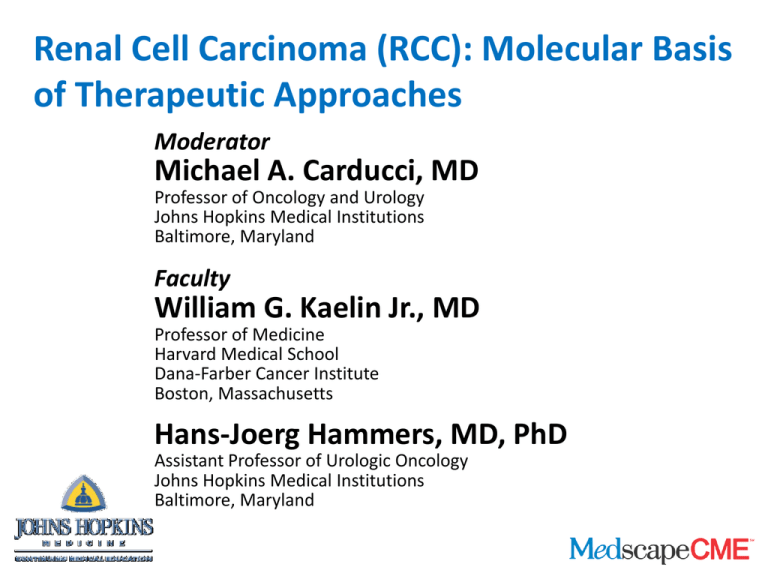
Renal Cell Carcinoma (RCC): Molecular Basis
of Therapeutic Approaches
Moderator
Michael A. Carducci, MD
Professor of Oncology and Urology
Johns Hopkins Medical Institutions
Baltimore, Maryland
Faculty
William G. Kaelin Jr., MD
Professor of Medicine
Harvard Medical School
Dana-Farber Cancer Institute
Boston, Massachusetts
Hans-Joerg Hammers, MD, PhD
Assistant Professor of Urologic Oncology
Johns Hopkins Medical Institutions
Baltimore, Maryland
Overall Goal
The goal of this educational activity is to review the
molecular pathways for choosing therapies based
on the molecular biology of kidney cancer
Role of VHL Gene in RCC
• Inactivation of the VHL tumor-suppressor protein
• Accumulation of HIF transcription factor
• Overexpression of a number of genes, including
VEGF
VHL = von Hippel Lindau; HIF = hypoxia-inducible factor; RCC = renal cell cancer;
VEGF = vascular endothelial growth factor
Review of Published Literature - VHL Gene
Inactivation
Study
VHL gene mutation VHL gene mutation
in clear-cell RCC
in nonclear-cell RCC
Gnarra,[a] 1994
57% (63/110)
Not reported
Shuin,[b] 1994
56% (22/39)
0% (0/8)
Gallou,[c]1999
56% (73/130)
0% (0/21)
Schraml,[d] 2002
34% (38/113)
Not reported
Yao,[e] 2002
52% (98/187)
Not reported
van Houwelingen,[f]
2005
61% (114/187)
15% (7/48)
aGnarra
JR, et al. Nat Genet. 1994;7:85-90. bShuin T, et al. Cancer Res. 1994;54:2852-2855.
cGallou C, et al. Hum Mutat. 1999;13:464-475. dSchraml P, et al. J Pathol. 2002;196:186-193.
eYao M, et al. J Natl Cancer Inst. 2002;94:1569-75. fvan Houwelingen KP, et al. BMC Cancer. 2005;5:57.
VEGF and mTOR Inhibitors
VEGF inhibitors
• Bevacizumab – Neutralizing antibody against VEGF
• Sunitinib
• Sorefenib
• Pazopanib
Small molecules inhibitors
against the VEGF receptor, KDR (VEGF-R2)
mTOR kinase inhibitors
• Temsirolimus
• Everolimus
KDR = kinase domain receptor; mTOR = mammalian target of rapamycin
VEGF Correlated With Poorer Overall Survival
Jacobsen J, et al. BJU Int. 2004;93:297-302.
VEGF Signaling Mechanisms
Antibodies to VEGF
or VEGFR
mTOR
inhibitors
Tyrosine kinase inhibitors
Erk = extracellularly regulated kinase; MAPK = mitogen-activated protein kinase;
MEK = MAP/Erk kinase; PKB = protein kinase B; VEGFR = VEGF receptor
Adapted from Rini BI, et al. J Clin Oncol. 2005;23:1028-1043.
