GAIT - Baylor College of Medicine
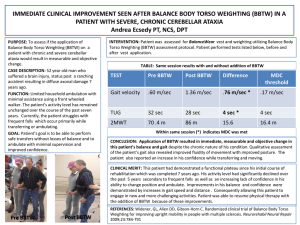
advertisement

GAIT- BALANCE DISORDER AND ASSISTIVE DEVICES Kashif A. Siddiqui, MD Geriatrics Medicine Baylor College of Medicine BROOKE SALZMAN, MD, Thomas Jefferson University, Philadelphia, Pennsylvania Am Fam Physician. 2010;82(1):61-68 SARA M. BRADLEY, MD, and CAMERON R. HERNANDEZ, MD, Mount Sinai School of Medicine, New York Am Fam Physician. 2011;84(4):405-411 Objectives • • • • • Normal Gait Abnormal Gait Pattern Basic Understanding of Gait Disorder Evaluation & Interventions Basic Understanding of Assistive Devices Definitions Gait Series of rhythmical , alternating movements of trunk & limbs resulting in forward progression of the COG Gait Cycle Begins when reference foot contacts the ground, Ends with subsequent floor contact of the same foot Step length Right step Length = Left step Length (Normal Gait) Stride Length Double the step length Walking base Side-to-side distance between the line of the two feet Comfortable Walking Speed (CWS) Least energy consumption per unit distance Average = 1.4 meter/sec Path of Center of Gravity • Center of Gravity (CG): o midway between the hips o Few cm in front of S2 • Least energy consumption if CG travels in straight line Path of C.G Vertical displacement: • Rhythmic up & down movement • Highest point: midstance • Lowest point: double support • Average displacement: 5cm • Path: extremely smooth sinusoidal curve Path of Center of Gravity Overall displacement: • Sum of vertical & horizontal displacement • Figure ‘8’ movement of CG as seen from AP view Horizontal plane Vertical plane Gait & Aging • No clearly accepted standards to define normal Gait in Older Adults • Changes at Aging o o o o o 10-20 % reduction in Gait Velocity & Stride Length. Increase Stance Width. Increase time spent in the Double Support Phase. Bent Posture. Slow & Wide Based Gait. • Up to 20% maintain normal Gait pattern into very old age, reinforcing that Aging not inevitably accompanied by disordered Gait. Gait & Balance Disorder • Most common causes of falls in Older Adults • Evaluation of Gait & Balance disorder parallels the evaluation of FALLS • It can lead to o o o o Injury & Disability loss of independence & reduces level of functioning limited quality of life Increase morbidity & mortality • 60% 80-84 yrs, 25% 70-74 yrs, & 30% 65 yrs have difficulty : o walking 3 blocks or o climbing 1 flight of stairs • 20 % require Assistive Devices to ambulate American Geriatrics Society/British Geriatrics Society clinical practice guideline: prevention of falls in older persons http://www.medcats.com/FALLS/frameset.htm. Accessed June 3, 2010 Falls related statistics • 5.8 million US Adults reported Falls o NH Residents (1.6 falls/bed/year) o 10–25% NH falls result in ER visits/hospital care • Mostly minor injuries o 10-15% resulting in fracture o 5% in serious soft tissue injury or head trauma • Leading cause (75%) of injury deaths for >65 yr o 60% fatal falls happen at home o 30% in public places o 10% in institutions Gait & Balance Disorder • Multifactorial Etiology • Comprehensive Assessment required to determine o Contributing factors o Targeted interventions • Most Gait changes in Older Adults related to underlying Medical conditions Sudarsky L. Gait disorders: prevalence, morbidity, and etiology. Adv Neurol. 2001;87:111-117. Causes of Gait & Balance Disorder • Affective Disorder & Psychiatric Conditions o o o o Depression Fear of falling Sleep Disorders Substance Abuse • Cardiovascular Disease o o o o o o CHF CAD Orthostatic Hypotension PAD Thromboembolic Arrhythmias • Neurological o o o o o o o o o Delirium Dementia Multiple Sclerosis Myelopathy NPH Parkinson Disease Stroke Vestibular Disorders Cerebellar Dysfunction • Sensory Abnormalities o Hearing Impairment o Peripheral Neuropathy o Visual Impairment Alexander NB. Gait disorders in older adults. J Am Geriatr Soc. 1996; 44(4):434-451 Causes • Infectious & Metabolic o o o o o o o o o Diabetes Mellitus Hepatic Encaph. HIV Hypothyroidism Hyperthyroidism Obesity Tertiary Syphilis Uremia Vitamin B12 Deficiency • Others o Recent Surgery o Recent Hospitalization (cont.) • Musculoskeletal Disease o o o o o o Osteoarthritis Osteoporosis Gout Spinal Stenosis Cervical Spondylosis Podiatric Conditions • Medications o o o o o Antiarrythmics, Digoxin Diuretics Narcotics Antidepressants, Psychotropics Anticonvulsants Alexander NB. Gait disorders in older adults. J Am Geriatr Soc. 1996; 44(4):434-451 Evaluation • History o o o o o o Acute and Chronic Medical problems Complete ROS Falls History (Previous Falls, Injury resulted, circumstances, & associated Sx. Nature of Difficulty with Walking (e.g. Pain, imbalance) Surgical History Usual Activity, mobility status, and level of function • Medication review o New medication or dosing review o Number and type of medications Hough JC, McHenry MP, Kammer LM. Gait disorders in the elderly. Am Fam Physician. 1987;35(6):191-196 Sudarsky L. Clinical approach to gait disorders of aging: an overview. In: Masdeu JC, Sudarsky L, Wolfson L, eds. Gait Disorders of Aging: Falls and Therapeutic Strategies. Philadelphia, Pa.: Lippincott-Raven; 1997:147-157 Evaluation • Presence of environmental Hazards o o o o o o o Clutter Electrical Cords Lack of grab bars near bathtub & toilets Low chairs Poor Lighting Slippery Surfaces Throw rugs Evaluation • Physical Examination o Vitals • (Wt. Ht. Orthostatic BP & Pulse) o Affective/cognitive • (Delirium, Dementia, Depression, Fear of Falling) o Cardiovascular • (Murmur, Arrhythmias, Carotid Bruit, Pedal Pulses) o Musculoskeletal • (Joint swelling, deformity, Limited ROM or instability) o Neurological • (M/S strength, tone, reflexes, coordination, sensation tremors, cerebellar, vestibular, sensory & proprioception) Evaluation Gait & Balance Performance Testing 1. Direct observation of gait & Balance • Watching patient enter and sitting in examination room o Stance o posture o Velocity o step length o Symmetry o Cadence o fluidity of movement o instability & need of assistance Evaluation Gait & Balance Performance Testing 2. Functional Reach Test • Reliable • Valid • Quick diagnostic tool • Inability to reach at least 7 inches predictive of fall Duncan PW, Studenski S, Chandler J, Prescott B. Functional reach: predictive validity in a sample of elderly male veterans. J Gerontol. 1992; 47(3):M93-M98 Evaluation Gait balance & performance testing 3. Timed Up & Go Test • Reliable Diagnostic tool (Sensitivity 80% & Specificity 80%) • Quick to administer • (Pt arise from a chair, without using arms, walk 3 meter, turn, return to the chair and sit down. They allowed to use their usual walking aids.) • Score < 10 sec normal • Score > 14 Sec Abnormal • Score > 20 Sec Severe gait impairment Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67(6):387-389 Evaluation Gait & Balance Performance Testing 4. Single leg stance test • Best balance measure for any individual • If one can stay on one leg for >10 sec, usually no significant balance problems Evaluation • Other Diagnostic Testing o Role of Lab testing in diagnostic evaluation has not been well studied o Tests useful when H&P raises suspicious for abnormality o CBC o Metabolic Panel o Thyroid Function o RPR o Vitamin B12 Level o CT head o Hearing Test o Visual Screening Gait Patterns • Antalgic o Description: Limited ROM, limping, slow, short steps, unable to bear full weight o Signs: Pain worse with movement & weight bearing o Causes: DJD, Trauma • Waddling o Description: Lumbar lordosis, swaying, wide based o Signs: Hip dislocation, proximal m/s weakness, uses arm to get up from chair o Causes: Muscular dystrophy & Myopathy • Parkinsonian o Description: Short stepped, shuffling, hip, knee & spine flexed o Signs: Bradykinesia, muscular rigidity, reduce arm swing o Causes: Parkinson disease • Choreic o Description: Dance-like, irregular, slow, wide based o Sign: Choreoathetoic movement of UE o Causes: Huntington Disease, Levodopa induced dyskinesia Gait Pattern • Cerebellar Ataxia o Description: Staggering, wide based o Signs: Dysarthria, Dysmetria, dysdiadokinesia, Intentional Tremors, Nystagmus, Romberg's o Causes: Cerebellar Degeneration, Stroke, MS, Thiamine, Vitamin B12 Def. Alcohol • Sensory Ataxia o Description: Unsteady, worse without visual input o Signs: Impaired