File - CCFP-EM
advertisement
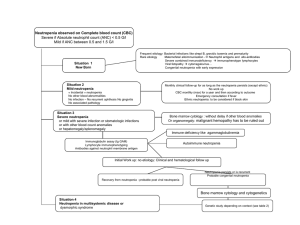
ONCOLOGY EMERGENCIES AHD “A” Dr Joseph Kozar, CCFP (EM) Mar 28, 2013 Oncology Emergencies - Categories • Local Tumour Effect -Compressions and Obstructions • Metabolic Crises • Hematologic Crises • Treatment Related Adverse Effects • Pain Crisis Oncology Emergencies • Local Tumour Effect – Compressions & Obstructions • Superior Vena Cava Syndrome • Malignant Spinal Cord Compression • Malignant Pericardial Effusion • Ureteral Obstruction • Upper Airway Obstruction • Massive Hemoptysis • Pathologic Fractures • CNS • Increased ICP effects • Seizures • GI • Obstruction • Perforation • Bleeding Oncology Emergencies • Metabolic Crises • Hypercalcemia • Hyponatremia and SIADH • Tumour Lysis Syndrome • Hyperuricemia • Tumour-associated hypokalemia • Hypoglycemia Oncology Emergencies • Hematologic Crises • Febrile Neutropenia • Hyperviscosity Syndrome • Thromboembolic disease • Acute hemolytic anemia • Thrombocytopenic bleeding Oncology Emergencies • Treatment Related Adverse Effects • Chemotherapy induced nausea and vomiting • Constipation/Obstipation • Diarrhea • Radiation induced pneumonitis, proctitis CASE • 55 yr old male with colon CA, chemo 9 days ago with 5-Fluorouracil and has T38.5 • No other infectious symptoms FEVER in the Cancer Patient • Fever occurs in chemo-induced neutropenia • 10-50% pts with solid tumours • >80% pts with hematologic malignancies • Documented infection in only 20-30% of febrile episodes 5 • Common sites of tissue based infection: GI tract, Lungs, Skin • Bacteremia in 10-25%, esp in prolonged or profound neutropenia • Non-infectious causes of fever: • Antineoplastics • Antimicrobials • Tumour necrosis • Inflammation Febrile Neutropenia - Definition • Fever • Single oral temp > 38.3 C • OR • Sustained oral temp > 38 C for > 1 hour • avoid axillary temp (inaccurate) and rectal temp (risk of infection) • Caveats 3: Elderly, steroids, sepsis presenting as hypothermia Febrile Neutropenia - Definition • Neutropenia • Absolute Neutrophil Count (ANC) < 0.5 X 109/L • OR • ANC predicted nadir < 0.5 X 109/L in next 48 hrs • Profound neutropenia = ANC < 0.1 X 109/L • Functional neutropenia = Hematologic malignancies with a qualitative defect (impaired phagocytosis and killing of pathogens) of circulating neutrophils despite normal neutrophil counts Neutropenia Typical nadir 5-10 days after last dose Recovery within 5 days of nadir Regimens for leukemias and lymphomas produce longer lasting and more profound neutropenia 4 Febrile Neutropenia • Risk of infection varies • Directly with duration of neutropenia • Directly with rate of decline • Inversely with ANC • > 20% with ANC <0.1 are bacteremic Febrile Neutropenia • Primary anatomic sites of infection often include 1: • GI tract • Chemo –induced mucosal damage allows invasion of opportunistic organisms • Skin • Invasive procedures (vascular access devices) provide portals of entry Febrile Neutropenia - Microbiology • 1960 and 1970’s gram negatives predominate • 1980 and 1990’s gram positives become more common with indwelling venous catheters • allow skin flora entry • Fungal : Candida & Asperigillus • consider in fevers unresponsive to antibacterials Febrile Neutropenia - Current Microbiology • Coagulase-negative staph most common blood isolate in most centres • Enterobacteriaciae (Enterobacter, E coli, Klebsiella) as well as Pseudomonas and Stenotrophomonas less common • Recently, drug resistant Gram Negatives on the rise in some centres • Gram Negative resistance • ESBL (Klebsiella and E coli) • Carbapenamase resistance (Klebsiella and Pseudomonas -KPC) • Gram Positive resistance • MRSA • VRE • penicillin resistant Strep pneumoniae & viridans Febrile Neutropenia • Diagnosis of infection is difficult because signs & symptoms of inflammation often attenuated or absent • skin and soft tissue infections may lack erythema, warmth, induration, pus • chest infection may have no infiltrate on CXR • UTI may have little pyuria • Fever often only sign of serious infection • Rigors or toxic appearance highly associated with infection and possible bacteremia Febrile Neutropenia - Historical Features • Underlying malignancy • Timing and type of chemo • Nadir usually 5-10 days after chemo • Site specific infectious symptoms • Presence of central venous catheters (CVC) • Anti-microbial prophylaxis • Prior documented infections or pathogen colonization • Underlying comorbid conditions eg DM, COPD, CKD, recent surgical procedures Febrile Neutropenia - Physical Exam • Vitals • Most common infection sites • Chest • Skin esp current or past catheter sites, marrow aspiration sites, periungal area • Oropharynx including gums • Abdomen • Perineum • no rectal exam Febrile Neutropenia - Investigations • Cultures • Blood Cultures • > 2 sets ( a set = 20 mL divided in aerobic and anaerobic bottles) • if CVC present, culture from each lumen plus a peripheral source • Urine C&S • If S&S of UTI, urinalysis abnormal or catheter present • Sputum C&S if productive cough • Stool for C diff toxin assay only if diarrhea • No bacterial C&S or O&P unless travel history • CSF if meningitis clinically suspected • Skin :aspiration of clinically suspected infection Febrile Neutropenia - Investigations • CBC and differential • Creatinine, Urea, LFTs, electrolytes • CXR if respiratory symptoms • CT as clinically indicated (eg Head, sinuses, chest, abdomen/pelvis) • Interestingly, CT chest will reveal evidence of pneumonia in >50% of febrile neutropenics with normal CXR CASE • 55 yr old male with colon CA, chemo 9 days ago with 5-Fluorouracil and has T38.5 • No other infectious symptoms • No significant past medical history • Looks well • Vitals normal • Porta-cath • No evidence infection • Exam: no abnormalities • ANC = 0.2 X109/L Question • Which antibiotics will you give him? • A] Cipro po & Clavulin po • B] Piperacillin/Tazobactam IV & Vancomycin IV • C] Meropenem IV • D] Ceftazidime IV & Gentamicin IV • E] Piperacillin/Tazobactam IV Febrile Neutropenia - Therapy • Febrile Neutropenia is a medical emergency • Start Empiric broad spectrum antibiotics promptly (< 2 hrs) as untreated infections have 25-50% mortality at 48hrs • No specific drug or combination can be unequivocally recommended for all pts • Guidelines applicable in most situations, but require modification based on local circumstances and epidemiologic data • Change from previous guidelines: More structured assessment of individual febrile neutropenic patient as high or low risk for serious infectious complications • Affects therapy and venue of therapy Febrile Neutropenia - Risk Assessment • Can divide patients into high risk or low risk for infectious complications • High Risk patients: IV antibiotics as inpatients • Low Risk