LDL-C (mg/dL)
advertisement

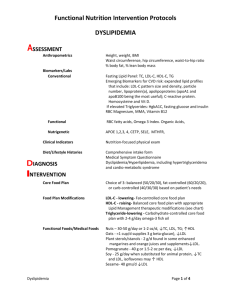
“Lipidology (Pre ATP-IV): Everything I Can Discuss on What You Should Know” How to Prevent a Heart Attack June 12, 2010 Robert H. Eckel, M.D. Professor of Medicine Division of Endocrinology, Metabolism and Diabetes Division of Cardiology Professor of Physiology and Biophysics Charles A. Boettcher II Chair in Atherosclerosis University of Colorado Denver School of Medicine Director Lipid Clinic, University Hospital The Lipid Patient Five Groups • LDL cholesterol • TG ( HDL cholesterol • LDL cholesterol + TG • HDL cholesterol • Lipoprotein (a) Assessing Acquired Causes of Dyslipidemia • Lifestyle – Diet, inactivity, alcohol, tobacco • Medications – Steroids, diuretics, -blockers, PIs, cis-RA • • • • Insulin resistance Thyroid disease Liver disease Kidney disease – Proteinuria – GFR Revised NCEP ATP III LDL-C Goals CHD Risk Category High (Very High) Moderately High Moderate Low Circulation 110:227, 2004 CHD or Risk Equivalent (>20%/10 yrs) 2+ RF (10-20%/10 yrs) 2+ RF (<10%/10 yrs) 0–1 RF’s LDL-C Goal Consider Drug Rx <100 100* (<70) <130 130* <130 160* <160 190* * Consider drug options if below goal, but above goal for next higher risk level Revised NCEP ATP III Non-HDL Goals CHD Risk Category High (Very High) Moderately High Moderate Low Circulation 110:227, 2004 Non-HDL-C Consider Goal Drug Rx CHD or Risk Equivalent (>20%/10 yrs) 2+ RF (10-20%/10 yrs) 2+ RF (<10%/10 yrs) 0–1 RF’s <130 130* (<100) <160 160* <190 190* <190 190* * Consider drug options if below goal, but above goal for next higher risk level NHLBI Clinical Guidelines for CVD Risk Reduction: Organizational Structure NHLBI Director Guideline Leadership Group DARD Director SAIC Support Contract DARD Project Team Clinical Guidelines Executive Committee Cross-Cutting Workgroups Risk Assessment Lifestyle/Nutrition/PA Implementation/System/IT/ Informatics Expert Panel for the Integrated CVD Guideline Development Expert Panel for Cholesterol Updates Expert Panel for Hypertension Updates Expert Panel for Obesity Updates Major Lipids, Apolipoproteins and CVD Risk: The Emerging Risk Factors Collaboration • 302,430 people without CVD from 68 long-term prospective studies – Mostly Europe and North America • 2.79 million person-years of follow-up – 8857 non-fatal MIs – 3928 CHD deaths – 2534 ischemic strokes – 513 hemorrhagic strokes – 2536 unclassified strokes ERF Collaboration, JAMA 302:1993, 2009 CHD Risk: Non-HDL vs. HDL Cholesterol (n = 302,430) ERF Collaboration, JAMA 302:1993, 2009 Apolipoprotein B One apo B molecule/particle Assesses potentially atherogenic particle number Helps to distinguish risk of CHD in patients with hypertriglyceridemia Highly correlated with non-HDL cholesterol • 0.95 when TG < 300 mg/dl • 0.80 when TG higher Apo B May Predict Vascular Events Better than LDL Cholesterol • Observational studies – Quebec Cardiovascular Study – LIPID (placebo) – AMORIS • Interventional studies – – – – AFCAPS/TexCAPS (lovastatin) LIPID (pravastatin) IDEAL (simvastatin, atorvastatin) TNT (atorvastatin) CHD Risk Based on Lipids and Apolipoproteins (n = 91,307) ERF Collaboration, JAMA 302:1993, 2009 The real value of apo B is in patients without increases in LDL cholesterol, in patients with hypertriglyceridemia Impact of TG Levels on Relative Risk of CHD: Framingham Heart Study 3.0 2.5 Men Women 2.0 RR 1.5 1.0 0.5 0.0 50 100 150 200 250 300 350 400 TG (mg/dL) Castelli WP. Can J Cardiol. 