position & vibration, Romberg's o Causes: Dorsal Column, Neuropathy • Vestibular Ataxia o Description: Unsteady, falling on one side, Postural instability o Signs: Nausea, Normal sensation, Nystagmus o Causes: Menieres, Acute Labrynthitis. • Cautious o Description: Slow, wide based, careful (Walking on Ice) o Signs: Associated with Anxiety, fear of falling, Open spaces o Causes: Deconditioning, Post fall syndrome, visual impairment Gait Pattern • Frontal gait disorder o Description: Freezing, start & turn hesitation o Signs: Dementia, Incontinence o Causes: NPH, Multi-infarct state, Frontal lobe degeneration • Senile gait disorder o Description: Slow, broad based, shuffling & cautious walking pattern o Signs: when underlying disease can not be identified o Causes: May present early manifestation of subclinical ds. • Psychogenic o Description: Bizarre, Non physiologic gait o Signs: Absence of neurological signs o Causes: Factitious, Somatoform disorder & Malingering Intervention • Interventions may impact important Functional outcomes, including Reduction in o Falls o Fear of falling o Overall limitation in mobility Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2009;(2):CD000340. Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821-827. Intervention • Gait Disorder secondary to Medical Conditions o (Arthritis, Vitamin B12, Thyroid Problems, Arrhythmias, Depression etc.) respond well to Medical Therapies. • Adjustment in Medication improves gait disorder • Limited data available, Surgery may improve Gait o o o o Cervical spondylotic myelopathy Lumbar spinal stenosis Normal pressure hydrocephalus Arthritis of hip or knee • Improving Sensory Input o Visual Correction o Hearing Aids Engsberg JR, Lauryssen C, Ross SA, Hollman JH, Walker D, Wippold FJ II. Spasticity, strength, and gait changes after surgery for cervical spondylotic myelopathy: a case report. Spine (Phila Pa 1976). 2003;28(7):E136-E139. Krauss JK, Faist M, Schubert M, et al. Evaluation of gait in NPH before and after shunting. In: Ruzicka E, Hallet M, Jankovic J, eds. Gait Disorders. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2001. Intervention • Other options includes o EXERCISE INTERVENTION & PHYSICAL THERAPY • Target strengths • Balance training • Functional exercises • Flexibility o Evidence supports HOME ENVIRONMENT ASSESSMENT prevent falls & related injuries • Above Interventions augment Gait, Function & Reduces number of falls Schenkman M, Riegger-Krugh C. Physical intervention for elderly patients with gait disorders. In: Masdeu JC, Sudarsky L, Wolfson L, eds. Gait Disorders of Aging: Falls and Therapeutic Strategies. Philadelphia, Pa.: Lippincott-Raven; 1997:327-353. Interventions • Modest improvement in Gait & Balance achievable by ASSISTIVE DEVICES. • Unfortunately, most cases its unlikely that Gait Disorder are reversible Assistive Devices • 6.1 million use assistive devices, 2/3 >65 years of age • ASSISTIVE DEVICES IMPROVE: o o o o Balance Reduce pain Compensate for weakness or injury Increase Mobility & Confidence • ASSISTIVE DEVICE SELECTION DEPENDS: o Amount of support assistive device offers o Coordination required o Strength, ROM, Balance, Stability, General Condition, & WB restrictions Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil. 2005; 86(1): 134-145. Faruqui SR, Jaeblon T. Ambulatory assistive devices in orthopaedics: uses and modifications. J Am Acad Orthop Surg. 2010; 18(1): 41-50. Assistive Device • Patients get Assistive Device without recommendations from Medical Professional • Evaluation should be done routinely for proper Fit & Use o Cane preferred for balance with one UE o Crutches or a walker appropriate for Both • CORRECT HEIGHT & FIT o Correct height of cane/walker • At the level of the patient’s wrist crease, as measured with the patient standing upright with arms relaxed at his or her sides, the patient’s elbow naturally flexed at 15 – 30 degree angle Assistive Devices • INSTRUCTIONS FOR PROPER USE: o Cane: • Should be held contralateral to weak/painful LE & advanced simultaneously with Contralateral Leg. • Need upright posture without forward or lateral leaning. • Take time when turning & should not lift the device off the ground. o Walker: • Both feet should stay between the posterior legs or wheels. • Need upright posture without forward or lateral leaning. • Take time when turning and should not lift the device off the ground. Kumar R, Roe MC, Scremin OU. Methods for estimating the proper length of a cane. Arch Phys Med Rehabil. 