24b96b07-29ca-4625-9682
advertisement
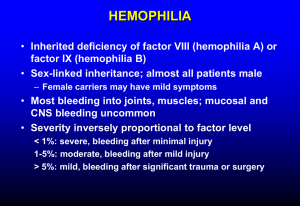
BLEEDING DISORDERS Dr.Nazzal Bsoul Hematologist Al Bashir Hospital HEMOSTASIS-1 In health hemostasis ensures that the blood remains fluid and contained in the vasc.system. If a vessel wall is damaged,a number of mechanisms are activated promptly to limit bleeding,involving: 1-Endothelial cells. 2-Platelets. 3-Plasma coag.factors. 4-Fibrinolytic system. HEMOSTASIS-2 These activities are finely balanced between keeping the blood fluid and preventing intravasc.thrombosis. 1-Pimary hemostasis: vasoconstriction and platelet adhesion and aggregation leading to the formation of the platelet plug. 2-Secondary hemostasis: involves activation of coag.system leading to the generation of fibrin strands and reinforcement of the platelet plug. 3-Fibrinolysis: activation of fibrin-bound plasminogen resulting in clot lysis. ROLE OF ENDOTHELIAL CELLS IN HEMOSTASIS Blood vessels are lined with endothelial cells,which synthesize and secrete various agents,that regulate hemostasis. 1-Procoagulant(prothrombotic) agents:tissue factor,von Willebrand factor,F V ,F VIII. 2-Anticoagulant (antithrombotic) agents: prostacyclin,nitric oxide,endothelin-1. ROLE OF PLATELETS IN HEMOSTASIS 1. Each megacaryocyte produces 10002. 3. 4. 5. 2000 platelets,which remain in the circulation for about 10 days. Releasing of hemostatic proteins. Platelet adhesion. Platelet aggregation. COAGULATION FACTORS Coag.factors:are plasma proteins synthesized in the liver which,when activated lead to the deposition of fibrin. 1-Initiation phase:leads to the formation of the complex TF-VIIa. 2-Amplification phase:leads to the formation of a small amount of thrombin from prothrombin. 3-Propagation phase:leads to the formation of much larger amounts of fibrin. INHIBITORS OF COAGULATION Are proteins that inhibit activated procaog.enzymes and prevent excessive intravasc.coagulation Raised levels are not associated with bleeding. Reduced levels may predispose to thrombosis. Antithrombin. Protein C,Protein S. Tissue Factor Pathway Inhibitor (TFPI). FIBRINOLYSIS Small amouns of fibrin are constantly deposited within the vascular system and are removed by the fibrinolytic system Plasminogen Plasmin Fibrin FDPs ASSESSMENT OF BLEEDING SYMPTOMS 1-Careful and full clinical history and examination. 2-Appropriate lab.investigations. 3-Other investigations. HISTORY 1-Site of bleeding. 2-Duration of bleeding. 3-Precipitating cause. 4-Surgery. 5-Family history. 6-Systemic illnesses. 7-Drugs. Clinical Features of Bleeding Disorders Platelet disorders Coagulation factor disorders Site of bleeding Skin Mucous membranes (epistaxis, gum, vaginal, GI tract) Deep in soft tissues (joints, muscles) Petechiae Yes No Ecchymoses (“bruises”) Small, superficial Large, deep Hemarthrosis / muscle bleeding Extremely rare Common Bleeding after cuts & scratches Yes No Bleeding after surgery or trauma Immediate, usually mild Delayed (1-2 days), often severe Coagulation factor disorders Inherited bleeding disorders Acquired bleeding disorders 1. Hemophilia A and B 2. vonWillebrand disease 3. Other factor deficiencies 1. Liver disease 2. Vitamin K deficiency/warfarin overdose 3. DIC HEMOPHILIAS Definition Hemophilias are a group of related bleeding disorders that most commonly are inherited. When the term ”hemophilia” is used, it most often refers to the following two disorders: 1- Factor VIII deficiency: hemophilia A 2- Factor IX deficiency: hemophilia B (Christmas disease) Factor XI deficiency: hemophilia C. History Hemophilia has featured prominently in European royalty and thus sometimes known as “the royal disease”. Queen Victoria passed the mutation for hemophilia B to her son Leopold, and through some of her daughters, to various royals across the continent, including the royal families of Spain, Germany, and Russia. Clinical Manifestation They exhibit a range of clinical severity that correlates well with factor levels. Severe disease: factor activity less than 1% Moderate disease: factor activity 1-5% Mild disease: factor activity more than 5% Incidence and Inheritance-1 The combined incidence of hemophilia A and B is 1 in 5000 live male births. Approximately 80% have hemophilia A,2/3 of whom have severe disease. Hemophilia A is the second most common inherited bleeding disorder. Severe cases among patients with hemophilia B are less common (about ½) Hemophilia A and B are X-linked recessive diseases. Write Presentation Title in Footer Incidence and inheritance-2 • • • • Factor VIII and IX are localized on X Chromosome Haemophilia A and B are caused by a defect on the X chromosome Affect almost exclusively men Affect equally all races and ethnic groups Male Female Carrier female Male with Haemophilia Slide Slide 18 18 X-Linked Recessive Inheritance Father With Haemophilia X Y X• XX• X•Y X XX XY 50% of daughters will be carriers • 50% of sons will have hemophilia • Healthy Mother Carrier Mother Healthy Father X• Y X XX• XY X XX• XY All daughters will be carriers All sons will be healthy • • Initial presentation-1 The majority of patients are known to have hemophilia because of the family history. The majority of newborns with severe hemophilia traverse delivery and the first few months of life without detection. Early bleeding occurs commonly in association with circumcision. Initial presentation-2 The majority of newborns with severe hemophilia become symptomatic during the first 2 years of life. Mean age at diagnosis of severe hemophilia 9 months,moderate disease 22 months. Moderate and mild hemophilia may,in the absence of informative family history,go undetected for signficant periods of time (age 14-62 years). Sites of bleeding As children begin to ambulate,bleeding episodes occur more often and begin to involve joints and muscles,as well as other systems: 1-Hemarthrosis: is a painful,debilitating manifestation of hemophilia. 