4:5A, 1988 Hypertriglyceridemia (1 mM ) and CHD: A Meta-Analysis (21 studies) Relative Risk MEN (65,863): WOMEN (11,089): 1.30 (1.25-1.35) 1.69 (1.45-1.97) Adjusted for HDL cholesterol (9 studies): MEN (29,105): 1.17 (1.10-1.26) WOMEN (6,345): 1.37 (1.13-1.66) Abdul-Maksoud M and Hokanson J.E., J Vasc Med, 2001 Risk of CHD in the Top vs. Bottom Tertile of Usual Log-TG by Study Characteristics Sarwar, N. et al. Circulation 2007;115:450-458 Sarwar N et al, Circulation 115:450, 2007 Apo B and CHD Risk: MetaAnalysis Thompson A and Danesh J, Journal of Internal Medicine, 259:481, 2006 CHD and Ischemic CVA Risk: Emerging Risk Factors Collaboration Meta-Analysis CHD (n = 302,430 people) CVA ERF Collaboration, JAMA 302:1993, 2009 Odds Ratios for the Development of CHD: Lipid and Lipoprotein Phenotypes Odds are adjusted for age, smoking, alcohol, blood pressure, gender, and medications (0.005) (0.001) 3.1 2.7 (0.01) 2.1 (0.001) 2.8 OR 1.7 1.0 1.0 Normal IIA IIB IV Nl TG TG HDL HyperapoB Lamarche B et al, Am J Card 75:1189, 1995 Management of Triglycerides Goal: Is it TG? No, it’s non-HDL cholesterol! Then isn’t it TG < 150 mg/dl? Or should it be apo B? Correlations Between Apo B, Cholesterol, LDL Cholesterol and Non-HDL Cholesterol Sniderman AS et al, Am J. Card 91:1173, 2003 ACC/ADA Lipid Goals CHD or DM + 1 Risk Factor ≥ 2 Risk Factors or DM LDL-C NonHDL-C Apo B < 70 mg/dl < 100 mg/dl < 80 mg/dl < 100 mg/dl < 130 mg/dl < 90 mg/dl Brunzell JD et al, JACC 51:1512, 2008 LDL-C Reduction in Statin Trials 35 Clinical statin trial data iEmax model, r2 = 0.82, p=0.01 30 4S P Event Rate (%) 25 20 4S Tx 15 10 TNT 80 mg CARE Tx HPS Tx LIPID P CARE P HPS P TNT 10 mg LIPID Tx 5 0 0 25 50 75 100 125 150 175 200 LDL-C (mg/dL) Charland SL, et al. Circulation 2005; 112:II-816 Statins: The Down Side • Abnormal AST and ALT – < 3X ULN: ~1.3% – > 3X ULN: <1.0% • Dose related • Myopathy: Any disease of muscles – Myalgias: pain in a muscle of group of muscles • ~10% – Myositis: muscle symptoms with CK • ~2.5% – Rhabdomyolysis: > 50 fold in CK + renal impairment • <0.1% Bruckert E et al, Cardiov Drugs 19:403, 2005 Brown WV, Curr Opin Lipid 19:558, 2008 Onusko E, J Fam Pract 57:449, 2008 What the Clinician Needs to Consider • Hypothyroidism • Other drugs – Fibrates, azole anti-fungals, cyclosporine, macrolides, diltiazem, HIV protease inhibitors • Genetic differences in drug-metabolizing enzymes, e.g. OATP1B1 – SLCO1B1, CYP2D2, 3A4 • Neuromuscular diseases – Mitochondrial myopathy, McArdles disease, myotonic dystrophy, polymyositis Patient Types Diagnostic Strategies CK in high risk patients only Asymptomatic CK measured: < 5 x normal Moderate to Severely Symptomatic Stop Statin: CK measured, hydrate if creatinine ↑ Eckel RH, JCEM In Press, 2010 Titrate Statin Dose to reach LDL and nonHDL-C goals Ezetimibe and/or BAS Symptoms worse: repeat CK & Stop or Reduce Statin Dose Mildly Symptomatic Therapeutic Options Symptoms gone: CK ↓& creat↓ Fluvastatin or pravastatin, 20 mg per night or every other night Fluvastatin XL 80 mg per night Rosuvastatin 5 mg daily, every other day, or weekly Red yeast rice, 600-1800 bid LIPOSORBER® SYSTEM LIPOSORBER® SYSTEM Re-Priming Solution Heparin Pump Regeneration Solution Regeneration Pump Blood Pump Plasma Pump Plasma Separator Blood Return LIPOSORBER® Columns Plasma Line Waste Line LIPOSORBER® SYSTEM LDL-C Diet Therapy Diet & Drug Therapy LIPOSORBER® Treatment Pre Time Average Post Time LIPOSORBER® SYSTEM LONG TERM EFFICACY OF LDL APHERESIS ON CHD IN Familial Hypercholesterolemia Patients Heterozygous FH with CHD Treatment LDL-Apheresis and Medication (n = 43) (Average LDL-Apheresis Interval = 14 days) Medication Only (n = 87) Follow-Up 6 Year Observation of Coronary Events (Non-Fatal MI, PTCA, CABG, CHD Death) Results 72% reduction in Coronary Events for apheresis patients Mabuchi H et al. Am J Card 82:1489, 1998 What about nonstatin approaches in the reduction of LDL cholesterol and CHD? Maintain an Overall Healthy Diet! Dietary Patterns and MI Risk in 52 Countries: INTERHEART 5761 cases 10,646 controls Iqbal R et al, Circulation 118:1929, 2008 Dietary Risk Score (7 components) and MI Risk in 52 Countries: INTERHEART Range of LDL Cholesterol Lowering with Drugs • • • • • Statins 15-60% Bile Acid Sequestrants 5-35% Ezetimibe 15-20% Fibrates 10-25% Nicotinic acid 0-20% Randomized Intervention Trials: Relationship Between LDL-C Reduction and Major Coronary Secondary Events 30 prevention trials Primary prevention trials 4S HPS 25 Major coronary event rate (%) 20 LIPID 15 LRC-CPPT CARE 10 Post-CABG 5 WOSCOPS AFCAPS/ TexCAPS 0 60 80 100 120 140 160 180 200 LDL-C during trial (active treatment and placebo) Modified from Waters DD and Azar RR. Am J Cardiol. 86:35J-43J, 2000. Fox R. Circulation. 2001;104:e9051; Schwartz GG et al. JAMA. 285:1711, 2001 Where are we at on ezetimibe? ARBITER 6-HALTS • “HALTS”: HDL And LDL Treatment Strategies • Purpose – Compare the effectiveness of combination lipid lowering therapy with either extended-release niacin or ezetimibe added to long-term statin therapy for the endpoint of carotid intima-media thickness over 14 months • PROBE Design – Prospective, randomized, parallel-group, open-label study involving blinded evaluation of endpoints • Walter Reed Army Medical Center- Washington, D.C. • Washington Adventist Hospital- Takoma Park, MD Overall Baseline Characteristics • • • • N = 208 80% male Age: 65 ± 11 years All on statins – 42 ± 25 mg/d – 6 ± 5 years duration – 95% simvastatin or atorvastatin Baseline measured variables • TC 147 ± 26 mg/dL • LDL-C 82 ± 23 mg/dL • HDL-C 42 ± 8.5 mg/dL • TG 134 ± 68 mg/dL • CIMT – Mean – Max 0.8977 ± 0.1583 mm 1.0179 ± 0.1653 mm •Baseline characteristics balanced in the 2 treatment groups. •Baseline statin dose: Little room for additional statin titration. Results: Lipid Concentrations Niacin Niacin • Niacin: HDL increased by 18.4% to 50 mg per deciliter • LDL and TG • Ezetimibe: LDL decreased by 19.2%, to 66 mg per deciliter P < 0.001 Ezetimibe P = 0.01 Ezetimibe Niacin Ezetimibe P = 0.001 P = 0.01 Niacin Ezetimibe Δ LDL-C Δ HDL-C Δ TG (median) Ezetimibe −17.6±20.1 mg/dL −2.8±5.7 mg/dL -9 mg/dL Niacin −10.0±24.5 mg/dL +7.5±9.2 mg/dL -36 mg/dL Results: Primary Endpoint Between-group Change in CIMT • Niacin was superior to ezetimibe for the primary endpoint of the between group difference in carotid intima-media thickness. •P = 0.003 Results: LDL Change vs. CIMT Change • In a post hoc analysis, we explored the bivariate relationships between changes in LDL cholesterol levels and mean carotid intima–media thickness. • Ezetimibe R = -0.31; P < 0.001 • Niacin R = -0.01; P = 0.92 Posted online at www.nejm.org • Paradoxical increase in CIMT in patients treated with ezetimibe with greater reductions in LDL cholesterol. This effect was not observed with niacin. Hypothesis generating regarding the net effects of ezetimibe’s complex mechanism of action in patients with dyslipidemia. Results: Major CVD Events Major adverse cardiovascular events occurred at a significantly lower incidence in the niacin (2/160 patients [1.2%] vs. the ezetimibe group (9/165 patients [5.5%]) •Chi-square p=0.04; Log-rank p = 0.047 HDL: So what do we really know? HDL and Atherosclerosis • Anti-oxidant • Anti-inflammatory • Anti-thrombotic – prostacyclin • Promotes vascular reactivity – NOS • Reverse cholesterol transport The HDL Proteome PLTP CETP LCAT ApoC-I ApoC-II ApoM ApoC-III ApoF SERF2 AGT SERF1 ApoC-IV ApoE Lipid Metabolism ApoD Proteinase Inhibitor PON3 SAA4 ApoL-1 SAA2 ApoA-II Clusterin ApoA-IV ApoH PON1 Complement Regulation SAA1 ApoA-I HRP AHSG SERA1 AMP KNG1 Acute Phase Response C3 C4A C4B C9 VTN ORM2 TTR ITIH4 RBP4 TF FGA HPX Vaisar T et al. J Clin Invest. 