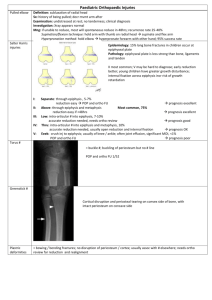
X-ray?
advertisement

Pediatric Orthopedics in the ED Common presentations, common fractures, and common sense treatments. James Thorburn Overview Housekeeping - terms and unique physiology of children General Approach Upper body (limbs) injuries - FOOSH Lower body - Approach to limping child What’s the difference? Periosteum is thicker, stronger, and more biologically active More plastic deformities GROWTH PLATES !! Ligaments stronger than bones Ortho talk Fracture description Buckle Fracture (#) Greenstick # Salter Harris Initial Approach ABC’s - just like everything else Quick assessment for: Neurovascular compromise (NVI) Open # Bleeding - femur and pelvis (C’s) History Mechanism of injury - important time exact location of pain other associated symptoms “SAMPLE” Pain Control! May be nervous about “medicating” kids. DON’T BE! Pain in kids can be difficult to interpret Pain scales Mechanism of injury Clinical exam Pain meds Ibuprofen (advil): 10 mg/kg per dose Acetaminophen (tylenol): 15 mg/kg per dose Narcotics: Fentanyl - IV, or intranasal (12mcg/kg) Morphine - 0.1mg/kg SQ, 0.1-0.5/kg PO SPLINT! Don’t be me back slab! FOOSH Examine clavicle to wrist! Clavicle # Elbow # Forearm # Quick and Dirty NV exam Colour, cap refill, pulses, swelling. Nerves (3) motor and sensory Radial - Thumbs up, 1st dorsal web space Median - Fist, pinch, palmar distal 2/3 digits Ulnar - Peace, distal pinky (palmar) Case 13 year old, fall off scooter SAMPLE hx Quick physical Fentanyl 1.5mcg/kg x 40kg = 60 mcg intranasal Place backslab X-rays. Clavicle # Majority in the middle 1/3 Sling for support (if old enough) Elbow # No one likes elbows ROM important NV exam quite important supracondylar # most common Possible #s Supracondylar Medial/lateral condylar Radial head # (older kids) Olecranon # X-ray approach 5 things to look at, and won’t miss Fat pads Anterior humeral line Hourglass sign Proximal radial line Ossification centres Fat Pads Capitellum is key Hourglass Ossification - CRITOE Supracondylar # management Pain management Non-displaced - back slab and “U” slab and follow up with ortho displaced - consult ortho from department compartment syndrome! Not Sure? No prob! ++ pain Posterior fat pad/ anterior sail sign Back slab and follow up for R/A!! Pulled Elbow Commonly in 9 month - 3 years old (may be older) Subluxation of radial head Mech: axial tension on pronated, extended elbow Minimal swelling, not using arm, holding in pronation Management X-ray? not usually necessary Reduction Hyperpronation Supination and flexion Can’t reduce? Consider x-ray try both techniques immobilize? sling? Arrange follow up Monteggia Galeazzi # Management of buckle and greenstick # Casting vs splinting Dr. Boutis Either for 3 weeks Approach to the limping child Differential is huge!! History is important Don’t ignore caregiver Estimate of 25% no diagnosis Differential - categories Traumatic vs non-traumatic Traumatic Cause may be obvious - #!!! Beware occult # - sprains/strains not as common in kids Buckle # Greenstick # Toddlers # Toddlers # May have a history of fall/trauma, but may not 9 months - 3 years Range of sx - subtle to obvious high index of suspicion needed. Management If obvious - classic teaching long leg splint with ortho f/u discuss with family pros/cons of immobilization if not obvious Usually splinted 5-6 weeks Don’t be afraid of follow up!! No trauma? Think articular vs systemic important questions: Fever? Rash? Preceding illness? Constitutional symptoms? GI sx? Ddx Articular Transient synovitis Septic Arthritis Legg-Calve-Perthes SCFE JRA Reactive arthritis Ddx Extraarticular Malignancy Testicular torsion Sickle cell crisis Rheum / vasculitis Transient synovitis vs Septic DO NOT want to miss septic arthritis can be difficult to tell the difference combination of hx, pe, and investigations can help Transient Synovitis Self limited inflammation of synovial lining (resolve 3-10 days) classically viral prodrome, but not necessary Septic Arthritis Danger to life and limb!! History clues Just how sick is the child? History Fever - how long? how high? toxic? Persistence of non-weight baring? Viral prodrome? Physical Consider early NSAID - may help exam Vitals and Appearance gentle log roll - may be tolerated in T.S. but not S.A. Importance of serial examination Labs Kocher Criteria Non-weight baring affected side ESR >40 Fever WBC >12 Kocher Criteria Good guide to “rule in” in high pretest probability Kocher et all, 2004 Sawyer and Kapoor, 2009 Negative predictive value if no fever and CRP<2 Ultrasound Can look for effusion Can be present in both Management If concern of septic arthritis, prompt Ortho consult. Await joint aspiration to start antibiotics If ortho not promptly available, take blood cultures and start antibiotics. Conclusion Manage Pain! Occult #s!! Elbows X-ray findings Limp Traumatic vs Atraumatic Intraarticular vs Extraarticular