patients: Carefully selected Low Risk patients may be eligible for Oral and / or Outpatient antibiotic therapy (?early discharge) • 2 risk assessment tools: • Clinical • Formal classification with MASCC scoring system Febrile Neutropenia - Risk Assessment • Clinical Criteria for High Risk • Profound neutropenia (ANC < 0.1) and anticipated to last > 7 days • Hepatic insufficiency (aminotransferases >5X normal) • Renal insufficiency (Creat clearance <30 mL/min) • Presence of any co-morbid medical problems including but not limited to: • Hemodynamic instability • Oral or GI mucositis that interferes with swallowing or causes severe diarrhea • Neurologic or mental status changes of new onset • Intravascular catheter infection, esp catheter tunnel infection • New pulmonary infiltrate or hypoxemia, or underlying chronic lung disease Febrile Neutropenia - Risk Assessment • Clinical Criteria for Low Risk • Anticipated neutropenia < 7days • No or few co-morbidities • Stable and adequate hepatic and renal function • More often in solid tumours Febrile Neutropenia - Risk Assessment High risk <21 Low risk >21 Fundamental problem is nebulous nature of “Burden of febrile neutropenia and symptoms associated with that burden” Febrile Neutropenia - Treatment • Goal of initial empiric antibiotics: Prevent serious morbidity and mortality until results of cultures available to guide more precise antibiotic choices • However recent prospective observational study of > 2000 pts revealed only 23% with documented bacteremia • gram positives: 57% • gram negatives: 34% • polymicrobial: 9% • But mortality: Gram Negatives 18% > Gram Positives 5% • Even if blood cultures negative, empiric antibiotics considered vital to cover occult infections Febrile Neutropenia - Treatment • despite decades of well performed clinical trials, no single empiric regimen proved superior • all effective regimens share certain features: • bactericidal in the absence of WBCs • anti-pseudomonal activity • minimal toxicity • Recently, increasing array and incidence of resistant pathogens causing challenges in the treatment of febrile neutropenics Febrile Neutropenia - IDSA 2010 Febrile Neutropenia - Treatment • Initial IV antibiotics: Monotherapy with anti-pseudomonal Beta-lactam • Piperacillin-Tazobactam: 3.375 IV q6h • Carbapenem : eg Meropenem 1g IV q8h • Cefipime: (4th generation cephalosporin) 2g IV q12h • Ceftazidime: (3rd gen cephalosporin) 1g IV q8h • Many centres find has decreased potency gram negatives & poor activity against many gram positives eg streptococci so has fallen out of favour Febrile Neutropenia - Treatment • Vancomycin (or other gram positive agent) not part of empiric initial therapy • Randomized studies show no difference with or without Vancomycin for empiric initial therapy despite predominance of cultures being gram positive (most common coagulase negative staph) • Add Vancomycin for specific indications -Table 4 Febrile Neutropenia - Treatment • Modifications to initial empiric antibiotic therapy for pts at risk for with antibiotic resistant organisms esp • if unstable • positive blood cultures suspicious for resistant bacteria Febrile Neutropenia - Treatment • Penicillin allergic patients with immediate type hypersensitivity • Ciprofloxacin + Clindamycin • Aztreonam + Vancomycin • AFEBRILE NEUTROPENIC pts with signs and symptoms of infection should be evaluated and treated as high risk patients Febrile Neutropenia - IDSA 2010 Febrile Neutropenia - Treatment • Low Risk Pts should receive initial Oral or IV empiric antibiotics in hospital or clinic setting • Recommended empiric Oral Rx: Ciprofloxacin + Clavulin • Alternatives are less well studied: • Levofloxacin monotherapy • Better gram positive coverage than cipro but less potent anti-pseudomonal coverage so should use 750mg daily dose for higher bacericidal drug concentrations • Ciprofloxacin + Clindamycin Febrile Neutropenia - Treatment • 2 large placebo controlled studies of low risk patients showed Oral cipro & clavulin comparable to empiric IV therapy, However, both groups were inpts • few studies have assessed feasibility of treating low risk patients solely in outpatient settings • most studies have observed pts in hospital for 24hrs of empiric therapy, although a few have discharged patients 6 hrs after antibiotics initiated • outpt oral or IV therapy can be considered after brief inpt stay, with IV antibiotics initiated, fulminant infection excluded, patient deemed low risk and stable, outpatient supports in place, status of initial cultures ascertained, prompt access (< 1hr from medical facility) to medical care 24/7 Outpatient management of febrile neutropenia • At TOH, decision made by oncology • “Outpt strategy should not be viewed as the current standard of care for febrile neutropenic patients” 3 CASE • 55 yr old male with colon CA, chemo 9 days ago with 5-Fluorouracil and has T38.5 • No other infectious symptoms • No significant past medical history • Looks well • Vitals normal • Porta-cath • No evidence infection • Exam: no abnormalities • ANC = 0.2 X109/L Question • Which antibiotics will you give him? • A] Cipro po & Clavulin po • B] Piperacillin/Tazobactam IV & Vancomycin IV • C] Meropenem IV • D] Ceftazidime IV & Gentamicin IV • E] Piperacillin/Tazobactam IV Summary • Febrile Neutropenia • IDSA 2010 guidelines • ANC < 0.5 • Early antibiotics • Pip/Tazo +/- Vancomycin References – Febrile Neutropenia • 1. Hughes et al. 2002 Guidelines for the Use of Antimicrobial Agents in Neutropenic Patients with Cancer. Clinical Infectious Diseases 2002; 34: 730-51. • 2. Bal, Gould. Empirical Antimicrobial Treatment for Chemotherapy-induced Febrile Neutropenia. International Journal of Antimicrobial Agents 2007; 29: 501-509. • 3. Adelberg DE, Bishop MR. Emergencies related to cancer chemotherapy and hematopoietic stem cell transplantation. Emergency Med Clin N Am 2009; 27: 311-331. • 4. