This would be title slide - University of Mississippi Medical Center
advertisement

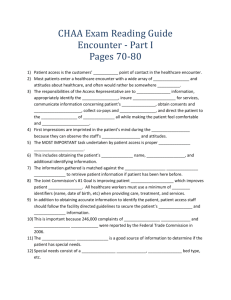
CHAA Examination Preparation Encounter - Session I Pages 70-80 University of Mississippi Medical Center What to Expect… • This module covers various aspects of Patient Access knowledge found in pages 7080 of the ENCOUNTER section of the 2010 CHAA Study Guide. • A quiz at the end will measure your understanding of the content covered. Patient Access Roles in a Nutshell • • • • • • The Basic Responsibilities of a Registrar are to: Gather information to identify the patient and insure reimbursement for services Communicate required complex information to patient regarding patient rights, HIPAA, Advanced Directives, and medical necessity Obtain consents and authorizations Collect co-payments and deductibles Direct the patient to the point of service And do so in a way that makes the patient feel comfortable and important The Encounter • First Impressions are made during the encounter. • First impressions are lasting impressions. This important time can make or break the entire visit. • Customers observe staff behaviors and attitudes and will be quick to determine if they are important to you or not. Patient Identification • THE MOST IMPORTANT TASK UNDERTAKEN BY PATIENT ACCESS IS PATIENT IDENTIFICATION! • Gathering the patient’s legal name and birthday allows you to check this info against the existing Master Patient Index (MPI) to determine if the patient has been to your facility before. • THE #1 GOAL OF THE JOINT COMMISSION’S NATIONAL PATIENT SAFETY GOALS IS IMPROVING PATIENT IDENTIFICATION. Patient Identification • All healthcare workers must use a minimum of TWO identifiers when providing care, treatment, and services. • Securing the patient’s demographic and financial information is also crucial due to the rise of identity theft and insurance fraud over the past few years. Special Needs of the Patient • Special Needs refer to anything from needing a private room to a large wheelchair for obese patients. • According to the Americans with Disabilities Act, hospitals are required to communicate effectively with patients, family members, and VISITORS who are HARD OF HEARING. • They must also take REASONABLE STEPS to provide meaningful access to a person with Limited English Proficiency (LEP). Special Needs of the Patient • At point of first contact, patient access staff must identify communication barriers not only for patients, but for FAMILY MEMBERS and VISITORS. • The PHYSICIAN ORDER is a good source of information on determining special needs. Special Needs of the Patient • The Joint Commission requires hospitals to establish a FALL REDUCTION program that includes an evaluation of the physical environment, as well as staff, patient, and family education. • Patient Access staff should be aware of the environment and actively communicate potential hazards to the appropriate department. Patient Placement • Also known as bed control or bed management, this is the process of providing the patient with the most APPROPRIATE LOCATION and level of service necessary for OPTIMUM CLINICAL CARE. • Special consideration should be given to infection control when assigning the appropriate bed. Infection Control • Patients who require contact precautions should be placed in a single patient room when available. • When that’s not available, patients with the same MRSA should be placed in the same room or patient care area. • MRSA is a type of bacteria resistant to certain antibiotics and is common in hospitals with large numbers of people with weakened immune systems. Infection Control Standard Precautions The Centers for Disease Control and Prevention (CDC) RECOMMEND the following precautions for infection control: 1. Hand Hygiene 2. Cough Etiquette 3. The use of Personal Protective Equipment (PPE) for staff when exposure to blood, body fluids, secretions, etc. is anticipated. Infection Control Standard Precautions • An ALCOHOL BASED rub is the preferred method of hand decontamination if hands aren’t soiled (If hands are soiled, use soap and water first). • Personal Protective Equipment (PPE) is specialized clothing or equipment worn by an employee for protection against infectious materials. • The Occupational Safety and Health Administration (OSHA) issues REGULATIONS for workplace and safety. Levels of Care • Acute Care – medical attention given to patients with conditions of sudden onset that demand urgent attention or care of limited duration when a patient’s wellness would deteriorate without treatment. • Acute Inpatient Care – a level of health care delivered to patients experiencing acute illness for generally less than 30 days. Levels of Care • Observation Care – services furnished by a hospital to monitor a patient’s condition to evaluate the need for a possible admission. Usually doesn’t exceed 24-48 hours. • Ancillary Services – scheduled or non-scheduled services such as radiology, laboratory, or other services. • Emergency Services – patients examined on an unscheduled emergent basis for