Ultrasound: AAA
advertisement

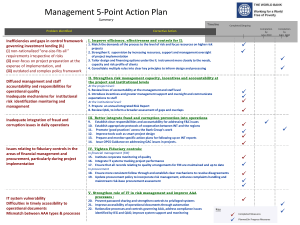
FOCUSED EMERGENCY ULTRASOUND: EVALUATION OF THE ABDOMINAL AORTA MARY BETH PHELAN, MD, RDMS DEPARTMENT OF EMERGENCY MEDICINE FOREDTERT MEMORIAL HOSPITAL Lecture Objectives Describe clinical role of bedside ultrasound in screening for AAA Describe the technique of acquiring sonographic images of the aorta Describe the sonographic appearance of the normal aorta Describe the sonographic appearance of AAA SAEM 2 Case History A 62-year-old man comes to the emergency department at 11PM complaining of left flank pain for approximately 2 hours. He has a history of hypertension. His initial vital signs are: HR 98, RR 24, BP 190/105, Temp 98.0. SAEM 4 Case History The emergency medicine resident equipped with the latest in emergency medicine ultrasound technology and training, IMMEDIATELY performs an abdominal ultrasound on the patient. This exam reveals the following: SAEM 5 SAEM 6 Case History The patient is taken to the OR after only 30 minutes in the ED. SAEM 7 OVERVIEW Epidemiology Clinical presentation Anatomy US exam Sonographic anatomy Scanning techniques Pitfalls Epidemiology AAA present in 2-4% of the population > 50 Incidence increasing Male > female 10,000 deaths/yr Rupture has a > 80% mortality rate Epidemiology: Risk Factors Cardiovascular disease Family History increases risk 10-20% Age > 50 Smoker Clinical Perspective Settings in which to perform US in the ED – Abdominal/back/flank pain and hypotension – Stable elderly patient with abdominal or back pain SAEM 11 Clinical Perspective Rate of expansion variable – 4-4.9 cm AAA has a 3.3% risk of rupture – 5cm AAA has a 14% risk of rupture – > 5cm has a 20-40% risk of rupture Clinical Perspective 4cm or less: annual US examinations Between 4-5 cm: US every 6 months Greater than 5cm: Elective repair Mortality rate for elective repair is 5% Clinical Presentation Highly variable Classic triad: – Abdominal/Back pain – Pulsatile mass – Hypotension Less than 1/3 of patients will have the triad Clinical Presentation Diagnosis – A formidable clinical challenge – Notorious for masquerading as renal colic – May be mistaken for: Diverticullitis GI bleed MI Musculoskeletal back pain SAEM 15 Clinical Presentation Stable vital signs Back or flank pain, left side > right Testicular or leg pain Hypertension Mortality rate same as elective repair Clinical Presentation Vast majority are retroperitoneal 10 -30 % intraperitoneal GI bleeding most often seen in patients with aortic grafts Mortality 50% Does this patient have an abdominal aortic aneurysm?LEDERLE, JAMA 99 2 groups Sensitivity of examination for ruptured AAA Sensitivity of exam with increasing size of AAA CONCLUSION:Cannot be relied on to exclude AAA Misdiagnosis of Ruptured Abdominal Aortic Aneurysms MARSTON W ET AL J OF VASCULAR SURG 1992 Misdiagnosis= delay >6hr or other diagnosis Most common physical findings in misdiagnosed group: ABD PAIN, SHOCK, BACK PAIN Pulsatile mass present more often in correctly diagnosed group SUSPECTED LEAKING ABDOMINAL AORTIC ANEURYSM:USE OF SONOGRAPHY IN THE EMERGENCY ROOM SHUMAN WP, ET AL, RADIOLOGY 88 US IN ED FOR SUSPECTED AAA 1 MIN EXAM CORRECTLY IDENTIFIED 31/32 AAA DECISION TO OPERATE BASED ON 3 CRITERIA CORRECT 21/22 DX EXTRALUMINAL BLOOD BY SONOGRAPHY POOR 4% (1/24) NO FALSE NEG EXAMS Diagnosing AAA Palpation of the abdomen alone Plain radiographs Computed tomography ULTRASOUND Diagnosis: PE Absence of mass does not R/O AAA Obesity Bleeding into retroperitoneum may create doughy abdomen. Hypotension minimizes pulsations Diagnosis: Plain Radiographs AAA can be seen in 60-75% of cases Calcification of aortic wall Paravertebral mass Cross table lateral most helpful view Negative study not helpful Diagnosis: CT Scan Near 100% accuracy Better demonstration of extent of aneurysm Will detect complications of the aneurysm – Retroperitoneal blood – Dissection Drawbacks – Contrast – Patient has to leave the ED – Delays time to diagnosis Diagnosis: US Ultrasound – Best test for detection of AAA in the ED – Sensitivity 97% to 100% – Small percentage can not be imaged due to bowel gas 6% in one study SAEM 25 Diagnosis: US Ultrasound – In some studies as accurate as CT – Measurements within 3 mm of surgical specimens – Angiography may underestimate AAA diameter SAEM 26 Diagnosis: US Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate and advantageous Kuhn et al. Ann Emerg Med 2000 “Relative neophytes can perform aortic ultrasound scans accurately. These scans appear useful as a screening measure in high-risk emergency patients; they may also aide in rapidly verifying the diagnosis in patients who require immediate surgical intervention” SAEM 27 Diagnosis: US ED Ultrasound Improves Time to Diagnosis and Survival in Ruptured AAA Plummer D, et al: Abstract at 1998 SAEM, Chicago, IL. •Average minutes •Average •Average minutes •Average minutes time to diagnosis by bedside US = 5.4 time to diagnosis by CT = 83 minutes time to OR for diagnosis by US = 12 time to OR for diagnosis by CT = 90 SAEM 28 US EXAM Transducer is 2.5-3.0MHz curvilinear Place the transducer in the subxiphoid area, using the left lobe of the liver as an acoustic window Pressure must be applied to displace bowel gas The aorta must be examined in both the longitudinal and transverse planes Longitudinal Orientation Marker Transverse Orientation Marker Orientation is similar to that of a CT scan Position probe is perpendicular to long axis of body or to long axis of object that is being IVC,Liver studied Aorta SAEM 31 US EXAM The aorta appears as an anechoic, pulsatile tubular structure to the left of the spine After the longitudinal scan, the transducer is rotated 90 degrees to the aorta to obtain transverse views. The key landmark in the transverse view is to locate the spinal column as a hypoechoic area at the bottom of the screen. The aorta is located above and to the left of the spine AORTA Left sided structure Thick vascular wall Not compressible Pulsatile IVC Right sided structure Thin wall Will collapse – “Sniff” – Valsalva May pulsate from aortic transmission US EXAM Measure from outside wall to outside wall An aneurysm is identified as any measurement of 3 cm or greater Measure at: – Epigastric region – Take off of SMA – 3-4 cm intervals to bifurcation Measure any aneurysm US EXAM Obesity or excessive bowel gas may obscure the aorta A coronal view of the aorta may be a reasonable alternative The patient is supine The transducer is placed in the mid-axillary line (probe indicator toward the patient’s head) The aorta is visualized adjacent to the vena cava SONOGRAPHIC APPEARANCE OF THE NORMAL AORTA: LONGITUDINAL SONOGRAPHIC APEARANCE OF THE NORMAL AORTA: TRANSVERSE Mid portion Bifurcation SONOGRAPHIC APPEARANCE OF THE NORMAL AORTA (L LATERAL DECUB/CORONAL) ABDOMINAL AORTIC ANEURYSM 90% of AAA are infra-renal 70% involve the renal vessels Thrombus is common, and usually forms on the antero-lateral walls of the aneurysm Two forms – Sacular – Fusiform – most common ABDOMINAL AORTIC ANEURYSM First sign may be loss of normal taper AP diameter > 3CM Focal dilitation even if less than 3 cm Thrombus Intimal flap AORTIC ANEURYSM Large fusiform AAA SAEM 42 AAA with clot SAEM 43 Another AAA with clot SAEM 44 ULTRASOUND EXAM: PITFALLS Bowel gas can be a major problem – Apply pressure – Roll the patient on their left side ( use the liver as an acoustic window) Does not detect complications of AAA – Retroperitoneal rupture – Dissection CT/MRI/angiography for stable patients is still recommended Pitfalls in Technique Failure to acquire high resolution images due to bowel gas Inaccurate measurements – do not measure what you cannot see! Distinguishing the IVC from the aorta Not identifying extraluminal fluid Failing to distinguish the normal “tortuous” aorta from an abdominal aortic aneurysm.