ST Segment Changes: Identifying MI Mimics – Leanna R. Miller RN
advertisement

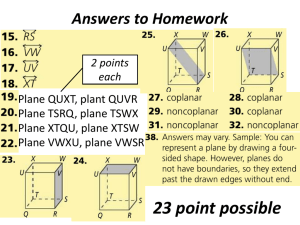
Leanna R. Miller, RN, MN, CCRN-CSC, PCCN-CMC, CEN, CNRN, CMSRN, NP Education Specialist LRM Consulting Nashville, TN ST Segment Changes: Identifying MI Mimics • Objectives – Evaluate common abnormalities that mimic myocardial infarction. – Identify the criteria for pericarditis and evidence – based interventions. – Differentiate between pulmonary embolus and myocardial infarction using diagnostic criteria. ST Segment Changes: Identifying MI Mimics Acute Coronary Syndromes – Unstable Angina – Non ST segment Elevation MI (NSTEMI) – ST segment Elevation MI (STEMI) ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Acute Coronary Syndromes – Clinical Symptoms • typical • atypical ST Segment Changes: Identifying MI Mimics Acute Coronary Syndromes – Diagnostics • Echocardiography • Lab –ABGs –H & H –enzymes ST Segment Changes: Identifying MI Mimics Acute Coronary Syndromes – Diagnostics • ECG (12 or 15 lead) –T wave inversion –ST segment elevation –Q wave –reciprocal ST segment depression ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics SITE INDICATIVE RECIPROCAL Septal V1, V2 None Anterior V2, V3, V4 None Anteroseptal V1, V2, V3, V4 None Lateral I, aVL, V5, V6 II, III, aVF Anterolateral I, aVL, V3, V4, V5, V6 II, III, aVF Inferior II, III, aVF I, aVL, V2, V3 Posterior None V1, V2 ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Variation to ST – Segment Elevation ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics High acute risk factors for progression to myocardial infarction or death – recurrent chest pain at rest – dynamic ST-segment changes: ST-segment depression > 0.1 mV or transient (<30 min) STsegment elevation >0.1 mV – elevated Troponin-I, Troponin-T, or CK-MB levels ST Segment Changes: Identifying MI Mimics High acute risk factors for progression to myocardial infarction or death – hemodynamic instability within the observation period – major arrhythmias (ventricular tachycardia, ventricular fibrillation) – early post-infarction unstable angina – diabetes mellitus ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics AMI LVH BBB Vpace BER Pericarditis LV Aneurysm Other ST Segment Changes: Identifying MI Mimics Acute Pericarditis • Introduction – causes physical discomfort – predisposition to tachydysrhythmias ST Segment Changes: Identifying MI Mimics Acute Pericarditis • ECG Criteria – ST segment elevation – PR segment depression – T wave flattening or inversion – atrial dysrhythmias ST Segment Changes: Identifying MI Mimics Acute Pericarditis • ST segment elevation – not isolated or discrete segments – upward concavity – may be notching at the junction of QRS and ST segment – no reciprocal ST segment depression ST Segment Changes: Identifying MI Mimics Acute Pericarditis • PR interval – interval between end of P wave and beginning of QRS may be depressed – most often seen in lead II and V leads may be only ECG finding ST Segment Changes: Identifying MI Mimics Acute Pericarditis • T wave flattening or inversion – no T wave inversion during acute phase – uncomplicated pericarditis: negative T waves only occur in leads which usually have negative T waves (aVR & V1) ST Segment Changes: Identifying MI Mimics Acute Pericarditis • Atrial dysrhythmias – SVT in postoperative open heart patient – treat with low dose steroids ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Acute Pericarditis • Complications (pericardial effusion) – dampening of electrical output – low voltage in all leads – ST segment & T wave changes ST Segment Changes: Identifying MI Mimics Acute Pericarditis • Complications (pericardial effusion) – freely rotating heart produces electrical alternans ST Segment Changes: Identifying MI Mimics Dressler’s Syndrome • Introduction – postmyocardial infarction syndrome – autoimmune process ST Segment Changes: Identifying MI Mimics Dressler’s Syndrome • Clinical Presentation –low – grade fever –chest pain (worsens with deep breath; lessens with sitting up and leaning forward) –pericardial friction rub ST Segment Changes: Identifying MI Mimics Dressler’s Syndrome • 12 – lead ECG diffuse ST segment elevation across the precordial leads – ST Segment Changes: Identifying MI Mimics Dressler’s Syndrome • Treatment – corticosteroid administration – monitor for complications (effusion) ST Segment Changes: Identifying MI Mimics Pulmonary Embolus • Introduction – sudden massive PE produces ECG changes – must get 12 – lead to rule out MI ST Segment Changes: Identifying MI Mimics Pulmonary Embolus • ECG Findings – RVH with strain – RBBB pattern in V1 – large S wave in Lead I; large Q wave in Lead III (S1Q3 pattern) ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Ventricular