Center for Cancer Risk Assessment
advertisement

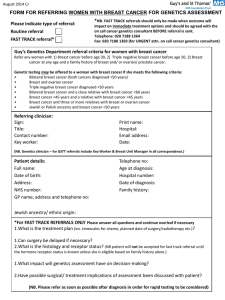
Evidence-based detection and management of hereditary breast cancer syndromes Kristen Mahoney Shannon, MS, CGC Program Manager/Sr. Genetic Counselor Date MGH Center for Cancer Risk Assessment April 13, 2012 Lecture Overview Detection • Identifying Risk • Personal / Family history • Genetic Testing • Syndromes Hereditary Breast/Ovary Cancer Syndrome (HBOC) Li-Fraumeni Syndrome (LFS) Cowden Syndrome Hereditary Diffuse Gastric Cancer (HDGC) Peutz-Jeghers Syndrome (PJS) Management • Cancer Screening • Cancer Risk Reducing Surgeries • Psychosocial Management Relative Risk of Developing Cancer Association between population frequency and relative risk for breast cancer Frequency in the Population (Percent) Foulkes W. N Engl J Med 2008;359:2143-2153 Detection of At-Risk Individuals Comprehensive Risk Assessment A Classic Hereditary Breast/Ovarian Family CancerHistory Kindred Breast, 49 73 Breast, 38 55 Breast, 29 Ovary, 42 d 45 Breast, 32 Personal Medical History Non-familial Risk Factors •Early menarche/late menopause • Nulliparity or late pregnancy • OCP use/hormonal exposures • Breast irradiation (during puberty) • Breast density • High BMI/Obesity • Atypical hyperplasia/ Lobular Carcinoma in Situ 80 Breast, 49 57 62 29 Physical Exam Genetic Testing Single Gene Testing Gene Panel Testing Hereditary Breast/Ovarian Cancer (HBOC) A Classic Hereditary Breast/Ovarian BRCA1 and BRCA2 Cancer Kindred Breast, 49 73 Breast, 38 55 Breast, 29 Ovary, 42 d 45 Breast, 32 80 Breast, 49 57 29 62 BRCA1 and BRCA2 phenotype Breast Cancers • BRCA1 – 80% are triple negative • BRCA2 – garden variety Ovarian Cancers • Endometriod, serous (BRCA1 and BRCA2) • Serous papillary (BRCA1) • NOT borderline tumors Identifying BRCA carriers HBOC Cancer Risks Breast Cancer Risk BRCA1: 50-80% BRCA2: 40-70% Ovarian Cancer Risk BRCA1: 40-60% BRCA2: 15-20% Other Cancer Risk Male Breast: <6-7% Pancreatic: 1.3-7% Prostate: <30-40% HBOC Cancer Risks Can Be Modified • • • • Lifestyle factors Location in the gene “Modifier” gene allelotypes Hormonal Interventions Breast Cancer Incidence (Penetrance) Non-carrier Chance of Remaining Cancer Free (Opposite Breast) In Different BRCA1 and BRCA2 Carrier Populations Metcalfe K et al JCO 22:2328, 2004 Li-Fraumeni Syndrome (TP53 gene) Component Tumors: •Sarcoma •Breast Cancer •Brain tumors •Leukemia (childhood) •Adrenal cortical carcinoma Identifying LFS Table 1: Clinical Criteria for Classic Li-Fraumeni Syndrome Li-Fraumeni Like Syndrome, and Chompret Criteria Classic Li-Fraumeni syndrome (LFS) criteria Proband diagnosed with a sarcoma before 45 years of age; and A first degree relative with cancer diagnosed before 45 years of age; and A first of second degree relative on the same side of the family with cancer diagnosed before 45 years of age OR a sarcoma at any age Li-Fraumeni Syndrome-Like (LFL) criteria Proband with any childhood cancer or sarcoma, brain tumor, or adrenocortical carcinoma diagnosed before 45 years of age; and First or second degree relative with a component LFS cancer (sarcoma, breast cancer, brain tumor, leukemia, or adrenocortical carcinoma) diagnosed at any age and; One first or second degree relative on the same side of the family with any cancer diagnosed under age 60 Chompret criteria Proband diagnosed with a narrow spectrum cancer (sarcoma, brain tumor, breast cancer, or adrenocortical carcinoma) before age 36 years, and at least one first or second degree relative affected by a narrow spectrum tumor (other than breast cancer if the proband was affected by breast cancer) before 46 years or a relative with multiple primary tumors at any age A proband with multiple primary tumors, two of which belong to the narrow spectrum and the first of which occurred before 36 years, regardless of family history A proband with adrenocortical carcinoma, regardless of age at diagnosis or family history *First degree relative is defined as parent, sibling, or child; *Second degree relative is defined as grandparent, aunt, uncle, niece, nephew, or grandchild LFS Cancer Risks ~75% of tumors are classic component tumors Risk of cancer 100 80 60 40 20 0 15- 40- 20y 45y 50y 80y Nichols, K.E., et al., Cancer Epidemiol Biomarkers Prev, 2001. 