Relationships Between VHL and mTOR
• Direct relationship between VHL loss and increased
VEGF activity
• mTOR indirectly affects HIF and VEGF
• Not clear which mTOR activities are relevant to
kidney cancer
• Inhibition of mTOR with rapamycin-like drugs can
activate upstream kinases
Roles of VEGF and mTOR Inhibitors
RAPTOR
mTOR
HIF
Temsirolimus
Everolimus
Transcription/Synthesis
pVHL
Destruction
HIF
HIF
Cancer Cell
Bevacizumab
Sunitinib
Sorafenib
Pazopanib
VEGF
Extracellular Space
KDR
Endothelial Cell
RAPTOR
PI3K
Courtesy of William G. Kaelin Jr., MD
AKT
mTOR
Temsirolimus
Everolimus
Effectiveness of Current Therapies
VEGF inhibitors as monotherapy are not curative
Combination therapies
• Must have different mechanisms of action
• Should not be cross-resistant
Ongoing clinical trials address
• VEGF inhibitors with mTOR inhibitors
– Bevacizumab, sorafenib, and temsirolimus in patients with
metastatic RCC[a]
– Everolimus and vatalanib in treating patients with advanced solid
tumors[b]
– Phase 1b, open-label, dose-finding study to evaluate the safety
of tivozanib (AV-951) in combination with temsirolimus in
subjects with metastatic RCC[c]
aClinicaltrials.gov.
Available at: http://clinicaltrials.gov/ct/show/NCT00378703
Available at: http://clinicaltrials.gov/ct/show/NCT00303732
cClinicaltrials.gov. Available at: http://www.clinicaltrials.gov/ct2/show/NCT00563147
bClinicaltrials.gov.
Questions That Remain Unanswered
• Is the combination of these agents actually adequate
for all patient populations?
• Can we stratify patients to these treatments with
some patient groups benefiting more from the
combinations than others?
• What are the potential mechanisms of resistance to,
for example, VEGF-based agents?
• Will combinations with mTOR inhibitors break this
resistance?
Targets: HIF-Responsive Gene Products
Pazopanib
CA = carbonic anhydrase; c-Met = mesenchymal-epithelial transition factor; CTGF = connective
tissue growth factor; CXCR = CXC chemokine receptor; HDAC = histone deacetylases; MMP =
matrix metalloproteinase; PDGF = platelet-derived growth factor; pVHL = VHL protein; SDF =
stromal cell-derived factor; TGF = transforming growth factor
Kaelin WG Jr. Cancer. 2009;115(10 Suppl):2262-2272.
Inhibition of TORC1 and TORC2 Complexes
Extracellular
RTK
Intracellular
RICTOR
PI3K
mTOR
AKT
Torc2 complex
(rapalog
insensitive)
Additional oncogenic functions
RAPTOR
mTOR
Torc1 complex (rapalog
sensitive)
Temsirolimus and everolimus are rapalogs
HIF
Courtesy of William G. Kaelin Jr., MD
pVHL Activity in Physiologic and
Pathologic States
Rathmell WK, Chen S. Exp Rev Anticancer Ther. 2008;8:63-73.
Molecular Pathways and Targeted Therapies
PDGFR = PDGF receptor; PTEN = phosphatidylinositol phosphate 3'phosphatase; FKBP = FK binding protein; TSC = tuberous sclerosis complex
Brugarolas J. N Engl J Med. 2007;356:185-187.
Responses With High-Dose IL-2
US Food and Drug Administration-approved highdose IL-2
• Durable responses in carefully selected patients
• Toxic
• Substituting with lower dose or adding interferon produced
fewer tumor regressions
Predictors of response to IL-2 therapy
• Patients with clinical features of a good or intermediate
prognosis
• Tumors with clear-cell histology
IL = interleukin
McDermott DF. Clin Cancer Res. 2007;13:716s-720s.
Immunologic Agents in Clinical Development
• Antibodies to CTLA4
– Phase 2 study with iplilimumab[a]
– Response was 4% to 27% by RECIST in IL-2 nonresponders
• Antibodies to PD1
– Phase 1/2 trial of MDX-1106 in solid tumors
– Clinical activity against RCC and melanoma with
intermittent dosing at 10 mg/kg
– No serious toxicity
CTLA4 = cytotoxic T-lymphocyte-associated protein 4; RECIST = response evaluation
criteria in solid tumors
aYang
JC, et al. J Immunother. 2007;30:825-830.
bBrahmer JR, et al. J Clin Oncol. 2009;27(15s):3018.
MET in RCC
• MET signaling has been shown to be important in
RCC[a]
• MET can cooperate with epidermal growth factor
receptor[b]
• MET mutations drive the pathology in hereditary
papillary kidney cancer[a]
• Papillary kidney cancer is an ideal RCC tumor for the
study of MET-targeted therapies[a]
• The rational design and development of MET
inhibitors has produced a number of potent and
selective agents[a]
• MET is an HIF target gene and therefore a potential
target in clear-cell RCC[a]
aGiubellino
A, et al. Expert Rev Anticancer Ther. 2009;9:785-793.
bInoue K, et al. Virchows Arch. 1998;433:511-515.
MET Signaling Pathway
GRB = growth factor receptor binding protein; PLC = phospholipase C
Abounader R, et al. Oncogene. 2004;23:9173-9182.
