Surgical Op
advertisement

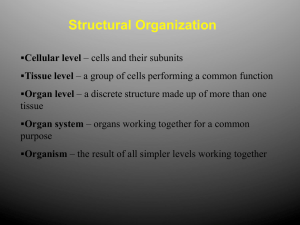
THEATRES & OPERATION NOTES Praneil Patel Obstetrics and Gynaecology SURGICAL OPERATION NOTES Objectives • Theatre etiquette • Format of the operation note • Tips • Common procedures for ST1 level THEATRE ETTIQUETTE • • • • WHO check list Introduce yourself to the team Establishes risk Enables Preparation WHO CHECK LIST - OBSTETRICS WHO CHECK LIST Surgery SURGICAL OPERATION NOTES • • • • Legal documentation No formal training Majority of operative notes are handwritten Important source for medical records – legal and financial implications ‘THE ADMIN’ Date of Procedure Patient details • Hospital sicker/hand write patient details Staff details • Operating Surgeon & grade • Surgical assistant & grade • Consultant overseeing care • Anaesthetist and grade THE SURGERY AND THE REASON The full title of the operation carried out • List from major to minor • No abbreviations Type of anaesthetic used. Indication for the procedure – pre operative diagnosis i.e. 8/40 Missed Miscarriage with Vaginal Bleeding ‘THE FINDINGS’ • • • • • • VE &abdominal palpation findings What was seen during the operation Post operative diagnosis Pathological findings Any relevant negative findings? As much detail as possible – site, size, colour, volume of structure involved • Picture aids • Any difficulties? • Blood Loss ‘THE PROCEDURE’ Surgical steps • Position • Prepped and draped • Incision (what instrument you used) • Step by step description of surgical steps undertaken • Sutures used and type of suturing (locking, continuous) • Written justification of unusual steps • Drains in situ / catheter – what is draining at end of procedure • Any samples obtained – how you took them • Swabs, needles and instrument checked POST OPERATIVE PLAN Important guidance on managing the patient in the post operative period Immediate • Analgesia • Medications • VTE assessment • Nutrition - fluids/ eating and drinking • Catheter management • Details of specific drains/dressing/packs/devices – when should they be removed • Samples for the lab • Routine post op care vs. close monitoring/ observations • Anaesthetic concerns THE POST OPERATIVE PLAN Hospital Stay • Suture / Staples care • Blood tests • Specific nursing/midwifery instructions • Any specialist input needed e.g. physio • Patient debrief – plan for future e.g. next delivery/contraception • Discharge – when and by whom • Follow up ‘THE SIGN OFF’ • Print your name [Stamp] • Sign the notes • Leave contact details Thank you Further Information Royal College of Surgeons of England Guidelines for Clinicians on Medical Records and Notes (1994) POSITION OF THE PATIENT Important medical legal detail • Appropriate position for access and to minimize complications e.g.. ulcers or nerve damage Common gynaecological patients’ positions Position Description Procedure Supine flat on back Caesarean section Abdominal hysterectomy Dorsal Lithotomy flat on back, buttocks at edge of bed Hips and knees fully flexed with legs in stirrups Perineal repair / Urogynae surgery ERPC Hysteroscopy Vaginal Hysterectomy Trandelenburg Flat on back with feet higher then head by 15-30 degrees Laparoscopy Abdominal hysterectomy Lloyd- Davies Trandelenburg position with hips flexed 15 degrees Laparoscopy Sacrocolpoplexy SURGICAL MANAGEMENT OF MISCARRIAGE ‘The admin’ ‘The surgery and the reason’ • • Gestation Rhesus status ‘The findings’ • VE – size of uterus, anteverted/retroverted, active bleeding, os open/closed • • • • Size of suction curette used Products seen Haemostasis EBL SURGICAL MANAGEMENT OF MISCARRIAGE ‘The procedure’ • • • • • • • • • • • Lithotomy position Prepped and draped Intermittent catheterization Cervix dilated – Hegar size Easy vs. difficult dilatation Size .... suction curettage used Evacuation of products Syntocinon given Cavity checked – what with and by whom EBL Haemostasis achieved (contracted uterus) SURGICAL MANAGEMENT OF MISCARRIAGE ‘The Post Operative Plan’ • • • • • • • • • • Analgesia +/Medication – antibiotics, Anti D Mobilize E+D Products – histology +/- FBC Monitor PVB loss Debrief on the ward vs. nurse led discharge Discharge follow up ‘The sign off’ DIAGNOSTIC HYSTEROSCOPY ‘The admin’ ‘The surgery and the reason’ ‘The findings’ • • • VE Vagina and vulva Uterine size, position, masses, bleeding • • • • • • Hysteroscopy Cervical canal – easy/difficult entry Utero-cervical length Uterus – cavity/ endometrium/ fibroids/ polyps – location and size Ostia EBL DIAGNOSTIC HYSTEROSCOPY ‘The Procedure’ • • • • • • • Dorsal Lithotomy position Prepped and draped Cervix dilated uterine ?size of cavity Normal saline hysteroscopy – hysteroscope inserted under direct vision Any additional steps – polypectomy, curetting, resection Repeat hysteroscopy following intervention ‘The Post Operative Plan’ • Analgesia • Mobilize • E+D • Monitor PV loss • Any biopsies/ tissue samples • Follow up plans ‘The sign off’ CAESAREAN SECTION The admin’ ‘The surgery and the reason’ • • Category for Emergency LSCS Indication for LSCS ‘The findings’ • Abdominal palpation • • VE Emergency LSCS – dilation, presentation, position, station • • • • • • • • • LSCS Difficult or unusual steps Adhesions Abdominal cavity findings (signs of obstruction/ appearance of lower segment) Presentation and position Liquor Placental delivery EBL Cord Gases CAESAREAN SECTION ‘The Procedure’ • • • • • • • • • • • • Supine position Prepped and draped Type of incision at skin Entry into abdominal cavity Bladder identified and reflected Type of incision to lower segment Delivery of baby – manual, forceps, any difficulty Delivery of placenta Uterine cavity check – empty Uterine angles – any extension Method of closure Swabbing of vagina / uterus contracted CAESAREAN SECTION ‘The Post Operative Plan’ • • • • • • • • Analgesia – e.g. PR given Medications – e.g. antibiotics, thromboprophylaxis, uterotonics Catheter management Details of specific drains/dressing/packs – when should they be removed Suture care Blood tests Midwifery instructions Patient debrief – plan for future e.g. next delivery/contraception ‘The sign off’