10(2): p. 83-7 Hwang, S.J., et al., Am J Hum Genet, 2003. 72(4): p. 975-83. . Chompret, A., et al., Br J Cancer, 2000. 82(12): p. 1932-7. Le Bihan, C., et al.,. Genet Epidemiol, 1995. 12(1): p. 13-25. Other tumors: Colorectal cancer Endometrial cancer Esophageal cancer Gonadal germ cell tumor Hematopoietic malignancies (leukemias and lymphomas) Lung cancer Melanoma and non-melanoma skin cancer Neuroblastoma Ovarian cancer Pancreatic cancer Prostate cancer Stomach cancer Thyroid cancer Wilms’ tumor and other kidney cancers 57% risk of 2nd primary 38% risk of 3rd primary Cowden Syndrome (PTEN gene) 91 yr 70 yr 32 yr 67 yr 42 yr 94 yr lung cancer 75 yr 65 yr colon polyps head circumference 62 cm oral mucosal papillomatosis 40 yr 33 yr cancer, unspecified 65 yr 35 yr enlarged thyroid 56 yr 37 yr recurrent goiter since 16 yr DCIS, 35 oral mucosal papillomatosis head circumference 60 cm Courtesy of G. Chan-Smutko, MGH Cowden Syndrome (PTEN gene) Cutaneous features (90-100%) (Oral) mucosal papillomas coalesce into “cobblestone” surface Trichilemmomas (facial) Acral keratoses (palmar/plantar) Papillomatous lesions trichilemmoma Images referenced from: Gene reviews: http://www.ncbi.nlm.nih.gov/books/NBK1488/ Emedicine: http://emedicine.medscape.com/article/1059940-overview Identifying Cowden Syndrome http://www.lerner.ccf.org/gmi/ccscore/ Cowden Syndrome Cancer Risks Tumor Site Risk Pilarski R. JGC.2009;18:13-27 Risk Tan et al. Clin Can Res. 2012;18(2):400-7 Breast 25-50% 85% Thyroid 3-10% 35% Endometrial 5-10% 28% Renal Cell Unknown 34% Melanoma Unknown 6% Colon Unknown 9% Hereditary Diffuse Gastric Cancer CDH1 gene 75 65 24 80 58 BR 56 49 47 45 ?CA 69 33 STO 32 35 THY 29 39 73 BR 66 86 BR 75 65 OV 51 STO 50 70 40 81 BR 77 60 78 57 66 BR 58 BR 66 STO 67 32 2 6 5 3 Courtesy of D. Patel, MGH Identifying HDGC The International Gastric Cancer Linkage Consortium (IGCLC) criteria: • Two gastric cancer (GC) cases in family, one individual under age 50 years with confirmed diffuse gastric cancer (DGC) • Three confirmed DGC cases in first- or second-degree relatives independent of age • Simplex case (i.e., a single occurrence in a family) of DGC occurring before age 40 years • Personal or family history of DGC and lobular breast cancer, one diagnosed before age 50 years Fitzgerald et al, 2010 HDGC Cancer Risks Diffuse Gastric Cancer Risk in CDH1 carriers by Age 90 Lobular Breast Cancer Risk = 39-51% 80 70 60 50 Women 40 Men 30 20 10 0 30years 50 years Lifetime Peutz-Jeghers Syndrome (PJS) STK11 gene Melanotic macules, intestinal polyps, increased cancer risk Identifying PJS Clinical Diagnosis • Two or more histologically confirmed PJ polyps • Any number of PJ polyps detected in one individual who has a family history of PJS in close relative(s) • Characteristic mucocutaneous pigmentation in an individual who has a family history of PJS in close relative(s) • Any number of PJ polyps in an individual who also has characteristic mucocutaneous pigmentation Beggs, et al (2010) PJS Cancer Risks Cancer Risks: Pancreas Liver Lungs Breast Ovaries Uterus Testicles other Low-Moderate Penetrant Genes Description Genes functionally related to BRCA1 and BRCA2 Genes ATM BARD1 CHEK2 MRE11A NBN RAD50 RAD51C (other) Genes in the Fanconi Anemia Pathway BRIP1 PALB2 Genes involved in hereditary colorectal cancer MLH1 MSH2 MSH6 PMS2 MYH 2-4x RR of breast cancer Managing Breast Cancer Risk For BRCA