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81:835-848. • 5. Freifeld AG et al. Clinical Practice Guideline for the Use of Antimicrobial Agents in Neutropenic Patients with Cancer: 2010 Update by the Infectious Disease Society of America. Clinical Infectious Diseases 2011; 52(4): e56-e93. Case • 62 yo male • NHL, finished 5 days of chemo 2 days ago (fludarabine) • Very weak, nausea and vomiting • BP 124/71, HR 60, RR 26, T 35.5, O2Sat 98% • Monitor wide complex, regular, slow What oncology emergency is this? ANSWERS? • A] Hypercalcemia • B] SIADH • C] Tumour Lysis Syndrome • D] Tumour associated hypokalemia • E] Hypomagnesemia Case Lab Results Na 133 L K 9.7 H Cl 100 Lactate 3.3 pH 7.23 pCO2 28 HCO3 12 H (0.5 - 2.2) CO2 11 L Glu 15.2 H AG 22 H pO2 153 Urea 44.3 H O2Sat 100% Creat 488 H Phos 7.74 H (0.78 - 1.53) WBC 6.6 Ca 2.11 L (2.23 - 2.58) Hb 94 L Pit 51 L INR 1.21 Mg 1.65 H (0.74 - 1.03) Alb 45 (34 - 46) Uric Acid 2755 H (210 - 450) Tumour Lysis Syndrome • Massive release of intracellular contents after tumour cell death 1,2 • Chemo usually • Radiation • Spontaneous • Overwhelms the normal homeostatic mechanisms • kidneys Tumour Lysis Syndrome • Metabolic derangements 1,2 • Hyperuricemia from DNA breakdown • Hyperkalemia from cytosol breakdown • Hyperphosphatemia from protein breakdown • Hypocalcemia develops secondary to hyperphosphatemia TLS • Hyperuricemia • Uric acid poorly soluble • Crystallization in renal tubules • Obstructs tubular flow • Acute renal failure TLS • Hyperphosphatemia • Kidneys initially increase excretion but become overwhelmed by phosphate load • Exacerbated by renal failure from hyperuricemia • Nausea, vomiting, diarrhea • Lethargy, seizures • Crystallization of calcium phosphate in renal tubules • Obstruction of tubular flow and worsening renal failure • Secondary hypocalcemia • Arrhythmia • Hypotension • Tetany, muscle cramps TLS • Hyperkalemia • Exacerbated by renal failure from hyperuricemia and hyperphosphatemia • Arrhythmias • Muscle cramps • paresthesias TLS • Renal failure • Induced by • hyperuricemia • uric acid precipitates in renal tubules • hyperphosphatemia • precipitation of calcium phosphate in renal tubules • Volume depletion • Preexisting renal failure makes syndrome more severe but even normal kidneys can be overwhelmed by rapid cell lysis and release of cell contents TLS • Mainly with hematologic malignancies that are extremely sensitive to therapy 1 • Acute leukemias • ALL, AML • High grade lymphomas • Burkitt’s lymphoma • High grade NHL • Has also been described with • Small cell lung ca • Germ cell tumors • Occurs 1-5 days post chemo or radiation TLS -Symptoms • Non specific • lethargy • GI • Nausea &vomit • Diarrhea • Anorexia • Cardiac • Fluid overload, edema, CHF • Dysrhythmias & sudden death • Neuro • Seizure • Tetany • Renal • Oliguria • hematuria TLS - Definition Coiffier B et al. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J Clin Oncol 2008; 26: 2767-2778. TLS - Definition Coiffier B et al. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J Clin Oncol 2008; 26: 2767-2778. TLS – Prevention & Treatment • Best treatment is prevention • Aggressive hydration and diuresis • Promotes excretion of uric acid & phosphate • Diuresis with furosemide only if no hypovolemia • Urine alkalinization no longer recommended1 • May cause ppt of xanthine and CaPO4 in renal tubules • Allopurinol • Blocks conversion of xanthine and hypoxanthine to uric acid • PO or IV TLS – Prevention & Treatment Coiffier B et al. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J Clin Oncol 2008; 26: 2767-2778. TLS - Treatment Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81:835-848 TLS - Treatment Coiffier B et al. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J Clin Oncol 2008; 26: 2767-2778. Summary • Tumour Lysis Syndrome • Hematologic malignancies undergoing chemo • Increased uric acid, PO4, K; decreased Ca • Renal failure • Fluids, diuresis, treat electrolyte abnormalities, allopurinol (rasburicase = fasturtec), dialysis References – Tumour Lysis Syndrome • 1. Coiffier B et al. Guidelines for the Management of Pediatric and Adult Tumor Lysis Syndrome: An Evidence-Based Review. J Clin Oncol 2008; 26: 2767-2778. • 2. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81:835-848. Case A • 60 yr old female treated for breast cancer 7 yrs ago with lumpectomy, adjuvant chemo and radiation • Local recurrence last year treated with chemo • Increasing low back pain for 1 month • Requiring increasing dose of analgesics • Percocet 2 q4h • Naproxen 500 bid • No radicular, bowel or bladder symptoms, signs Case A Question • Would you • A] Switch percocet to hydromorphone and follow up with FMD • B] Xray. If normal have pt followup with FMD for bone scan. If abnormal arrange for emergent MRI spine, give Decadron 10 mg IV • C] Arrange emergent MRI • D] Arrange for urgent outpt CT Spine • E] Consult radiation oncology • F] Arrange urgent MRI (next 48hrs) Case B • 73 yr old male presenting with a 3 month history of increasing back pain and last 2 weeks bilateral radicular leg pain • Past medical Hx: nil • Increasing opioid requirements • Dilaudid 4mg q4h • Last 3 days have difficulty mobilizing in home because of pain and leg weakness • Today unable to urinate • ROS: Weight loss & Night sweats • Exam • Bilateral leg weakness (3/5) • Decreased rectal tone • Urinary retention CASE B -Question • Would you • A] Xray, increase hydromorphone dosage, Decadron 10 mg IV, contact spine specialist in the morning • B] Arrange emergent consult with Spine Service • C] Arrange for emergent CT Spine, Decadron 100mg IV • D] Arrange for emergent MRI, Decadron 10 mg IV Malignant Spinal Cord Compression • Metastases to the spine or epidural space that compresses the spinal cord • Develops in 2.5%-6% of all terminal cancer patients 1 • Most common primary tumour sources 1,2,3,4 • Breast 29% • Lung 17% • Prostate 14% • Others: NHL, Renal cell, Multiple myeloma (5-10%) • Location in spine • Thoracic 59-78% • Lumbar 16-33% • Cervical 4-15% • Multiple levels involved in up to 50% Malignant Spinal Cord Compression • 80% of cases of MSCC occur in patients with pre-existing diagnosis of malignancy 1 • Back pain in pt with known cancer should be considered secondary to MSCC until proven otherwise 1 • Corollary: 20% of cases in patients with no previous diagnosis of cancer 2 • A medical emergency MSCC: Pathophysiology • Develops in 3 ways 4 • Growth and expansion of vertebral metastasis into epidural space Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. MSCC: Pathophysiology • Neural foramina extension by a paraspinal mass • Lymphoma • neuroblastoma MSCC: Pathophysiology • Destruction of vertebral cortical bone, causing vertebral body collapse and displacement of bony fragments into the epidural space L2 and S1 compression fractures in metastatic bronchogenic carcinoma MSCC: Pathophysiology • Can lead to instability of spine if 2 or 3 columns disrupted 3 Denis’ 3 column model of spinal stability. Destruction of 2 or 3 columns may lead to structural instability Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. MSCC: Pathophysiology • Spinal cord damage is multifactorial and complex, but predominantly vascular in nature • Tumour or bony fragment causes venous plexus compression, which leads to edema of spinal cord • Edema causes increased pressure on small arterioles leading to decreased capillary flow and white matter ischemia and eventually infarction MSCC: Presentation • 80% have pre-existing cancer diagnosis • Symptoms 2,3 • Back pain 83-95% • Initially local due to tumour stretching periosteum or invading soft