Acute Coronary Syndrome
advertisement
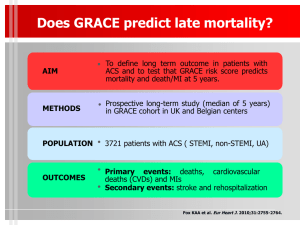
Acute Coronary Syndrome Steven R. Bruhl MD, MS 3rd Year Cardiology Fellow Internal Medicine Didactics July 14, 2010 Goals and Objectives Discuss the definition & pathophysiology of ACS Recognize the clinical features of low, intermediate and high risk ACS Be able to identify and treat patients appropriate for a conservative or invasive strategy Discuss new and controversial pharmacological treatments Gold Standard for Treatment of ACS ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction http://circ.ahajournals.org/cgi/content/full/102/10/1193 Algorithm for evaluation and management of patients suspected of having ACS. Anderson JL, et al. J Am Coll Cardiol 2007;50:e1–e157, Figure 2. ACS Overview Overview of ACS Assessment of “Likelihood of ACS” Early Risk Stratification Invasive vs Conservative Strategy Pharmacotherapy Long-term Therapy/Secondary Prevention Scope of the Problem 5 million ER visits nationwide for CP 800,000 experience an MI each year 213,000 die from their event ½ of those die before reaching the ER Pre-CCU, mortality for MI was >30% Fell to 15% with CCU With current interventions, in hospital mortality of STEMI is 6-7% Overview of ACS Acute Coronary Syndromes* 1.57 Million Hospital Admissions - ACS UA/NSTEMI† STEMI 1.24 million 0.33 million Admissions per year Admissions per year *Primary and secondary diagnoses. †About 0.57 million NSTEMI and 0.67 million UA. Heart Disease and Stroke Statistics – 2007 Update. Circulation 2007; 115:69–171. Acute Coronary Syndrome (ACS) Definition: The spectrum of acute ischemia related syndromes ranging from UA to MI with or without ST elevation that are secondary to acute plaque rupture or plaque erosion. [----UA---------NSTEMI----------STEMI----] Pathophysiology of Stable Angina and ACS Pathophysiology ACS •Anemia •Plaque rupture/clot Increased O2 Demand O2 supply/demand mismatch→Ischemia Myocardial ischemia→necrosis Angina •Flow- limiting stenosis Asymptomatic Decreased O2 Supply Pathophysiology of ACS Evolution of Coronary Thrombosis Unstable Angina Non occlusive thrombus Non specific ECG Normal cardiac enzymes NSTEMI Non-occlusive thrombus sufficient to cause tissue damage & mild myocardial necrosis STEMI Complete thrombus occlusion ST elevations on ECG or new LBBB ST depression +/T wave inversion on ECG Elevated cardiac enzymes Elevated cardiac enzymes More severe symptoms STEMI Name 3 situations in which you cannot diagnose STEMI STEMI Name 3 situations in which you cannot diagnose STEMI Left Ventricular Hypertrophy Chronic or Rate Dependent LBBB Paced Rhythm Cardiac Catheterization Name the only 3 situations that demand emergent cardiac catheterization. Cardiac Catheterization Name the only 3 situations that demand emergent cardiac catheterization. STEMI or new LBBB ACS with hemodynamic or electrical instability despite optimal medical management Uncontrolled CP despite optimal medical management Diagnosis of ACS At least 2 of the following History ( angina or angina equivalent) Acute ischemic ECG changes Typical rise and fall of cardiac markers Absence of another identifiable etiology Initial Evaluation and management of Non ST-elevation ACS Initial Evaluation and Management •History and Physical •ECG •Cardiac Biomarkers Establish the Likelihood that Clinical Presentation Represents an ACS Secondary to CAD Risk Stratify for Short-term Adverse Outcomes Likelihood of ACS by Hx/PE History/Examination Suggesting AMI Pain in Chest or Left Arm CP Radiation Right Shoulder Left Arm Both Left & Right Arm Diaphoresis 3rd Heart Sound SBP < 80 mm Hg Pulmonary Crackles Panju AA. JAMA. 1998;280:1256. LR 2.7 LR 2.9 (1.4-6.0) LR 2.3 (1.7-3.1) LR 7.1 (3.6-14.2) LR 2.0 (1.9-2.2) LR 3.2 (1.6-6.5) LR 3.1 (1.8-5.2) LR 2.1 (1.4-3.1) Likelihood of ACS by Hx/PE Clinical Examination – Pleuritic Chest Pain Sharp or Stabbing Pain Positional Chest Pain Reproducible Chest Pain Against AMI LR 0.2 (0.2-0.3) LR 0.3 (0.2-0.5) LR 0.3 (0.2-0.4) LR 0.2-0.4 Panju AA. JAMA. 1998;280:1256. Risk Stratification by ECG Simple, quick, noninvasive tool Universally available, cheap Correlates with risk and prognosis Guides treatment decisions Can identify alternative causes Risk Stratification by ECG ECG Findings and Associated LR for AMI New ST-E > 1mm New Q waves Any ST-E New Conduction Defect New ST-D LR 5.7-53.9 LR 5.3-24.8 LR 11.2 (7.1-17.8) LR 6.3 ( 2.5-15.7) LR 3.0-5.2 NORMAL ECG LR 0.1-0.4 Panju AA. JAMA. 1998;280:1256. Risk Stratification by ECG CAVEATS 1-8% AMI have a normal ECG Only Approx 50% of AMI patients have diagnostic changes on their initial ECG Peter J. Zimetbaum, M.D., N Engl J Med 2003;348:933-40. Risk Stratification by ECG CAVEATS cont. 1 ECG cannot exclude AMI Brief sample of a dynamic process Small regions of ischemia or infarction may be missed Peter J. Zimetbaum, M.D., N Engl J Med 2003;348:933-40. How Sensitive is the ECG Alone? How Predictive is NTG response? Timing of Release of Various Biomarkers After Acute Myocardial Infarction Shapiro BP, Jaffe AS. Cardiac biomarkers. In: Murphy JG, Lloyd MA, editors. Mayo Clinic Cardiology: Concise Textbook. 