2-Skeletal muscle:hematoma formation most affects quadriceps,iliopsoas,and forearm. 3-CNS:intracranial hemorrhage. Hemarthrosis (acute) Diagnosis Family history: mainly on the maternal side of the family. Screening tests. Specific factor assay, genetic testing. Family history The patients mother is a known carrier. Negative family history in about 1/3 of patients. Lack of a family history is of little value in excluding the possibility of hemophilia. 1-spontaneous mutation which occurs 25-33% of cases. 2-Neonatal deaths or a passage of the trait through a succession of female carriers Screening tests Initial tests to be done in patients with a bleeding diathesis of unknown etiology: 1-Platelet count 2-Prothrombin time (PT). 3-Activated partial thromboplastin time (aPTT). A normal platelet count,normal PT,and a prolonged aPTT is characteristic of hemophilias, and heparin therapy. Specific assays Factors that can produce an isolated prolonged aPTT are F VIII,F IX,and FXI Genetic analysis of F VIII and F IX. Prof.Abbadi did genetic studies to the all Jordanian patients with hemophilia and identified new novel mutations among Jordanians with hemophilia A and B. Hemophilia in females Symptomatic hemophilia has been welldocumented in females. Three possible explanations for this : 1-X-chromosome inactivation in early stage of embryogenesis. 2-Mating between an affected male and a carrier female produces homozygous disease in ½ of female offspring. 3-Abnormal karyotype (Turner syndrome) Late complications 1-Joint destruction due to hemarthroses, leading to a number of orthopedic abnormalities (hemophilic osteoarthropathy). 2-Transmission of blood-borne infections. 3-Development of inhibitor antibodies. Hemophilic arthropathy Multiple factors may contribute to synovitis and joint destruction in patints with hemarthroses. 1- Tissue deposition of iron 2- Dense fibrosis of the joint with contractures,pain,and limitation of motion. Primary prophylactic treatment with factor concentrates can markedly reduce the risk of subsequent arthropathy. Synovectomy: pharmacological synovectomy. radioactive synovectomy. Infection Patients treated with older factor VIII and IX concentrates were at high risk for infection with hepatitis A,B,C,and D and with HIV. The risk of infection has been reduced markedly by improvement in donor screening and virucidal techneques and the development of recombinant products. Inhibitors Antibodies are primarily IgG. Occur in 25% of severe hemophilia A,and 3-5% of those with severe hemophilia B. Much less common in patients with mild or moderate disease. Increased risk of bleeding. Maturational delays. Management-1 Complex, and should include: 1-Preventive and comprehensive care. (routine immunizations,circumcision, dental care,counselling and education,exercise and athletic participation) 2-Replacement therapy (treatment and prophylaxis) 3-Other therapies: gene therapy. Therapies other than replacement therapy Ice. Immobilization. Steroids. Physiotherapy. Analgesia: aspirin and NSAIDs are contraindicated, paracetamol or codeine can be used. Desmopressin. Antifibrinolytic therapy: tranexamic acid,epsilon 34 Treatment of hemophilia A Intermediate purity plasma products – Virucidally treated – May contain von Willebrand factor High purity (monoclonal) plasma products – Virucidally treated – No functional von Willebrand factor Recombinant factor VIII – Virus free/No apparent risk -No functional von Willebrand factor Dosing guidelines for hemophilia A Mild bleeding – Target: 30% dosing q8-12h; 1-2 days (15U/kg) – Hemarthrosis, oropharyngeal or dental, epistaxis, hematuria Major bleeding – Target: 80-100% q8-12h; 7-14 days (50U/kg) – – – – CNS trauma, hemorrhage, lumbar puncture Surgery Retroperitoneal hemorrhage GI bleeding Adjunctive therapy Tranexemic acid or DDAVP (for mild disease only) Treatment of hemophilia B Agent – High purity factor IX – Recombinant human factor IX Dose – Initial dose: 100U/kg – Subsequent: 50U/kg every 24 hours Treatment of patients with inhibitors-1 Components of therapy: 1-Treatment of active bleeding. 2-Inhibitor ablation via immune tolerance induction (inhibitor eradication). Treatment of patients with inhibitors-2 Inhibitor bypassing products: 1-Prothrombin complex concentrates, FIEBA: are associated with a lot of complications. 2-Recombinant activated factor VII ( r FVIIa): no anamnestic antibody response.Not associated with increased risk of DIC due to it’s localized effect. THANK YOU