tissue • May be severe, constant, progressive • Worse recumbent due to lengthening of spine • Worse with valsalva, cough, sneeze • Radicular from compression or invasion nerve roots • Mechanical • Suggests vertebral body collapse and spinal instability MSCC: Presentation • Symptoms • Back Pain • Motor Deficit 83-95% 60-85% • Clumsiness or heaviness progressing to paralysis • 50% non-ambulatory at diagnosis • UMN weakness • Usually symmetric • LMN weakness • Usually asymmetric MSCC: Presentation • Symptoms • Back Pain • Motor Deficit • Sensory Deficit 83-95% 60-85% 40-80% • Rarely occur before motor deficits or pain • Usually begin distally & ascend • Gait disturbance/falls with progression of motor and sensory deficits MSCC: Presentation • Symptoms • Back Pain 83-95% • Motor Deficit 60-85% • Sensory Deficit 40-80% • Autonomic/Sphincter Dysfunction 40-60% • Typically a later finding • Among elderly, urinary retention more reliable finding than urinary incontinence • Poor prognostic indicator MSCC: Diagnosis • MRI • Study of choice & gold standard 1,2,3,4 • Sensitivity 93% • Specificity 97% • Should image the entire spine because multiple levels frequently involved • CT • If contraindications or lack of availability of MRI • MR image of cord compression at T5 & T11 in patient with lymphoma Figure 2 MRI of the patient's cervical spine Selvaggi K and Abrahm J (2006) Metastatic spinal cord compression: the hidden danger Nat Clin Pract Oncol 3: 458–461 10.1038/ncponc0561 MSCC: Diagnosis • Xray • Insufficient sensitivity or specificity • 30-50% of bone must be destroyed before visible on plain films 2 • Bone may not be affected if neural foraminal extension • 80% patients with symptomatic spinal mets have abnormal plain films 1,2 • Radionuclide bone scans and PET can detect MSCC but are not as accurate as MR 2,3 C4 metastatic # L2 met from breast CA Superior endplate deformity MSCC: Therapy • Corticosteroids • Decrease cord edema • By inhibiting production of vascular EGF released with cord hypoxia • Delays neurologic deterioration • Proven bridge to definitive treatment • Should be started ASAP • Some say before MRI 4 • Some say after MRI, but to give immediately if there is a delay to imaging 1 MSCC: Therapy • Dexamethasone • No consensus on dosing 1,3 • Moderate dose • 10 mg IV loading dose • Followed by 16 mg daily divided q6-8h • High dose • 100 mg IV loading dose • Followed by 96 mg/d • May have slightly better outcome but higher adverse effects • GI bleeds • GI perforation • psychoses MSCC: Therapy • Rapidly progressive motor symptoms use high dose? • Minimal or non progressive weakness use moderate dose? 3 • TOH Radiation oncology (Dr Grimard) advises • Decadron 10 mg IV MSCC: Therapy • Radiotherapy • Standard of treatment 1,4 • Preserves or improves neuro function • Optimal dose and treatment regiment controversial • Arrests progression of tumour temporarily but doesn’t stabilize spine • Takes days to work • Insufficient to treat SCC caused by vertebral body collapse and displacement of fragments into epidural space MSCC: Therapy • Surgery • Allows immediate cord decompression • Opportunity to stabilize spine • First RCT (2005) comparing direct decompressive and reconstructive surgery followed by radiotherapy with radiotherapy alone 5 • Ability to walk surgery 84% radio 57% • Retain ability to walk surgery 122d radio 13d • Regain ability to walk surgery 62% radio 19% • Survival surgery 126d radio 100d • Many exclusion criteria, medical suitability and overall prognosis mean that wouldn’t apply to all patients MSCC: Therapy • Agreed upon indications for surgery • Spinal instability • Bony fragment compression • Should be evaluated by a spine surgeon Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. MSCC: Therapy • Need coordination of: • Radiation oncology • Spine surgery • Diagnostic imaging QCH-TOH Decision tree for suspected cord compression Sept 2009 MSCC: Prognosis • Prognostic factors 1,4 • Rapidity of symptom onset • Favourable histology (multiple myeloma, germ cell tumours, small cell carcinoma) • Pretherapy ambulatory function • 80-100% who are ambulatory when they begin radiation maintain walking ability • 1/3 who are not mobile, regain ambulatory status MSCC: Prognosis • Overall limited survival • Median survival about 3-6 months 3 • up to 1/3 survive > 1 year 4 • Goal is to maintain quality of life • Control pain • Avoid complications • Preserve neurologic function Case A • 60 yr old female treated for breast cancer 7 yrs ago with lumpectomy, adjuvant chemo and radiation • Recurrence last year • Increasing low back pain for 1 month • Requiring increasing dose of analgesics • Perocet 2 q4h • Naproxen 500 bid • No radicular, bowel or bladder symptoms, signs CASE A - Question • Would you • A] Switch percocet to hydromorphone and follow up with FMD • B] Xray. If normal have pt followup with FMD for bone scan. If abnormal arrange for emergent MRI spine, give Decadron 10 mg IV • C] Arrange emergent MRI • D] Arrange for urgent outpt CT Spine • E] Consult radiation oncology • F] Arrange urgent MRI (next 48hrs) Case A Case B • 73 yr old male presenting with a 3 month history of increasing back pain and last 2 weeks bilateral radicular pain • Past medical Hx: nil • Increasing opioid requirements • Dilaudid 4mg q4h • Last 3 days have difficulty mobilizing in home because of pain and leg weakness • Today unable to urinate • ROS • Weight loss • Night sweats • Exam • Bilateral leg weakness (3/5) • Decreased rectal tone • Urinary retention CASE B - Question • Would you • A] Xray, increase hydromorphone dosage, Decadron 10 mg IV, contact spine specialist in the morning • B] Arrange emergent consult with Spine Service • C] Arrange for emergent CT Spine, Decadron 100mg IV • D] Arrange for emergent MRI, Decadron 10mg IV Case B MRI of paraspinal lymphoma Sagittal T1-weighted image shows invasion of a tumor of the bone marrow and growth in the neural foramen at two levels (arrows). Summary • Malignant Spinal Cord Compression • High index suspicion in Cancer patient with back pain • Red flags: neurologic signs & symptoms • MRI emergent or urgent • Steroids early: Decadron 10 mg IV • Referral to radiation oncology/spine service References - MSCC • 1. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81:835-848. • 2. Glauser J. Oncologic Emergencies. Emergency Medicine Reports 2009;30 (8) • 3. Sun H, Nemecek A. Optimal Management of Malignant Epidural Spinal Cord Compression. Emerg Med Clin N Am 2009; 27: 195-208. • 4. Kwok Y et al. Radiation Oncology Emergencies. Hem/Onc Clin N Am 2006;20: 505-522. • 5. Patchell RA et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005; 366: 642-648. Case • 60 yr old female brought by husband because of progressive symptoms over last 4 weeks; 3rd ED visit • Back pain requiring increasing doses of morphine • 20 mg q4h • No radicular, bowel or bladder symptoms • Fatigue • Nausea, occ. Vomiting • Poor appetite • Generalized weakness • Confused Case • PMHx • Breast Ca in remission for 5 yrs • Exam • HR 90, BP 130/75, RR 12, T 36.5, O2 sat 95% • No apparent pain • Very poor historian, slow to answer, apathetic • Needs help to sit up but no focal weakness • Pupils 2mm What oncology emergency is this? Question • What oncology related electrolyte abnormality is present on the ECG? • A] Hyponatremia (SIADH) • B] Hypercalcemia • C] Hyperkalemia & Hyperphosphotemia • D] Hypocalcemia • E] Hypomagnesemia Labs Na K Cl CO2 Glu Creat Urea Ca Mg PO4 Alb 144 3.9 110 24 6.5 155 9.9 3.50 0.99 0.70 37 L H H H (2.20 - 2.52) (0.74-1.03) L (0.78-1.53) (35 - 48) Hypercalcemia of Malignancy • Occurs in 20-30% of patients with cancer 1,2,3 • Most common serious electrolyte abnormality in adults with cancer • Usually in patients with established diagnoses of cancer but can be presenting feature • Associated with: • Multiple myeloma • Lung • Breast • prostate • Kidney • Leukemia • Metastatic tumours with extensive bony involvement Hypercalcemia of Malignancy 4 Mechanisms • Local osteolytic hypercalcemia 1,3 • Osteoclastic bone resorbing cytokines • Extensive metastases • 20% • Humoral hypercalcemia of malignancy • Parathyroid hormone related peptide (PTHrP) secreted systemically • Binds to PTH receptors, thereby mobilizing calcium from bone and increasing renal reabsorption of calcium • 80% Hypercalcemia of Malignancy 4 Mechanisms • Vit D 1,25 secreting lymphomas • Active form of Vitamin D causing enhanced osteoclastic bone resorption and enhanced intestinal absorption of calcium • <1% • Ectopic hyperparathyroidism • <<1% Hypercalcemia of Malignancy • Total serum calcium is usually measured • Varies with albumin level • Correction factor • Corrected Ca = measured Ca (mmol/L) + 0.02X(40 - measured Albumin (g/L)) • Accuracy questioned • Ionized calcium is more accurate Hypercalcemia of Malignancy • Severity: No formal guidelines exist 1 • Mild: 2.6 -2.9 mmol/L • Moderate: 3.0 -3.4 mmol/L • Severe: >3.5 mmol/L Hypercalcemia of Malignancy • Symptoms • Insidious onset • Severity of symptoms vary with • Level of hypercalcemia • Rapidity of onset • Pre-existing cognitive dysfunction • Concomitant sedatives/narcotics Hypercalcemia of Malignancy Symptoms • GI • Early, frequent, mistakenly attributed to disease or therapy • Nausea, vomiting • Anorexia • Constipation • Renal • Polyuria due to interference with ADH- Diabetes insipidus-like syndrome • Polydipsia • Dehydration from nephrogenic DI and anorexia, nausea & vomiting Hypercalcemia of Malignancy Symptoms • Neurologic • Lethargy and fatigue • Cognitive and behavioural changes • Altered mental status to coma • Muscle weakness EKG in Hypercalcemia • Hallmark : abnormal shortening of QTc because of short ST • Other: U waves (V3), bradydysrhythmias (unusual): AV block, sinus arrest, SA block Hypercalcemia of Malignancy - Lab • Total calcium & albumin or ionized calcium • Medical emergency above 3.50 mmol/L (total) 1,4 • Phosphorus • Hypophosphatemia common and can worsen condition • Creatinine, urea elevated • Electrolytes • 50% are hypokalemic • PTH level Question • First Line treatment for her hypercalcemia (Ca= 3.50 mmol/L)? • A] Pamidronate IV • B] Mithramycin IV • C] Aggressive fluid rehydration with NS followed by Furosemide • D] Prognosis very poor, no treatment • E] Calcitonin SQ Hypercalcemia of Malignancy Treatment • Aggressive rehydration with NS 200-500 ml/hr • Dehydration occurs secondary to: • polyuria from renal tubular dysfunction (nephrogenic diabetes insipidus) • Vomiting and anorexia • Watch for fluid overload in those at risk • Followed by furosemide 40-60mg IV after adequate urine output established • Blocks calcium reabsorption in loop of henle Hypercalcemia of Malignancy Treatment • Bisphosphonates 1 • First- line • Inhibit osteoclastic bone resorption • Onset of effect 2-4 days • Peak effect 4-7 days • 60-90% pts normalize calcium • Response lasts for 1-3 weeks • Pamidronate Hypercalcemia of Malignancy Treatment • Adjunctive treatment • Discontinue calcium replacement, vitamin D, Thiazide diuretics • If possible reduce sedatives and narcotics • Increased weight bearing • Replace phosphate orally if low • Sodium Phosphate (Phosphate Novartis )500 mg po bid • Glucocorticoids • Prednisone 1-2 mg/kg/day Hypercalcemia of Malignancy Treatment • Superseded by bisphosphonates • Calcitonin • 4-8IU/kg q6-q12h SC or IM • Rapid but modest & transient reduction • Mithramycin • Manufacturer discontinued production in 2000 • Antihypercalcemic therapy is interim measure • Antitumour therapy if appropriate 3 Hypercalcemia of Malignancy • Prognosis • Very Poor • Approx. 50% die within 30 days 3 • May be appropriate and humane to withhold hypercalcemia therapy 1,2 • Will result in coma and death Question • First Line treatment for her hypercalcemia (Ca= 3.50 mmol/L)? • A] Pamidronate IV • B] Mithramycin IV • C] Aggressive fluid rehydration with NS followed by Furosemide • D] Prognosis very poor, no treatment • E] Calcitonin SQ Summary • Hypercalcemia • Common in numerous cancers • Insidious onset, non-specific symptoms • IV hydration, furosemide • Bisphosphonates: Pamidronate, Zolendronic acid • Check Ca, PO4 in oncology patients References - Hypercalcemia • 1. Stewart AF. Hypercalcemia associated with Cancer. NEJM 2005; 352: 373-379 • 2. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81:835-848. • 3. Kacprowicz RF, Lloyd JD. Electrolye Complications of Malignancy. Emerg Med Clin of N Am 2009; 27:257-269. • 4. Glauser J. Oncologic Emergencies. Emergency Medicine Reports 2009;30 (8) Case • 68 yr old male receiving chemo for Non-small cell lung CA who for past week • Anorexia • Nausea, vomiting • Generalized weakness • Found by wife, on floor, ++ confused but confusion has improved significantly since arrival • c/o headache Case • Exam • Afebrile, vitals unremarkable • Euvolemic • Tongue bite mark • No localizing neuro symptoms • GCS =15, mild confusion regarding recent events this week Case Na 113 L Cl 81 L CO2 24 K 4.5 Glu 6.1 Urea 5.0 Creat 101 Ca 2.32 (2.20-2.52) Question • What is your initial management? • A] IV NS fluid bolus 1L, then 125 mL/hr • B] Ativan 2 mg IV • C] Hypertonic saline (3%) 100mL over < 1hr • D] Demeclocycline 300 mg po • E] Restrict oral fluids to 1L/day Hyponatremia • An excess of water in relation to sodium in the ECF • For this to occur: An inability of body to excrete free water through kidneys despite continued water intake 2,3 Hyponatremia - Symptoms • None • GI • Anorexia • Nausea, vomiting • Constipation • General • Myalgias • Malaise, lethargy • CNS Hyponatremia • Severity 3 • Mild: <135 mmol/L • Moderate : <130 mmol/L • Severe: <125 mmol/L Hyponatremia • Severity of symptoms highly dependent on rate of development of hyponatremia 1 • Brain is most sensitive organ • As [Na] declines, water shifts intracellularly down the osmotic gradient and results in cerebral edema • If [Na] decline is slow, brain cells can adapt by expelling K and other osmotically active substances & maintain near normal cell volume 1 • Symptoms much less severe in chronic hyponatremia Yeates, K. E. et al. CMAJ 2004;170:365-369 SIADH Diagnostic Criteria • Serum Osmolality decreased • <280 mOsm/kg • Euvolemic • Urine osmolality not maximally dilute • > 100 mOsm/L • Urine [Na] high • >40 mmol/L • Normal thyroid and adrenal function • No recent use of diuretics SIADH Causes Yeates KE et al. Salt and Water: a simple approach to hyponatremia. CMAJ 2004; 170: 365-369. SIADH in Cancer • Etiology 1 • Small cell lung CA • Occasionally with other solid tumors • Primary and metastatic brain malignancies • Pancreatic • prostate • Drug induced • Vincristine • Cyclophosphamide • Cisplatin/carboplatin • Morphine SIADH • Hyponatremia associated with cancer most commonly caused by SIADH 1 • Mechanism • Ectopic production of Arginine Vasopressin (AVP = ADH) by tumour cells • Results in absorption of free water in the renal collecting ducts • Hyponatremia, hypotonicity of serum • Inappropriately concentrated urine • Normally hypotonicity should suppress the production of AVP, but tumour cells don’t respond and keep producing AVP Baroreceptors -low BP or blood volume stimulates ADH release Treatment of Hyponatremia • Tailor treatment to symptoms, severity and chronicity of hyponatremia 1,2,3,4 • Rapidly correcting [Na] in chronic hyponatremia and minimal symptoms can be disastrous 1 • Osmotic demyelination syndrome = Central pontine myelinolysis • Destruction of oligodendrocytes and myelin in pons, basal ganglia and cerebellum • Quadriparesis • Pseudobulbar palsy • Altered mental status • Locked-in syndrome • Coma & death Osmotic Demyelination Syndrome • Recall that during chronic hyponatremia, osmolytes are shifted out of brain cells to avoid shift of water into cells and brain edema • With rapid correction of [Na], brain cells not able to reaccumulate these osmolytes quickly enough resulting in water shift out of cells hence cell shrinkage and concentrated ion damage1 Osmotic Demyelination Syndrome • Risk is related to • Chronicity • Acute : < 48 hrs - low risk • Chronic: > 48 hrs - high risk • Usually difficult to determine in ED • Severity: [Na] < 120 mmol/L usually • Rate of rise of [Na] • Most strongly associated with rate rise 1,4 • > 12 mEq/L/24 hrs • >18 mEq/L/ 48hrs • Most recent guidelines recommend limiting correction to 8 mEq/L/24hrs 1,4 Treatment of Chronic Hyponatremia Treatment of Chronic Hyponatremia Treatment of SIADH/Chronic Hyponatremia • No data from randomized trials 3 • Rapid correction required if 1 • Seizures • Respiratory depression • Altered mental status • Coma Emergent Treatment of Hyponatremia • Hypertonic Saline (3%) • Formulas for calculating free water excess and sodium deficits 1,3 • Cumbersome • Reliability? • Avoid calculating Na deficits – not physiologically based • Simpler approach 3 1,3 • 1 mL/kg/hr of 3% NS • Results in approx an increase of 1 mEq/L serum Na/hr • Monitor [Na] q 1-2 h and stop if any of: • Resolution of symptoms • [Na] of 120 mEq/L reached • Daily limit of 6-8 mEq/L correction reached (although some say up to 10 or 12 mEq/L) 1,3,4 Emergent Treatment of Hyponatremia Emergent Treatment of Hyponatremia • Pts at risk of volume overload or hx CHF 1,3 • Furosemide 20- 40 mg IV • Promotes free water excretion & Prevents ECF volume expansion • Seizures: Can add standard anti-seizure treatment Emergent Treatment of Hyponatremia • If overcorrection occurs, can relower Na to reduce risk of ODS 1,3 Non-Emergent Treatment SIADH • With mild symptoms/chronic hyponatremia • Risk of rapid correction > benefit • Fluid Restriction 2,4 • <1000-1250 mL/day • Treatment of underlying tumour Treatment of SIADH • Disposition 1 • Any significant symptoms • Admit • Without significant symptoms but [Na] < 125 • Admit for fluid restriction and further evaluation usually warranted • [Na] 126-130 mEq/L • Dependent on availability of followup and overall clinical situation Treatment of SIADH • Long Term Management • Treatment of tumour • Demeclocycline 2,4 • 300-600 mg po bid • Induces a drug-induced diabetes insipidus by diminishing the intracellular effect of ADH on renal tubular cells • Can also be used if fluid restriction not successful after several days Future Treatment ? • Arginine vasopressin receptor antagonists (Vaptans)1,3 • Approved for clinical use in USA • Not approved in Canada with no plans to proceed • Mechanism • Interacts with the vasopressin receptor at the renal collecting duct level • Blocks receptor causing aquaresis resulting in relative increase in serum Na • Demonstrated usefulness in euvolemic and hypervolemic hyponatremia • Conivaptan • 20 mg IV bolus over 30 min and then by infusion of 20-40 mg over next 24 hrs • No clinical trials addressing use in severely symptomatic hyponatremia Case • Exam • Afebrile, vitals unremarkable • Euvolemic • Tongue bite mark • No localizing neuro symptoms • GCS =15, mild confusion regarding recent events this week Case Na 113 L Cl 81 L CO2 24 K 4.5 Glu 6.1 Urea 5.0 Creat 101 Ca 2.32 (2.20-2.52) Question • What is your initial management? • A] IV NS fluid bolus 1L, then 125 mL/hr • B] Ativan 2 mg IV • C] Hypertonic saline (3%) 100mL IV over < 1hr • D] Demeclocycline 300 mg po • E] Restrict oral fluids to 1L/day Summary • Hyponatremia • Small cell lung ca • Treatment dictated by severity of symptoms and rate of onset • Correct rapidly if seizures, altered LOC, resp depression • 3% hypertonic saline 100 mL OR • 3% hypertonic saline1 ml/kg with max change of 6-8 mEq/24 hrs • Fluid restriction • Treatment of underlying tumour References - SIADH • 1. Kacprowicz FR, Lloyd JD. Electrolyte Complications of Malignancy. Emerg Med Clin N Am 2009; 27: 257-269. • 2. Yeates KE et al. Salt and Water: a simple approach to hyponatremia. CMAJ 2004; 170: 365-369. • 3. Ellison DA, Berl T. The Syndrome of Inappropriate Antidiuresis. NEJM 2007; 356: 2064-2072. • 4. Verbalis JG et al. Hyponatremia Treatment Guidelines 2007: Expert Panel Recommendations. Am J Med 2007: 120; S1-S21. • EMCrit podcast #39 - Hyponatremia CASE • 58 yr old male with 2 week Hx of • Progressive SOB on exertion • Swelling neck and face • Anorexia and fatigue • No CP, dysphagia • Ex smoker • Exam • HR 105, RR 22, BP 150/95, Sats 93% • Periorbital edema • Dilated veins upper chest Case • What’s your approach? Superior Vena Cava Syndrome • Syndrome caused by