Does my child have a “flat” head?
advertisement

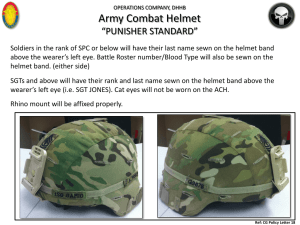
Does my child have a “flat” head? Lloyd Ellis & Anna Noisette The Royal Children’s Hospital, Melbourne Objectives of today’s session; Types of cranial asymmetry Identification of torticollis types Prevention Monitoring change RCH model Helmet therapy Resources/Questions Future? The Skull Craniosynotosis Fused Suture Name Description Sagittal Scaphocephaly Boat Skull Metopic Trigonocephaly Triangular Skull Unilateral Coronal Bicoronal Plagiocephaly Brachycephaly Lambdoid Plagiocephaly Asymmetric Skull Short Skull Asymmetric Skull Scaphocephaly Scaphocephaly Scaphocephaly Trigonocephaly Does my child have a “flat” head? What causes deformational Plagiocephaly? Prolonged pressure the skull in a particular position SIDS protocols “Back to sleep” Torticollis – a tightening of the neck muscles Macrocephaly Child resistant to ‘tummy time’ / muscle weakness Lack of education of prevention methods Utero constraints eg multiple births, insufficient pelvis The expanding brain applies an externally directed force, with the brain capable of extreme plastic deformation with no loss of function or intellect if volume is not reduced Sleeping Position • 1992 AAP recommended infants sleep supine/side to reduce SIDS risk • Revised 1996 – no sidelying sleeping • Victorian statistics: 1989 513 SIDs deaths/year 2000 140 SIDS deaths/year Incidence SIDS reduced significantly since inception of ‘Back to Sleep’ campaign (up to 40%) (Task Force on Sudden Infant Death Syndrome, 2005; Saeed et al., 2008; Xia et al., 2008; Losee & Mason, 2005). Dramatic increase (10-48%) in incidence of plagiocephaly since “Back to Sleep” campaign (Saeed et al., 2008; Habal et al., 2004; Persing et al., 2003; Xia et al., 2008). 13-15% singletons have some flattening Right side more common 1.3% incidence torticollis Deformity persists in 30% at 2 years Risk factors: found repeatedly • • • • • • • • • • Male First born Multiple pregnancy Prematurity Oligohydramnios Supine sleeping < 5 mins tummy time/day Delayed motor milestones Preferred head orientation for sleep at 6 weeks Positioning to same side for all bottle feeds Decreased Prone Play • Decreased awareness of the importance of supervised ‘tummy time’, extended time on back • WHY? • Parental fears • Infant intolerance Treatment of Plagiocephaly Wait and See! If torticollis present, treat with physiotherapy/gentle stretching Counter positioning • Changing the forces on the head by altering the lying position Cranio-reshaping helmet therapy • Fitting a custom made helmet which is worn for 23/34 hours a day until improved cosmesis is achieved Classifications • Macdonald 1969 gave 3 classifications: • Sternomastoid tumour group (42.7%) • palpable mass present • Muscular torticollis group (30.6%) • tight SCM but no palpable mass • Reduced active/passive ROM • Postural torticollis group (22.1%) • no palpable mass or tightness • Full active/passive ROM Congenital Muscular Torticollis (CMT) • CMT usually presenting with unilateral tightness of the sternocleidomastoid (SCM) muscle (Luther, 2002) • Characterised by lateral flexion to the affected side and rotation away from the affected side Physiotherapy Rx • Goals of Physiotherapy: • increase PROM • increase AROM • Improving facial and cranial symmetry • Encourage gross motor development • Education, Stretching, Counter positioning techniques including positions carrying and for play Counter Positioning • Parent education • Active and consistent repositioning of infant during play to apply pressure to prominent part of the skull • Use of passive devices to position baby, specially designed devices Counter positioning Positioning, play and carrying techniques to encourage movement to ‘neglected side’ and lengthen tight muscles Variety of positions for play • Supervised ‘tummy time’ whilst the infant is awake • Head shape and motor development are affected by sleep and awake positions of infant Prevention is the key ! Key Preventative Strategies 1. Early detection of torticollis & referral to Physiotherapy 2. Encourage prone & side-lying during supervised awake play periods several times per day 3. Nightly/weekly alternating head positioning during supine sleeping 4. Avoid prolonged repetitive positioning (e.g. Car seat carriers, buggies, baby swings & bouncers. 