1995; 76(12): 11731175 Assistive Devices o INSTRUCTIONS FOR PROPER USE • Navigating Stairs with Cane/Walker: o Patients with unilateral LE impairment advance the Unimpaired Extremity first when going up stairs AND advance the Impaired Extremity first when going down stairs. o • Simply remember this phrase, “Up with the good and down with the bad.” A video about how to use a cane is available online at http://www.youtube.com/watch?v=fRn8ZZJMzno CANES STANDARD CANE • Indications: • • Mild ataxia (sensory, vestibular, or visual) Mild arthritis • Advantages: • • • Inexpensive Adjustable Improves balance • Disadvantages: • • Umbrella handle cause carpal tunnel syndrome Not for weight bearing CANES OFFSET CANE • Indication: o Moderate arthritis • Advantages: o Inexpensive o Intermittent weight bearing o Shotgun handle put less pressure on palm • Disadvantages: o Commonly used incorrectly Liu HH, Eaves J, Wang W, Womack J, Bullock P. Assessment of canes used by older adults in senior living communities. Arch Gerontol Geriatr. 2011; 52(3): 299-303 CANES QUADRIPOD • Indications: o Hemiparesis • Advantages: o Increased base of support o bear large weight o Stands freely on its own • Disadvantages: o Slightly heavier o Awkward to use correctly with all four points on ground simultaneously Laufer Y. Effects of one-point and four-point canes on balance and weight distribution in patients with hemiparesis. Clin Rehabil. 2002; 16(2): 141-148 CRUTCHES AXILLARY CRUTCHES • Indication: o Lower extremity fracture • Advantages: o Inexpensive o Completely redistribute weight off of lower extremities o Permits 80-100 % weightbearing support • Disadvantages: o Difficult to learn to use o Requires energy & strength o Risk of nerve or artery compression CRUTCHES FOREARM CRUTCHES: • Indication: o Paraparesis • Advantages: o Frees hands without having to drop crutch o Less cumbersome to use, particularly on stairs o No Axillary compression • Disadvantages: o Permits only occasional weight bearing WALKERS STANDARD WALKER • Indications: o Severe myopathy o severe neuropathy o Cerebellar ataxia • Advantages: o Most stable walker o Folds easily • Disadvantages: o Slower o Needs to be lifted up with each step o Less natural gait WALKERS FRONT-WHEELED WALKER • Indications: o o o o Severe myopathy Severe neuropathy Paraparesis Parkinsonism • Advantages: o Maintains normal gait pattern o No need to be lifted up with each step • Disadvantages: o Large turning arc o Less stable Cubo E, Moore CG, Leurgans S, Goetz CG. Wheeled and standard walkers in Parkinson’s disease patients with gait freezing. Parkinsonism Relat Disord. 2003; 10(1): 9-14 WALKERS ROLLATOR • Indications: o Moderate arthritis o Claudication o Lung disease, CHF • Advantages: o o o o Easy to propel Highly movable Small turning arc Has seat & basket • Disadvantages: o Not for weight bearing o Less stable o Does not fold easily Selection of AD Assistive Devices List providing stability & support from most to the least : Parallel bars Walker Axillary crutches Forearm crutches Two canes One cane Assistive Devices List requiring Coordination from least to the most: Parallel bars Walker One cane Two canes Axillary crutches Forearm crutches Conclusion • Comprehensive evaluation with targeted interventions reduce falls by 30-40% • Gait Disorder evaluation the most effective strategy for falls prevention • Limited evidence supporting the effectiveness of interventions for gait & balance disorders Harris MH, Holden MK, Cahalin LP, Fitzpatrick D, Lowe S, Canavan PK.Gait in older adults: a review of the literature with an emphasis toward achieving favorable clinical outcomes, part II. Clin Geriatrics. 2008; 16(8):37-45. “Don’t walk behind me, I may not lead. Don’t walk ahead of me, I may not follow. Walk next to me & be my friend.” Albert Camus Thank you !!