carriers: • Breast self-exam training and education and regular monthly BSE starting at age 18y • Semiannual clinical breast exam starting at age 25y • Annual mammogram and MRI screening starting at age 25 • Discuss option of prophylactic mastectomy on case-by-case basis • Consider chemoprevention options for breast and ovarian cancer • Consider investigational imaging and screening studies High-Risk Patient With MRI detected Breast Cancer: Normal Mammogram Courtesy of Dr. Phoebe Freer, MGH MRI Detects an Apparent Cancer Courtesy of Dr. Phoebe Freer, MGH Risk Reducing Mastectomy • Bilateral prophylactic mastectomy decreases risk breast cancer ~90% • Prophylactic contralateral mastectomy decreases risk second breast cancer ~90% Hartmann L NEJM 2001; Seynaeve C ASCO abs #102962 2002; Rebbeck T JNCI 1999; NEJM 2002; Kauff N NEJM 2002 • • • Uptake ~50% More often in women w/ sister or mother w/ breast ca Less when mom or sister had ovarian cancer Skytte et al, Clin Genet 2010; Metcalfe et al Clin Genet 2008 Managing Ovarian Cancer Risk • Recommend ovary/fallopian tube removal, ideally between 35 and 40 y, or upon completion of child-bearing • For those who have not elected ovary/fallopian tube removal, consider concurrent ultrasound + Ca-125 every 6 mo starting at age 35y or 5-10 y earlier than the earliest age of first diagnosis of ovarian cancer in the family • Consider chemoprevention options for breast and ovarian cancer • Consider investigational imaging and screening studies Risk Reducing Oophorectomy • Decreases risk of breast cancer ~50% • Decreases risk of ovarian cancer ~90% Hartmann L NEJM 2001; Seynaeve C ASCO abs #102962 2002; Rebbeck T JNCI 1999; NEJM 2002; Kauff N NEJM 2002 • Uptake ~90% • More often in women w/ mom or sister with ov cancer • BRCA2 carriers less Skytte et al, Clin Genet 2010; Metcalfe et al Clin Genet 2008 Management – Other cancers Gene BRCA1/2 LFS Cancer Risk Screening Begin at age Frequency Surgery Prostate PSA/DRE As directed annual Not discussed Pancreatic Investigational (EUS/MRI) 10 years earlier than panc dx annual Not discussed Male Breast BSE CBE Consider mammo 35 35 40 Monthly Q 6mo annual Not discussed Brain Investigational (MRI) childhood Annual n/a Sarcoma Investigational (whole body MRI) childhood annual n/a Leukemia Investigational Bloodwork childhood annual n/a Adrenal Investigational MRI childhood annual n/a Colon Consider Colonoscopy 25 2-5y Per clinical findings Others As directed Management – Other cancers (cont.) Gene Cowden HDGC PJS Cancer Risk Screening Begin at age Frequency Surgery Thyroid U/S & bloodwork 18 Consider annual Not discussed Endometrial Education n/a n/a Consider Renal Cell Urinalysis 18 annual Not discussed Colon Consider colonoscopy 35 (50?) 5-10y Per clinical findings Melanoma Consider derm exam 18 Annual n/a Stomach Upper endoscopy w/ random biopsies 20? Q 6mo Recommended Colon Consider colonoscopy 10 years younger than youngest dx or 35y 3-5 Not discussed Colon Colonoscopy 18 Annual Per clinical findings Ovary / Uterus Education n/a n/a Consider Testicular Exam & u/s Childhood Annual Not discussed Small bowel Upper endoscopy plus small bowel examination (MR or CT enterography, wireless capsule endoscopy 8y annual Not discussed Other Management Issues • Education about signs and symptoms of cancer • Education about heritability / encourage family testing • Education about prenatal diagnosis / assisted reproduction • Psychosocial Management Summary • Detection & Management not straightforward • Multidisciplinary effort • Genetic Counselors / Specialists Acknowledgements MGH Center for Cancer Risk Assessment Breast/Ovarian Cancer Genetics Program Leif Ellisen, MD, PhD, Director Gayun Chan Smutko, MS, CGC Devanshi Patel, MS, CGC Michele Jacobs Gabree, MS, CGC Janette Lawrence, MS, CGC Erica Blouch, MS, CGC Meredeth Seidel, MS, CGC