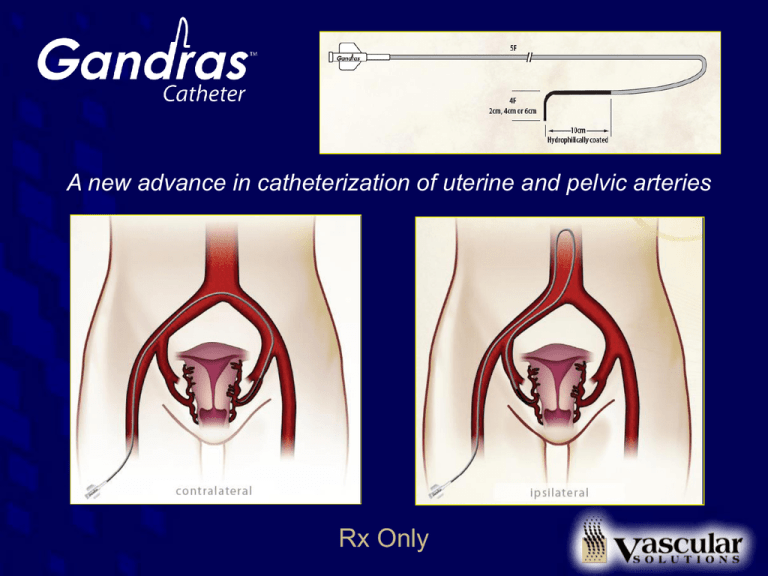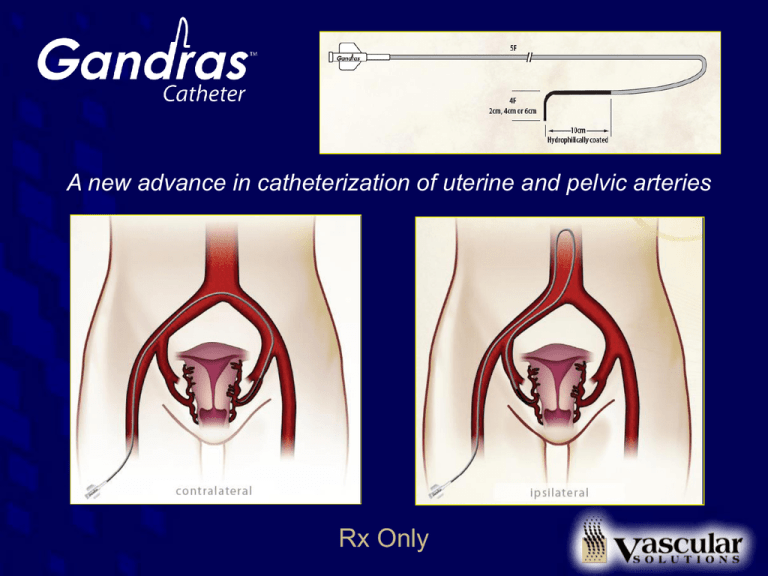
A new advance in catheterization of uterine and pelvic arteries
Rx Only
Specifications
Distal taper to 4F
Transition to floppy, radiopaque
section with hydrophilic coating
14.6cm
Distance between the curves
5F proximal end
Tip lengths:
2cm (Model 5580)
4cm (Model 5581)
6cm (Model 5582)
Catheter Deployment
Case #1 with still images and
discussion
(2cm distal tip catheter)
Pelvic Arteriogram
Initial pre-treatment pelvic angiogram via a right common femoral artery
approach using an Omni flush demonstrates bilateral hypertrophied uterine
arteries supplying an enlarged, myomatous uterus
Contralateral Catheterization
The Omni is used to place a Bentson wire over the aortic bifurcation.
Then it is exchanged and the left uterine artery is catheterized using the
Gandras catheter over a 0.035 inch angled Glidewire
Contralateral Confirmation
An injection of contrast confirms placement into the contralateral
uterine artery. Embolization can begin safely.
Contralateral Embolization
Without spasm, flow-directed embolization of the contralateral
uterine artery can proceed to stasis
Forming Reverse Curve
Once contralateral embolization is complete, the catheter is placed so the primary
curve sits perched on the aortic bifurcation, usually by pushing the catheter in over
a guidewire deeper into uterine a. or other internal iliac branch. Then the guidewire
is placed at the level of the primary curve and thecatheter is pushed up into the
aorta, forming the reverse curve.
Ipsilateral catheterization - CIA
Once a reverse curve is formed, the catheter can be pulled into the ipsilateral
common iliac artery (CIA) by steering the tip to the right
Ipsilateral catheterization - IIA
From there, the right internal iliac artery (IIA) is catheterized by directing the
tip of the catheter posterior and medially, leading with a Bentson or Terumo
angled Glidewire. Roadmapping can be helpful for this step.
Ipsilateral catheterization - UA
The catheter is then pulled into the anterior division of the internal iliac artery, off of
which the uterine artery (UA) arises. Roadmapping is helpful. This is done over
Glidewire to engage the origin of the UA. Experienced operators may be able to
select by puffing contrast without wire.