Aneurysm • Introduction (etiology) – myocardial infarction – congenital – cardiomyopathy – inflammatory – idiopathic ST Segment Changes: Identifying MI Mimics Ventricular Aneurysm • Introduction – infereolateral wall of LV – symptoms include CHF & exercise – induced syncope (VT) ST Segment Changes: Identifying MI Mimics Ventricular Aneurysm • ECG Findings – persistent ST segment elevation – small q wave in II, III, & aVF – sustained VT with RBBB morphology ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Ventricular Aneurysm • Treatment – surgical resection – antidysrhythmics – anticoagulants – treat heart failure – ablation therapy ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Left Bundle Branch Block (LBBB) • QRS duration > 0.12 second • absence of septal q waves and S wave in I, aVL, & V5 – 6 (+ complex usually notched) • broad QS or rS in V1 – 3 (- complex) ST Segment Changes: Identifying MI Mimics Left Bundle Branch Block (LBBB) • S – T, T wave changes in leads I, aVL & V5 – 6 (T wave opposite QRS) • delayed intrinsicoid deflection over left ventricle (V6); normal over V1 ST Segment Changes: Identifying MI Mimics Left Bundle Branch Block (LBBB) • hypertensive heart disease • aortic stenosis • degenerative changes of the conduction system • coronary artery disease ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics LBBB with Acute Myocardial Infarction ST Segment Changes: Identifying MI Mimics Left Ventricular Hypertrophy ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Left Ventricular Hypertrophy ST Segment Changes: Identifying MI Mimics • Brugada Syndrome – autosomal dominant inheritance (SCN5A) gene – sodium channel involvement in 25% of the patients – Asian populations (58%) – high incidence of polymorphic ventricular tachycardias ST Segment Changes: Identifying MI Mimics • Brugada Syndrome – found in right precordial leads – prominent J wave – ST – segment elevation in the absence of structural heart disease – three types ST Segment Changes: Identifying MI Mimics • Brugada Syndrome – Type I: ST – segment elevation is triangular and T waves may be inverted in V1 – V3 – Type II: downward displacement of ST – segment (does not reach baseline) – Type III: middle part of ST segment touches baseline ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics Brugada Syndrome ST Segment Changes: Identifying MI Mimics LBBB • Infarction Resemblance – ST segment elevation in the negatively deflected leads, (V1 – V3) – QS complexes in the negatively deflected leads, (V1 – V3) • Recognition – Wide QRS – QS in V1 ST Segment Changes: Identifying MI Mimics Ventricular Rhythms • Infarction Resemblance – ST segment elevation in the negatively deflected leads, (V1 – V3) – QS complexes in the negatively deflected leads, (V1 – V3) • Recognition – Wide QRS following pacer spike – Negative V1 (RV paced) ST Segment Changes: Identifying MI Mimics LVH • Infarction Resemblance – ST segment elevation in the negatively deflected leads, (V1 – V3) • Recognition – Choose deepest S wave from V1 and V2 – Choose tallest R wave from V5 and V6 – Add deflections of tallest R wave and deepest S wave – Suspect LVH if total is > 35 ST Segment Changes: Identifying MI Mimics Pericarditis • Infarction Resemblance – ST segment elements in multiple leads • Recognition – ST segment elevation not in anatomical grouping – PR segment deprewsion – Notching of the J point ST Segment Changes: Identifying MI Mimics Acute Pulmonary Emboli • Infarction Resemblance – RVH with strain pattern – RBBB pattern in V1 – S1Q3 on frontal plane • Recognition – Patient is symptomatic with atypical cardiac pain – Elevates BMP – r/o with spiral CT/angiogram ST Segment Changes: Identifying MI Mimics Ventricular Aneurysm • Infarction Resemblance – High risk for ventricular dysrhythmias (VT with RBBB pattern) – Inferolateral MI – Persistent ST segment elevation – Small q wave in II, III, aVL • Recognition – Structural abnormality on ECHO – CHF & exercise – induced syncope (VT) ST Segment Changes: Identifying MI Mimics Brugada Syndrome • Infarction Resemblance – Ventricular dysrhythmias (polymorphic VT) – ST segment elevation in right precordial leads • Recognition – Autosomal dominant – Asian culture – No structural abnormality noted on ECHO ST Segment Changes: Identifying MI Mimics • Prominent J with ST segment elevations – septal MI – RV cardiomyopathy – pericardial effusion – hypercalcemia ST Segment Changes: Identifying MI Mimics • Prominent J with ST segment elevations – hyperkalemia – acute pulmonary embolism – subarachnoid hemorrhage – tricyclic antidepressant intoxication ST Segment Changes: Identifying MI Mimics ST Segment Changes: Identifying MI Mimics • In Conclusion – is the patient having a MI? – a variety of conditions can mimic infarction ST segment changes