5. Regularly change position of cot in room or toys/mobiles around cot. 6. Counter positioning / alternating the orientation of infant in the cot 7. Alternating feeding positions. (Saeed et al., 2008; Task Force on Sudden Infant Death Syndrome, 2005; Neufeld & Birkett, 1999; Persing et al., 2003; van Vlimmerman et al., 2008., Canadian Paediatric Society, 2001). Assessment • • • • • History Examination Severity scoring Measurement Closure of anterior fontanelle • Range 4 to 18m Clinical Severity Score RCH treatment model • Research into the effectiveness of conservative management is just beginning • • • • • 3d Capture Counterpositioning: initial treatment Follow-up 3d review Physiotherapy: if torticollis present Orthotic management: for severe cases in older infants (from 6/12 old) To treat or not to treat? • Cosmetic condition • Studies have shown that helmets improve the • • • • head shape No study has been conducted to see if the condition self corrects regardless of treatment Who should we treat ? Last resort when conservative management fails. They are not an ‘easy’ option Significant time and resource costs for health services and families Indications for referral to RCH Deformational Plagiocephaly Clinic • • • • Failure of early treatment strategies Severe deformity Severe torticollis and restriction Associated medical conditions • Prematurity • Developmental delay Helmet Therapy • Do not affect the growing brain • Not the easy option! • They are a significant cost in time and resources for families • For most children they shouldn’t be required RCH treatment protocol: To qualify a child must: • Have a deformational score of 6 or greater on the • • • • assessment sheet or Score a 3 in a single deformation change Be at least 6 months old Have no craniosynostosis Helmets do not treat torticollis! How does it work? Wearing Regime Helmet is worn in gradually over 3-7 days (day time only), then worn 23/24 for duration of treatment Review every 4-6 weeks according to growth • Repeating 3D photos mid treatment and end of treatment The Finished product The process • 3D photography using 5 point camera • Use to manufature helmet • Baseline to see shape improvement Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Helmet Therapy Positional Therapy Positional Therapy Positional Therapy Positional Therapy 7mths 8.5mths Positional Therapy 8mths 9.5 mths 24mths 12mths 5yrs Deformational Plagiocephaly - Mild Deformational Brachycepahley - Mild Deformational Plagiocephaly – Moderate / Serve Deformational Plagiocephaly – Moderate / Serve Deformational Plagiocephaly – Moderate / Serve Deformational Plagiocephaly – Moderate / Serve RCH - What are we doing? • Development of brochure & poster: - ‘Back to Sleep – Tummy Time to Play • ‘How to Protect Your Baby’s Head Shape’ • Available from APA • Plagiocephaly Fact sheet for parents – RCH website • Plagiocephaly Clinic Future Objectives Educational material on positional plagiocephaly to: • Raise awareness • Early recognition • Early management • Prevention Further research required in: • Natural history of plagiocephaly • Severity rating of plagiocephaly • Objective outcome measures Conclusion • Early detection of deformational plagiocephaly within 6-10wks and positional therapies followed there is a greater degree of avoiding helmet therapy. Acknowledgements • Sharon Vladusic, Senior Physiotherapist, Orthopaedic Department, RCH • Dr. Susie Gibb, Consultant Paediatrician, Department of General Paediatrics, RCH • Angela Serong, Senior Physiotherapist, RCH Questions? References Canadian Paediatric Society. (2001). CPS Statement Update: Positional plagiocephaly and sleep positioning: an update to the joint statement on sudden infant death syndrome. Paediatr Child Health, 6, 788-789. De Ribaupierre S et al. Posterior plagiocephaly treated with cranial remodeling orthosis. Swiss med Weekly 2007; 137: 368-72. Habal, M.B., Castelano, C., Hemkes, N., Scheuerle, J., & Guilford, A. M. (2004). Clinical Note: In search of causative factors of deformational plagiocephaly. The Journal of Craniofacial Surgery, 15, 835-841. Losee, J.E., & Mason, A.C. (2005). Deformational plagiocephaly: diagnosis, prevention and treatment. Clin Plastic Surg, 32, 53-64 Neufeld, S., & Birkett, S. (1999). Clinical Notebook. Positional plagiocephaly: a community approach to prevention and treatment. Alta RN, Jan-Feb, 55, 1516. NHS Quality improvement Evidence note 16: The use of cranial orthosis treatment for infant deformational plagiocephaly, Scotland, 2007. Persing, J., James, H., Swanson, J., Kattwinkel, J. (2003). Prevention and management of positional skull deformities in infants. Pediatrics, 112, 199202. Saeed, N.R., Wall, S.A., & Dhariwal, D. K. (2008). Management of positional plagiocephaly. Arch Dis Child, 93, 82-84. Steinbok P et al. Long term outcome of infants with positional plagiocephaly. Childs Nervous System 2007: 23: 1275-83. Task Force on Sudden Infant Death Syndrome. (2005). The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleep environment, and new variables to consider in reducing risk. Pediatrics, 116, 1245-1255. Van Vlimmeren LA et al. (2007). Risk Factors for Deformational Plagiocephaly at birth and 7 weeks of age: A prospective cohort study, Pediatrics ,119; 2:20062012. Van Vlimmeren LA et al (2008). Effect of Pediatric physical therapy on deformational plagiocephaly in children with Positional preference. A randomized controlled trial, Arch Ped Adol Med ,162;8:712-718. . Xia, JJ et al. (2008). Nonsurgical treatment of deformational plagiocephaly, a systematic review. Arch Ped Adol Med,162; 8: 719-20.