Ipsilateral catheterization - UA
Deeper seating into the uterine artery can proceed once the origin is engaged.
Avoid too much wire into the artery which can cause spasm. Withdraw wire as the
catheter is pulled in. If the UA is very tortuous a wire may be needed to straighten
the artery to allow deeper seating.
Ipsilateral catheterization - UA
This particular uterine artery has a very acute angle and is extremely tortuous
proximally, making the catheterization challenging. However, because of the
flexibility of the Gandras catheter shaft and soft tip, the artery is engaged with
minimal trauma without incident.
Ipsilateral Confirmation
Once catheterized, an injection of contrast confirms position in the
uterine artery just beyond its origin
Ipsilateral embolization
Because there is no significant spasm or reflux around the
catheter tip, the artery is occluded to stasis from this position
using flow-directed embolization without incident
Straightening and Removal
Once stasis is achieved, the Gandras catheter is pushed into the aorta with a guidewire at the
primary curve level and straightened over the bifurcation. At this point any loops that have
been created can be reduced by torquing in the correct direction while pulling down on the
catheter. A wire should remain within the length of the catheter to avoid knotting. From there
the catheter is exchanged for a flush catheter for completion angiography.
Completion
Post-embolization images demonstrate no significant filling into the
myomatous uterus with the remainder of the pelvic vasculature preserved
Completion
Pre and post embolization images
Catheter Deployment
Case #2 with fluoro loops and
discussion
(4cm distal tip catheter)
Using roadmapping, the catheter is pushed over Glidewire into
contralateral uterine artery to proximal horizontal segment.
Note, only the tapered tip is within the uterine artery.
Advancing deeper over 0.018” wire to avoid spasm
Geometry of catheter over aortic bifurcation
- note locations of primary and secondary curves
Following contralateral embolization, the catheter is advanced into
uterine artery in order to perch the catheter’s primary curve on the
bifurcation before it is pushed into the aorta
Ipsilateral catheterization without wire while “puffing” contrast –
if very tortuous arteries then guidewire
use recommended while roadmapping
Ipsiliateral deep seating without guidewire
– note the soft flexible tip minimized spasm
Flexibility of catheter with tip deep in uterine artery
Flexibility of catheter tip
Straightening and removal of 4cm tip
following ipsilateral embolization
Catheter Deployment
Case #3 with fluoro loops and
discussion
(6cm distal tip catheter)
Deep seating 6cm tip on contralateral side
without guidewire
Injection following advancement
demonstrates no significant spasm
Geometry of Gandras 6cm tip at this time –
note primary and secondary curves
Catheterization of ipsilateral CIA
Ipsilateral cath with roadmapping - note withdrawal
of wire once origin engaged
and then advancing without guidewire
Injection confirms no spasm in a medium to small uterine
artery following deep seating
Deep seating of Gandras 6cm tip without wire
- note ultra flexibility of tip of catheter
Injection confirmed no spasm following deep seating.
Why would you need to use a microcatheter?
Flow-directed embolization
without spasm can proceed
Straightening of Gandras 6cm tip following
ipsilateral embolization
Gandras 6cm removal over bifurcation
Gandras 6cm tip ipsilateral cath example #2 using
roadmap in extremely tortuous artery over wire
Injection showing ultra flexibility of Gandras 6cm tip following
ipsilateral catheterization with no significant spasm
Flow-directed embolization achieved without spasm using
ultra flexible Gandras 6cm tip
Why would you need to use a microcatheter when you can
deep-seat this tip without spasm?
The Optimal Catheter
Catheterize both uterine arteries from a single puncture site
• Quicker case
• Less anesthesia
• Less X-ray
Flexible shaft to minimize longitudinal force on artery
Tapered hydrophilic distal tip for atraumatic catheterization
Hybrid ultra flexible soft distal tip to perform like a microcatheter
• Microcatheters are very expensive!
Low profile to minimize spasm
The Gandras catheter is indicated to be used for delivering embolic
materials and radiopaque media to selected sites in the vascular
system. Diagnostic, embolic or therapeutic agents are to be used in
accordance with specifications outlined by the manufacturer. Please
see the Gandras Instructions for Use for a complete listing of
indications, contraindications, warnings and precautions.
Embedded images are representative of a typical UFE procedure using
the specially designed Gandras catheter curve shape.
USA CAUTION: Federal law (U.S.A.) restricts these devices to sale by
or on the order of a physician.
CAUTION: The Gandras catheter should be used by physicians with
adequate training in the use of the device.
Please see the appropriate product Instructions for Use for a complete
listing of the indications, contraindications, warnings and precautions.
Vascular Solutions, Inc.
6464 Sycamore Court
Minneapolis, Minnesota 55369 USA
888.240.6001
763.656.4300
www.vascularsolutions.com
This presentation is provided for your professional use and content of
individual slides may not be modified without prior consent of Vascular
Solutions, Inc.
Gandras is a trademark of Vascular Solutions, Inc.
©2009 Vascular Solutions, Inc. All rights reserved.
ML1906 Rev. B 03/09