immediate treatment in the emergency facilities of a hospital. Levels of Care • Ambulatory/Same Day Surgery – surgical treatment that patients receive from a facility and are discharged within 4 to 6 hours of procedure. • Long Term Care – care generally provided to the chronically ill or disabled in a nursing facility or rest home. Medicare beneficiaries are eligible for 100 days and Medicaid coverage is available for those who have exhausted their resources. Levels of Care • Respite Care – allows families caring for physically dependant members time off in their care giving responsibilities. NOT REIMBURSABLE under Medicare or Medicaid. • Hospice – this is a support system to patients with less than 6 months to live who choose to spend their remaining days in the comfort of their own home or hospice designated facility. • Pallative Care – medical treatment specially focused on the relief of the pain and symptoms of a serious illness. Collecting Demographic Information • Demographic Information is defined as patient identifying and contact information. • Gathering and entering this has both clinical and financial purposes. • Examples of Demographic Info: legal name, birthdate, SSN, address, phone number, employer, employer contact info, emergency contact/next of kin. • Verify Demographic info by obtaining positive identification and by using open ended questions during a verbal interview. Explaining and Obtaining Consents • Consent refers to the various forms and signatures involved in registering patients. • Either the patient or the patient representative is required to sign consent forms which should be explained to them beforehand. • Most consent forms include basic consent for treatment and usually a consent that authorizes the provider to release information for financial purposes. • Patient Access Representative may also have to sign form as a witness. Emergency Room Consents • IMPLIED CONSENT BY LAW states that when a patient’s condition prevents them from signing the form and no patient representative is present, the patient access employee may document on the form and sign as a witness. • In this situation, it is important to follow up to obtain written consent with the patient or the patient representative (EXPLICIT CONSENT). Consent Regarding Minors • Consent must be gained from parents or guardians of a minor when providing NON-EMERGENT services. • If a minor presents for NON-EMERGENT services without parent or guardian, the staff member may contact the parent/guardian by phone to obtain verbal consent. This needs to be documented on the consent form. • Some facilities may require a second staff member to verify and document as well. Consent Regarding Minors • In some states, certain services do not require consent from a parent or legal guardian. These include: – Pregnancy Related Services – Contraceptive/Sexually Transmitted Disease services – Mental Health Services – Substance Abuse Services – Emancipated Minors for any service Emancipated Minors • In most states there are three circumstances in which a minor becomes emancipated. These are: – Enlisting in the Military – Getting Married – Obtaining a court order from a judge In most instances, legal documentation is required as proof minor emancipation HIPAA Privacy Notice • The Notice of Privacy Practices (NPP/NOPP) is a document that explains how Protected Health Information (PHI) is used and disclosed by a healthcare entity. • A signed NPP acknowledges that the information was offered to the patient. • The NPP remains in effect for subsequent visits and has to be SIGNED ONLY ONCE, unless the Notice changes. The Patient Self-Determination Act (PSDA) • This act affords patients the right to participate in their own healthcare decisions, including the right to receive or refuse treatment. • Patients have the right to file a complaint or grievance at ANY TIME during the healthcare encounter. • An Advance Directive or Living Will is written instructions regarding patients’ wishes when they cannot make healthcare decisions themselves. The Patient Self-Determination Act (PSDA) • A Durable Power of Attorney for Healthcare is the portion of the Advance Directive where the patient appoints a proxy to make medical decisions on their behalf if they become unable to during treatment. • While the ENCOUNTER SETTING isn’t the ideal place to initiate an Advanced Directive, the PSDA requires that patients be educated regarding what an Advanced Directive is and asked if they have completed one. • An Advanced Directive becomes active when a patient becomes incapacitated and can be revoked at any time by destroying all copies. The “Important Message from Medicare” Form • This form must be presented to ALL MEDICARE PATIENTS prior to admission and re-presented to them within 48 hours of discharge. • It explains Medicare beneficiary rights under law regarding filing an appeal in the event they disagree with the discharge plan or if they have a complaint about the care they received. • The main idea is that the patient has the right to file an appeal before discharge occurs.