UCVA D - Lingua Lasik
advertisement

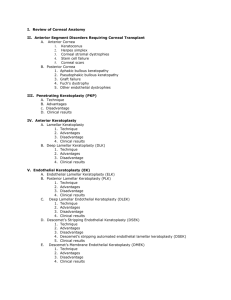
Conductive Keratoplasty for the Correction of Low to Moderate Hyperopia: U.S. Clinical Trial 12-Month Results U.S. Clinical Investigators Marguerite McDonald, MD – Medical Monitor Penny Asbell, MD Stephen Brint, MD William Culbertson, MD Jonathan Davidorf, MD Elizabeth Davis, MD Dan Durrie, MD R. Bruce Grene, MD Peter Hersh, MD David Hardten, MD Vera Kowal, MD Richard Lindstrom, MD Robert Maloney, MD Edward Manche, MD Roger Meyer, MD Thomas Samuleson, MD Timothy Schneider, MD Kaz Soong, MD Alan Sugar, MD Conductive Keratoplasty Features • Treats hyperopia, astigmatism, presbyopia and over/under LASIK corrections • Induces permanent collagen shrinkage • Creates a column of treatment • Utilizes cornea’s conductive properties ViewPoint™ CK System The Keratoplast™ tip (90 µm wide, 450 µm long) with coated stop at the distal end (shown next to a 7-0 suture) Conductive Keratoplasty (CK) Study Objective • US FDA Phase III Study • 400 Patients – Spherical hyperopia 0.75 D to 3.00 D – < 0.75 D of cylinder – No prior refractive surgery – No significant ocular/physical history • 24 Month Follow-Up Demographics Number of Patients Number of Eyes Mean Age Range Mean Preoperative MRSE Median MRSE Mean Preoperative CRSE 233 401 55 +/- 5.4 years (40 to 74) +1.82 +/- 0.60 D +1.75 D +1.86 +/- 0.63 D Simple Procedure • • • • Instill topical anesthesia Insert lid speculum (return path for energy) Mark eye Apply treatment Total time less than 5 minutes Conductive Keratoplasty (CK) Number, Location, and Sequence of Treatment Spots 8 spots 16 spots (0.75 to 0.875 D) (1.00 to 1.625 D) Sequence 5 1 8 3 4 7 24 spots 32 spots (1.75 to 2.25 D) (2.375 to 3.00 D) 2 6 6 mm OZ 7 mm OZ 8 mm OZ Slit Lamp Photo 1 Hour After CK Small leucoma Visible striae Percent Postoperative UCVA Over Time 100 90 80 70 60 50 40 30 20 10 0 90 93 92 86 56 4550 40 6364 73 75 Month 3 N=358 Month 6 N=352 Month 9 N=347 Month 12 N=318 20/20 or > 20/25 or > 20/40 or > Accuracy of Achieved Refraction Percent 100 90 80 70 60 50 40 30 20 10 0 83 56 88 87 89 9799 99 99 Month 3 N=358 Month 6 N=352 Month 9 N=347 Month 12 N=318 61 64 63 +/- 0.5 D +/- 1.0 D +/- 2.0 D MRSE Stability through 12 Months Percent Patients with Consecutive Visits 100 90 80 70 60 50 40 30 20 10 0 87 83 98 99 89 74 <0.50 D <0.75 D <1.00 D 3 to 6 Mo. Mean Change in MRSE Conf. Interval 96 98 93 6 to 9 Mo. 9 to 12 Mo. 0.25 D (0.50) 0.11 D (0.41) 0.11 D (0.35) 0.19, 0.31 0.07, 0.15 0.07, 0.15 Safety Variables 2 lines lost BSCVA 12 Months N=383 2% > 2 lines lost BSCVA 0.0% BSCVA Worse than 20/40 0.0% Increase >2.00 D Cylinder 0.3% Pre-Op 20/20, Post-op 20/25 0.0% Induced Cylinder >2.00 D CK vs. Non-Contact LTK Post-op Month LTK1 CK2 1 Month 3.4% 3.0% 