES de POINTES:
However, along with these new drug therapies come inherent new risks.
QT Interval and Stroke
• Atrial Fibrillation is a rhythm more associated with risk of stroke (as we learned last month)
• But prolonged QT intervals are the rhythms more often seen after strokes
• Research does not yet show if this is due to the type of stroke, or cardiac output changes after strokes.
QT INTERVAL and
TORSADES de POINTES:
Prolonged QT intervals make patients more prone to a potentially fatal form of polymorphic ventricular tachycardia called:
Torsades de Pointes
QT INTERVAL and
TORSADES de POINTES:
Translated from French: “twisting of the points”
QT INTERVAL and
TORSADES de POINTES:
“Polymorphic” means it assumes multiple shapes.
The tachycardia varies in size and shape and gives the appearance of twisting around the isoelectric baseline.
QT INTERVAL and
TORSADES de POINTES:
• The patient may have no pulse or blood pressure and may need to be defibrillated immediately.
• But other times, the rhythm spontaneously converts before loss of pulse or blood pressure occurs.
– Or even before EMS arrival
QT INTERVAL and
TORSADES de POINTES:
These patients may simply present with complaint of fainting spells at home.
Or there may be a long family history of sudden, unexplained death, especially among young people.
QT INTERVAL and
TORSADES de POINTES:
May be caused by factors that prolong the QT interval.
Among these factors are
– heredity
– electrolyte disturbances
– myocardial ischemia
– stroke
– bradycardia
– drug therapy
• Drug Induced
– Antidepressants
– Phenothiazines
– Antiarrhythmics
• Pronestyl
• Amiodarone
• Corvert
• Electrolye imbalance
– Low Magnesium
– Low Potassium
– Low Calcium
– Also Insecticides
QT INTERVAL and
TORSADES de POINTES:
• Eating disorders
• Hereditary (prolonged QT syndrome)
– 1/3 asymptomatic
– Suspect if hx. Fainting
– Triggers
• emotional excitement
• exercise
• being startled
• anger
• test-taking
• stressful situations
This is a very abbreviated list of drug classifications that may cause prolongation of the QT interval.
A longer list is available from pharmacy and various web sites.
QT INTERVAL and
TORSADES de POINTES:
“HOW do I monitor QT interval?”, you may ask.
QT Interval
•
Measure from beginning of q wave to where the t wave returns to baseline.
•Q wave is first downward deflection after P.
•If no Q wave, start at first upward deflection after P.
• S hould be less than
50% of R-R interval.
•
If > 50% of R-R interval: risk for Torsades de
Pointes !
QT INTERVAL and
TORSADES de POINTES:
• The acceptable length of QT interval varies according to many factors.
• The biggest factor is heart rate.
– Slower heart rates have longer QT’s. This doesn’t necessarily mean there is a problem.
QT INTERVAL and
TORSADES de POINTES:
Measuring the QT pre-hospital
• 12 lead monitors will inform you when the QT interval is prolonged.
– When you print out the 12-lead, it will be included in the notes.
• Sometimes just by eying it you can see when it’s too long
• Or if you want to have some fun, locate a laminated QT to QTc conversion chart online or in the ED.
Treatment
• If patient is pulseless and apneic, treat as regular v-tach.
– CPR, shock and drugs
• There is no SMO for
Torsades
– But medical control may ask ALS providers to give
Magnesium in addition to other resuscitation drugs if indicated.
• If patient is awake and
Torsades is intermittent, treat the symptoms
(dizziness, weakness, syncope, etc) as you normally would.
• Again, ALS providers may be asked to give patient Magnesium.
QT INTERVAL and
TORSADES de POINTES:
SUMMARY
• Many drugs, stroke history, heredity and other conditions can cause the QT interval to prolong.
• Torsades de Pointes may result, causing death.
• Measuring and trending QT interval will help prevent this complication from occurring.
Thank you!
• THANK YOU FOR YOUR ATTENTION
• Feel free to email afinkel@silvercross.org
with questions for Leslie or any other questions.
• If you are watching this live, you can also type your questions in the text box to the right!