extrinsic or intrinsic obstruction of SVC leading to edema and retrograde flow • Not a true medical emergency unless neurologic or respiratory involvement • No formal professional guidelines • Not much data from research SVC - Etiology • Has changed over time 1 • Non-malignant 35% • Thrombosis from intravascular devices • Fibrosing mediastinitis • TB • Aortic aneurysms • Malignant • Lung cancer - Small Cell • Lymphoma - NHL • Metastatic • Others • Germ cell • Thymoma • mesothelioma 65% 90% Wilson LD et al. Superior Vena Cava Syndrome with Malignant Causes. NEJM 2007; 356: 1862-1869. SVC - Presentation • Swelling/Edema 2 • Facial/neck 82% • Arms 68% • Plethora/cyanosis • Dyspnea/orthopnea 66% • Cough 50% • Dilated chest veins 38% • Indicates development of collateral circulation and hence a slowly progressing chronic disease process over weeks • Chest pain • Hoarseness • Headache • Worrisome symptoms • Confusion/ obtundation • Cerebral edema • Stridor • Laryngeal edema SVC - Presentation • Influenzed by • Location of obstruction wrt azygous vein • More severe if obstruction below azygous vein as collaterals can’t drain via azygous • Rapidity of onset of obstruction • Collateral vessels take several weeks to dilate in order to accommodate retrograde flow from SVC • SVC before (above) and after (below) stent Figure 1 Photographs of the patient showing the reduction in swelling of the face, neck and upper extremities Chee CE et al. (2007) Superior vena cava syndrome: an increasingly frequent complication of cardiac procedures Nat Clin Pract Cardiovasc Med 4: 226–230 doi:10.1038/ncpcardio0850 Superior Vena Cava Syndrome Diagnosis • Clinical • CXR • 85% have abnormal CXR 2 • Mediastinal widening • Pleural effusion • CT with contrast • Cause of obstruction • Level and extent of blockage • Evaluation of collaterals CXR Wan JF, Bezjak A. Superior Vena Cava Syndrome. Emerg Med Clin N Am 2009; 27: 243-255. CT Wan JF, Bezjak A. Superior Vena Cava Syndrome. Emerg Med Clin N Am 2009; 27: 243-255. SVC Treatment • Tissue diagnosis required first • Unless acute airway compromise (laryngeal edema) or neurologic decline (cerebral edema) • Treatment will vary dependent on: • Diagnosis • Extent of disease • Severity of symptoms • Prognosis SVC Treatment • Chemo • Lymphomas • Small cell lung Ca • Germ cell tumors • Radiation • Lung Ca • Stent • Provides rapid relief • Can be used prior to tissue diagnosis if severe symptoms • Very rarely surgical SVC Treatment • Adjunctive therapy for symptom relief • Head of bed elevated • O2 • Steroids • Dexamethasone 4mg bid-qid • Often recommended for reduction edema but no data • Risk of obscuring pathology results if given before biopsy • Diuretics • Transient symptomatic relief but avoid hypovolemia • Anticoagulation • Only if demonstrable thrombus on imaging SVC Syndrome • Prognosis • Quite variable dependent on cancer • Usually indicates advanced disease • Median life expectancy: 6 months Summary • SVC syndrome • Not an emergency unless neuro or airway involvement • CT • Tissue diagnosis req’d to guide treatment References – SVC Syndrome • 1. Wilson LD et al. Superior Vena Cava Syndrome with Malignant Causes. NEJM 2007; 356: 1862-1869. • 2. Wan JF, Bezjak A. Superior Vena Cava Syndrome. Emerg Med Clin N Am 2009; 27: 243-255. Case • 75 yr old male currently receiving chemo for non small cell lung CA • Presents with • SOB • Minimal chest discomfort • Small cough and sputum • No fever • No leg swelling Case • PMHx • Non small cell lung CA • Ex smoker with COPD • No Cardiac History • Exam - HR 135, BP 115/80, RR 28, O2 sat 89% R/A • No JVD • Wheezy ++ • No leg swelling/tenderness What’s your approach? What’s your approach? Malignant Pericardial Effusion • Frequently undiagnosed in cancer patients • 10%-15% of cancer patients at autopsy will have some degree of pericardial effusions • Prognosis poor • Most die within 1 yr Malignant Pericardial Effusion & Tamponade • Etiology • Most common • Metastatic lung or breast • Others • Malignant melanoma • Leukemia • Lymphoma • Post chest radiation • Chemotherapeutic agents Malignant Pericardial Effusion S&S • Symptoms • Asymptomatic • Dyspnea/Orthopnea • Palpitations • Chest pain • Anxiety • Fatigue/dizziness • Signs Malignant Pericardial Effusion • Spectrum of S&S from mild to tamponade to arrest • Severity depends on • Accumulated fluid volume • Rate of fluid accumulation Malignant Pericardial Effusion • Diagnosis • CXR • EKG • Echocardiogram • CT • MRI CXR in Pericardial Effusion Heart is globular or “water bottle” shaped ECG in Pericardial Effusion Sinus tachycardia Low voltage Electrical alternans < 1cm = small > 1cm = large Malignant Pericardial Effusion • Treatment • None if asymptomatic • Pericardiocentesis • Usually done by cardiology unless in arrest or imminent arrest situation • Classic blind pericardiocentesis • Up to 6% mortality (Tintinalli) • Pericardial window or drain • Reaccumulation prevented by • Chemo • Radiation • sclerosis Summary Malignant Pericardial Effusion • Cancer patients with SOB, Chest pain, tachycardia, hypotension • Go and get the Ultrasound machine Case • 72yr old male • Dx: Colon Ca with mets to bone and liver • Pain has been well controlled until last 2 days • Fentanyl patches 100mcg/hr X3 • Breakthrough pain • Hydromorphone 20 mg po q2h prn • Has used 5 doses in 24 hrs • Celebrex 100mg q 12h • Severe pain left femur • 10/10 Case • How will you treat his pain? Types of pain • Nociceptive • Somatic eg bone mets • sharp, aching • localized • Visceral • dull, cramping • +/- intermittent • poorly localized • More responsive to opioids • Neuropathic • Nerve Injury Cancer Pain Emergency • Severe, sustained episode of excruciating pain • Pain > 7/10 • Sustained for hours • Escalating for hours or days • Search for cause Cancer Pain Emergency • Causes • Breakthrough • Mechanical • Pharmacokinetic • Concurrent medical/surgical process • Perforated viscus • Abscess • Progression of underlying malignancy • Prefracture of weight bearing bone • Epidural cord compression Cancer Pain Emergency • Management • Rapid upward titration of analgesic until effective dose found • IV route • SQ if IV not accessible • Which drug? • Use same opioid patient is tolerating • Switch opioid if opioid toxicity • If opioid-naive use morphine Cancer Pain Emergency • Management • Which dose? • Give 5% of 24 hr parenteral morphine equivalent dose • If opioid-naive • Morphine 0.1 mg/kg IV • Give IV as infusion over 15 min Case • 72yr old male • Dx: Colon Ca with mets to bone and liver • Pain has been well controlled until last 2 days • Fentanyl patches 100mcg/hr X3 • Breakthrough pain • Hydromorphone 8 mg po q2h prn • Has used 5 doses in 24 hrs • Celebrex 100mg q 12h • Severe pain left femur • 10/10 Cancer Pain Emergency • Repeat doses • Reassess pain • 15 min after IV infusion complete (30 min after SQ) • If pain > 7/10, double the dose • If pain responds, but inadequate relief, repeat same dose • Continue upward titration until analgesia or toxicity Cancer Pain Emergency • Complications • Respiratory depression in patients with excruciating pain is very low • Continued presence of severe pain despite a bolus of morphine predicts the dose can be safely doubled Summary • Cancer pain crisis • First dose : 5% of 24 hr parenteral dose • Repeat doses: double dose if severe pain persists • Look for causes References • 1. DeSandre PL, Quest TE. Management of Cancer-Related Pain. Emerg Med Clin of N Am 2009; 27: 179-194. • 2. Hagen NA et al. Cancer Pain Emergencies: A Protocol for Management. Journal of Pain and Symptom Management 1997; 14: 45-50. • 3. Dr Ed Fitzgibbon, ORCC palliative care 2001. Case • 59 yr old male in urgent care at General • 5 weeks of daily vomiting • Initially had headaches which sounded quite benign and have now resolved • No abdo pain, diarrhea, blood, fever • Feels weak, lost 17 lbs • PMed Hx: Nil - Oh yeah, I had melanoma 7 yrs ago • Vitals all normal • Exam unremarkable, except Brain Metastasis • Up to 25% of pts dying of cancer • Most common primaries • Lung • Breast • Melanoma • Others • May be initial presentation • Hematogenous spread • 90% supratentorial Brain Metastasis • Clinical features result from • Direct destruction of tissue • Compression of tissue by • Metastasis • Tumor-associated brain edema • Disruption of BBB and increased capillary permeability • Compromise of vasculature or CSF flow • Clinical presentations • Increased ICP • Seizures • Focal neuro deficits Increased ICP • Headache • Not in all pts • Classic description of brain tumour headache • “Rare to nonexistent” 1 • Often nondescript • Nausea & vomiting • Visual changes • Papilledema • 8% of malignant glioma pts at presentation • Mental status deterioration • Herniation & death Increased ICP - Treatment • Corticosteroids • Dexamethasone • Most lipid soluble of all the steroids • 70-80% of patients will have symptomatic improvement • Onset effect in few hours • Maximal effect 24-72 hrs • Non-emergent situation • 6-24 mg/day, divided bid to qid • Impaired LOC, rapidly progressive signs ICP, herniation • 40-100mg IV bolus • Maintenance 40-100 mg/day divided doses Increased ICP - Treatment • Hyperventilation • To pCO2 of 30 mm Hg • Causes cerebral vasoconstriction • Temporizing measure only • Concerns • Decreases flow to watershed areas • Decreases cerebral perfusion pressure Increased ICP - Treatment • Hyperosmolar agent: Mannitol • Creates osmotic gradient that draws water from extracellular space into blood • 0.5 – 2.0 g/kg IV loading dose (usually 1 g/kg) of 20% mannitol • Onset action 15-30 min • Duration action few hours • ?role for hypertonic saline • Head of bed to 300 and avoid flexion/extension of neck to maximize venous outflow Increased ICP • Definitive Treatment • Whole brain radiation • Neurosurgery • Stereotactic radiosurgery • Dependent on • Pt/family wishes • Number of mets • Status of primary • Overall condition of patient Summary • Brain Mets • High index of suspicion with Cancer pt (esp lung, breast, melanoma) and headache, neuro changes, seizure • Decadron +/-Mannitol • Radiation oncology vs NeuroSx References • 1. Damek D. Altered Mental Status, Seizures, Acute Stroke, Leptomeningeal Metastases and Paraneoplastic Syndrome. Emerg Med Clinics of N America 2009; 27: 209-229. • 2. Glauser J. Oncologic Emergencies. Emergency Medicine Reports 2009; 30(8) • 3. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81: 835-848. Hyperviscosity Syndrome • Impaired blood flow due to increased intrinsic resistance of fluid to flow • Acellular fraction : protein • Cellular fraction • Results in • Sludging • Decreased perfusion of microcirculation • Vascular stasis Hyperviscosity Syndrome • Abnormal plasma proteins • Waldenstrom macroglobulinemia (IgM) • IgA myeloma • Term “Hyperviscosity Syndrome” best reserved for hyperproteinemias • Abnormal cells • Leukocytosis • Leukemias with WBC > 100,000 • Erythrocytosis • Thrombocytosis Hyperviscosity Syndrome Symptoms • Classic Triad • Bleeding • Visual disturbances • Focal Neurologic signs • Hyperleukocytosis • Dyspnea common Halfdanarson. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006; 81: 835-848. Hyperviscosity Syndrome • Lab • Cell line abnormalities • CBC • Smear • Rouleaux formation Rouleaux formation Hyperleukocytosis in the setting ofAML Hyperviscosity Syndrome • Lab • Hyperproteinemia • Proteinuria • Protein electrophoresis • Serum viscosity high • Normal serum viscosity < 1.8 centipoise • Symptomatic HVS >3 centipoise • Water = 1 cp • Measured by viscosimeter Hyperviscosity Syndrome • Treatment • Supportive • Judicious fluid resuscitation • Avoid diuretics • Avoid pRBC transfusions • Hematology consult • Plasmapheresis or Leukapheresis • If not available • Phlebotomy of aliquots of 100-200 mL Hyperviscosity Syndrome • Emergency Plasma Exchange • Temporizing measure with severe HVS from hyperproteinemia • Seizure or coma • Phlebotomize between 1-2 units of blood and replace volume with NS Summary • Hyperviscosity • Classic triad: bleeding, visual disturbances, focal neuro deficit +/- dyspnea • Plasmapheresis/Leukapheresis References • 1. Glauser J. Oncologic Emergencies. Emergency Medicine Reports 2009; 30(8). • 2. Halfdanarson TR et al. Oncologic Emergencies: Diagnosis and Treatment. Mayo Clin Proc 2006: 81: 835-848. • 3. Adams BD. Myeloproliferative Disorders and the Hyperviscosity Syndrome. Emerg Med Clin N Am 2009; 27:459-476. Summary • Hematologic Crises • Febrile Neutropenia • Hyperviscosity syndrome • Compressions & Obstructions • Malignant Spinal Cord Compression • SVC Syndrome • Malignant Pericardial Effusion • Brain Mets • Metabolic Crises • Hypercalcemia • Tumor Lysis Syndrome • Hyponatremia & SIADH • Pain Crisis Mandatory parameters ("T", "N", and "M")[2] ■T: size or direct extent of the primary tumor ■Tx: tumor cannot be evaluated ■Tis: carcinoma in situ ■T0: no signs of tumor ■T1, T2, T3, T4: size and/or extension of the primary tumor ■N: degree of spread to regional lymph nodes ■Nx: lymph nodes cannot be evaluated ■N0: tumor cells absent from regional lymph nodes ■N1: regional lymph node metastasis present; (at some sites: tumor spread to closest or small number of regional lymph nodes) ■N2: tumor spread to an extent between N1 and N3 (N2 is not used at all sites) ■N3: tumor spread to more distant or numerous regional lymph nodes (N3 is not used at all sites) ■M: presence of metastasis ■Mx: distant metastasis cannot be evaluated ■M0: no distant metastasis ■M1: metastasis to distant organs (beyond regional lymph nodes) [edit]