117:746, 2007 HDL- Paradox • CETP deficient Japanese families with HDL levels • 80-100 mg/dL or higher in heterozygotes • But, possibly an increase in CHD risk • Apo A1Milano • Low HDL octagenarians with low CHD risk • Tangier Disease • ABCA1 gene deficiency • Genetically low HDL: Turkey (HTGL gene mutation) and China • When relocated to an urban environment, CHD risk • Many patients without low HDL have CHD • Pro-inflammatory HDL? • Type 1 diabetes Novel Therapies for Raising HDL • • • • • • Reconstituted HDL Apo A-1 Apo A-1 Milano Apo A-1 peptides PPAR-/ dual agonists New drug classes For HDL, where’s the evidence? Coronary Drug Project 15-Year Mortality Results Niacin Placebo Risk n=1,119 n=2,789 Reduction Total Mortality P 52% 58% -11% <0.005 FBG < 100 mg/dL 48% 53% -9% <0.05 FBG 100 mg/dL 56% 63% -12% <0.005 36% 41% -12% <0.01 CHD Mortality Canner PL et al, J Am Coll Cardiol. 8:1245, 1986. % of Patients with Non Fatal MI CDP - METABOLIC SYNDROME Placebo n = 124 Niacin 30 25 20 69% 15 28% 10 5 0 Metabolic Syndrome (+) Metabolic Syndrome (-) Canner PL et al, Am J Cardiol. 2006 97:477, 2006 CDP - METABOLIC SYNDROME % of Patients (Total Mortality) Placebo n = 368 Niacin 80 70 60 27% 17% 50 40 30 20 10 0 Metabolic Syndrome (+) Metabolic Syndrome (-) Canner PL et al, Am J Cardiol. 2006 97:477, 2006 Niacin and CVD Events in the Metabolic Syndrome: FATS, HATS, AFREGS Zhao XQ et al, Am J Cardiol. 104:1457, 2009 Definitive HDL Cholesterol Outcome Studies • HPS2-Thrive – This study is currently recruiting participants. – Verified by University of Oxford, November 2009 – First Received: April 17, 2007 Last Updated: November 4, 2009 History of Changes – Purpose - The primary aim is to assess the effects of raising HDL cholesterol with extended release niacin/laropiprant vs. matching placebo on the risk of MI or coronary death, stroke, or the need for revascularization in people with a history of circulatory problems. Definitive HDL Cholesterol Outcome Studies • Aim High – Plaque Inflammation and Dysfunctional HDL Cholesterol in Participants Receiving Niacin and Statins in the AIM-HIGH Study (The HDL Proteomics Study) – This study is currently recruiting participants. – Verified and funded by National Heart, Lung, and Blood Institute (NHLBI), April 2009 – First Received: April 10, 2009 No Changes Posted – Purpose: This study will examine MRI images and blood samples of participants who are taking niacin plus statins or statins alone to determine the effect of these medications on inflammation in atherosclerotic plaques. IMPROVE-IT • IMPROVE-IT: – Examining Outcomes in Subjects With Acute Coronary Syndrome: Vytorin (Ezetimibe/Simvastatin) vs. Simvastatin (Study P04103AM3) – clinicaltrials.gov – This study is currently recruiting participants. – First Received: September 13, 2005 Last Updated: December 10, 2009 History of Changes – Primary Outcome: To measure the effect of treatment with ezetimibe/simvastatin compared with simvastatin monotherapy on death due to any CVD events, nonfatal coronary events (i.e. MI), and non-fatal strokes. • Time Frame: Trial will continue until a minimum of 5,250 subjects have a primary endpoint event and each subject is followed for a minimum of 2.5 years. New Non-Statin Therapies for Atherogenic Lipoprotein Lowering • MTP inhibitors • Antisense apolipoprotein B • Thyroid hormone -receptor agonists – Pro-drug targeted to the liver • PCKSK9 inhibitors Lipoprotein (a): What do We Know? Lipoprotein (a) Genotype, Level and CHD Risk Clarke R et al, NEJM 361:2518, 2009 The Lipid Patient: Lipoprotein (a) > 30 mg/dl LDL cholesterol Goal – <160, <130, <100, <70 mg/dl • NCEP-ATP:III – <145, <115, <85, <55 mg/dl • Suggested goal for lipoprotein (a) > 30 mg/dl So What are the Tough Decisions? Question My Opinion LDL-C: How low? Statin Intolerance <100 or < 70 Your choice LDL-C: What drugs? All if needed TG, Non-HDL-C or Apo B in Patients with TG? HDL-C: A target for Rx? Lipoprotein (a)? Apo B ???? > 30 mg/dl, LDL-C by 15 more