Potential Predictors of Outcome
• Histology: Tyrosine kinase inhibitors promise longer
progression-free survival in clear-cell histology
• Clinical prognostic factors combined with histologies
can help guide treatment selection in poor-risk
patients
– Poor-risk patients can also benefit from tyrosine
kinase inhibitors
Waterfall Plots of Primary Tumor Responses:
Size Response to Sorafenib Therapy
Response evaluation criteria in solid tumors: partial response criteria designated by lower
dashed line at −30% and progressive disease criteria designated by upper dashed line at 20%.
LD = longest dimension
Cowey CL, et al. J Clin Oncol. 2010;28:1502-1507.
Axitinib Treatment for Cytokine-Refractory
mRCC: Phase 2 Study
Axitinib - Investigational KDR inhibitor
Maximum percentage of tumor decrease for target lesions by RECIST
Zero represents baseline (no change), -100% represents potential complete response,
~ 30% represents potential partial response
Rixe O, et al. Lancet Oncol. 2007;8:975-984.
Improving Response?
• Does HIF-1-alpha status affect the response to VEGF
inhibitors?
• Will the use of a pharmacodynamic biomarker
(hypertension) provide more effective dosing?
• Which VEGF inhibitor has good potential in
combination therapy?
Resistance Mechanisms
• IL-8 contributing to VEGF resistance[a]
• Acquired or transient resistance[b]
aHuang
D, et al. Cancer Res. 2010;70:1063-1071.
bMotzer RJ, et al. J Clin Oncol. 2009;27:3584-3590.
Toxicity of Sunitinib Plus Bevacizumab
Characteristics of patients in whom TMA developed compared with
characteristics of patients with RCC
Characteristic
Index Patient Index Patient Index Patient Other Patients With
1
2
3
RCC (n = 8)
Age
57
60
69
Sex
Female
Male
Male
Median 55
(range, 46-83)
7 male/1 female
Histology
Chromophobe
Clear cell
Papillary
7 clear cell†/1 papillary
Previous
Yes
Yes
Yes
Yes (100%)
nephrectomy
Baseline blood
114/77
140/86
146/80
Median 142/81
pressure, mm Hg
Peak blood
157/102
180/104
190/111
Median 167/99
pressure, mm Hg
Hemoglobin
baseline/nadir,
11.7/9.8
15.7/12.4
15.2/15.2
Median 13.4/12.6
g/dL
TMA = thrombotic microangiopathy; LDH = lactate dehydrogenase; HFS = hand-foot
syndrome; S = sunitinib; B = bevacizumab
Rini BI, Garcia JA. J Clin Oncol. 2010;28:e284-e285.
Toxicity of Sunitinib Plus Bevacizumab (cont)
Characteristic
Index
Patient 1
Index
Patient 2
Index
Patient 3
Other Patients
With RCC (n = 8)*
490/59
273/76
158/72
Median 219/78
Platelet baseline/
nadir, K/μL
Creatinine baseline/
peak, mg/dL
Haptoglobin
baseline/nadir, mg/dL
0.9/1.1
1.3/1.4
1.5/2.2
Median 1.3/1.6
393/< 20
209/< 20
118/< 20
NA†
LDH baseline/peak, U/L
324/392
173/310
585/324
Median 170/396
2.9
2.7
2.2
Peak reticulocyte count, %
Grade 3 toxicity
Tumor burden change, %
NA†
Hypertension: 6 pts
HFS: 3 pts
Hypertension Hypertension
Hypertension Proteinuria: 2 pts
/fatigue
/HFS
Fatigue: 1 pt
Low platelets: 1 pt
Median −39
−48
−36
−66
(range, −4 to −73)‡
*Dose levels for other patients with RCC included S 25 mg/B 5 mg/kg (1 pt), S 37.5 mg/B 5 mg/kg (3 pts), S
37.5/B 10 mg/kg (1 pt), and S 50 mg/B 10 mg/kg (3 pts). † Two pts with papillary features and 1 pt with
sarcomatoid features. ‡ Baseline haptoglobin and reticulocyte count not be measured in the majority of
patients enrolled in initial cohort. No patient with haptoglobin < 20 on any measurement.
§ Two pts unevaluable due to lack of postbaseline scans.
Rini BI, Garcia JA. J Clin Oncol. 2010;28:e284-e285.
Adjuvant Therapy for Those at High Risk
for Relapse
There is no evidence for benefit of adjuvant therapy in
clear-cell RCC at this time
• Should it be given before or after nephrectomy?
• Will molecular markers be better able to identify
high-risk patients?
• Adjuvant therapy
– Sunitinib, sorafenib, bevacizumab
– Temsirolimus and everolimus
– Immunotherapy with CTLA-4 and PD-1 antibodies
Bleumer I, et al. Can J Urol. 2006; Suppl 2:57-62.
Jonasch E, Tannir NM. Cancer J. 2008;14:315-319.
de Reijke TM, et al. Eur J Cancer. 2009;45:765-773.
Thank you for participating
in this activity.
To proceed to the online CME test,
click on the Earn CME Credit link
on this page.