3 Months 1.4% 2.0% 6 Months 0.9% 1.0% 12 Months 0.2% 0.3% 1Sunrise LTK FDA Clinical Study, 2Conductive Keratoplasty 12-Month FDA Clinical Study Results. Summary Efficacy Variables FDA Guideline 6 Mos. (N = 352) 12 Mos. (N = 318) UCVA < 20/20 50% 45% 56% UCVA < 20/25 Not Stipulated 64% 75% UCVA < 20/40 85% 90% 92% MRSE + 0.50 50% 61% 63% MRSE + 1.00 75% 88% 89% Data from patients with single treatment. No retreatments included. Conductive Keratoplasty: Case Study • Preoperative – – – – – 50 year old Female African American Good health No ocular history – 6 mm pachymetry: 556 µm – IOP: 15 mm Hg • Preoperative – UCVAD: 20/125 – UCVAN: J12 – Manifest RX: + 3.25 – 0.75 X 130 – Cycloplegic RX: + 3.25 – 0.25 X 130 – BSCVAD: 20/25 Conductive Keratoplasty: Case Study • Operative – Instilled three drops topical anesthesia – Inserted lid speculum – Applied 32 treatment spots – Removed lid speculum – Instilled NSAID and antibiotic – Immediate K-Readings: • 51.75 @ 180 X 49.62 @90 Conductive Keratoplasty: Case Study • 1 Day Post-Operative – UCVAD: 20/32 – UCVAN: J7 – Manifest RX: + 1.50 – 0.50 X 120 – BSCVAD: 20/20 – BSCVAN: J2 – Slit Lamp: small epithelial defects Conductive Keratoplasty: Case Study • 1 Month Post-Operative – UCVAD: 20/20 – UCVAN: J2 – Manifest RX: - 0.25 – 0.75 X 125 – BSCVAD: 20/20 – BSCVAN: J1 – Slit Lamp Exam: WNL Conductive Keratoplasty: Case Study • 3 Month Post-Operative – UCVAD: 20/32 – UCVAN: J2 – Manifest RX: plano – 1.00 X 125 – BSCVAD: 20/16 – BSCVAN: J1 – Slit Lamp Exam: WNL Conductive Keratoplasty: Case Study • 6 Month Post-Operative – UCVAD: 20/30 – UCVAN: J2 – Manifest RX: + 0.25 – 0.75 X 125 – BSCVAD: 20/25 – BSCVAN: J1 – Slit Lamp Exam: WNL Conductive Keratoplasty: Case Study • 12 Month Post-Operative – UCVAD: 20/20 – UCVAN: J2 – Manifest RX: + 0.25 – 0.25 X 110 – BSCVAD: 20/16 – BSCVAN: J1 – Slit Lamp Exam: WNL Conductive Keratoplasty: Case Study • Preoperative – – – – 50 year old Female UCVAD: 20/125 UCVAN: J12 Manifest RX: + 3.25 – 0.75 X 130 – BSCVAD: 20/25 • 12 Months Post-op – UCVAD: 20/20 – UCVAN: J2 – Manifest RX: + 0.25 – 0.25 X 110 – BSCVAD: 20/16 No retreatment. Spherical correction only Corneal Topography: Case Study Preoperative 12 month Post-op Confocal View Of CK Folds Between Treatment Spots Sabry, McDonald, Klyce - 2001 Confocal View Of CK Deep CK Treatment With Healthy Endothelium Sabry, McDonald & Klyce - 2001 Cylindrical Footprint of CK Summary of Phase III Study • Highly effective – comparable to H-LASIK • Stability at 6 months • Safe – low rate induced cylinder • Penetration depth confirmed by histology, confocal microscopy Summary of Phase III Study • Topography shows central corneal steepening with mid-peripheral flattening • Visual axis spared • Multicenter study continues for two years