3 rd ed. Rochester, MN: Mayo Clinic Scientific Press and New York: Informa Healthcare USA, 2007:773–80. Anderson JL, et al. J Am Coll Cardiol 2007;50:e1–e157, Figure 5. Risk Stratification by Troponin 7.5 % Mortality at 42 Days 8 7 6.0 % 6 5 4 3 2 1 1.0 % 831 3.4 % 3.7 % 148 134 1.7 % 174 50 67 0 0 to <0.4 0.4 to <1.0 1.0 to <2.0 2.0 to <5.0 5.0 to <9.0 Cardiac troponin I (ng/ml) 9.0 Non ACS causes of Troponin Elevation 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Trauma (including contusion; ablation; pacing; ICD firings,, endomyocardial biopsy, cardiac surgery, after-interventional closure of ASDs) Congestive heart failure (acute and chronic) Aortic valve disease and HOCM with significant LVH Hypertension Hypotension, often with arrhythmias Noncardiac surgery Renal failure Critically ill patients, especially with diabetes, respiratory failure Drug toxicity (eg, adriamycin, 5 FU, herceptin, snake venoms) Hypothyroidism Coronary vasospasm, including apical ballooning syndrome Inflammatory diseases (eg, myocarditis, Kawasaki disease, smallpox vaccination, Post-PCI Pulmonary embolism, severe pulmonary hypertension Sepsis Burns, especially if TBSA greater than 30% Infiltrative diseases: amyloidosis, hemachromatosis, sarcoidosis, and scleroderma Acute neurologic disease, including CVA, subarchnoid bleeds Rhabdomyolysis with cardiac injury Transplant vasculopathy Vital exhaustion Modified from Apple FS, et al Heart J. 2002;144:981-986. Combined Sensitivities for ACS Early Invasive Conservative Unstable angina/NSTEMI cardiac care Evaluate for conservative vs. invasive strategy based upon: Likelihood of actual ACS Risk stratification by TIMI risk score ACS risk categories per AHA guidelines Low High Intermediate TIMI Risk Score Predicts risk of death, new/recurrent MI, need for urgent revascularization within 14 days TIMI Risk Score T: Troponin elevation (or CK-MB elevation) H: History or CAD (>50% Stenosis) R: Risk Factors: > 3 (HTN, Hyperlipidemia, Family Hx, DM II, Active Smoker) E: EKG changes: ST elevation or depression 0.5 mm concordant leads A2:Aspirin use within the past 7 days; Age over 65 T: Two or more episodes of CP within 2 hours Deciding between Early Invasive vs a Conservative Strategies Definitive/Possible ACS Initiate ASA, BB, Nitrates, Anticoagulants, Telemetry Early Invasive Strategy • TIMI Risk Score >3 • New ST segment deviation • Positive biomarkers •Hemodynamic instability •Elecrical instability •Refractory angina •PCI in past 6 months •CABG •EF <40% Coronary angiography (24-48 hours) Conservative Strategy •TIMI Risk Score <3 (Esp. Women) •No ST segment deviation •Negative Biomarkers Recurrent Signs/Symptoms Heart failure Arrhythmias Remains Stable ↓ Assess EF and/or Stress Testing ↓ EF<40% OR Positive stress Go to Angiography Specifics of Early Hospital Care Anti-Ischemic Therapy Anti-Platelet Therapy Anticoagulant Therapy Early Hospital Care Anti-Ischemic Therapy Class I Bed/Chair rest and Telemetry Oxygen (maintain saturation >90%) Nitrates (SLx3 Oral/topical. IV for ongoing iscemia, heart failure, hypertension) Oral B-blockers in First 24-hours if no contraindications. (IV B-blockers class IIa indication) Non-dihydropyridine Ca-channel blockers for those with contraindication fo B-blockers ACE inhibitors in first 24-hours for heart failure or EF<40% (Class IIa for all other pts) (ARBs for those intolerant) Statins Early Hospital Care Anti-Ischemic Therapy Class III Nitrates if BP<90 mmHg or RV infarction Nitrates within 24-hrs of Sildenafil or 48 hrs of Tadalafil Immediate release dihydropyradine Ca-blockers in the absence of B-Blocker therapy IV ACE-inhibitors IV B-blockers in patients with acute HF, Low output state or cardiogenic shock, PR interval >0.24 sec, 2nd or 3rd degree heart block, active asthma, or reactive airway disease NSAIDS and Cox-2 inhibitors Early Hospital Care Anti-Platelet Therapy Class I Aspirin (162-325 mg), non enteric coated Clopidogrel for those with Aspirin allergy/intolerance (300-600 mg load and 75 mg/d) GI prophylaxis if a Hx of GI bleed GP IIb/IIIa inhibitors should be evaluated based on whether an invasive or conservative strategy is used GP IIb/IIIa inhibitors recommended for all diabetics and all patient in early invasive arm Early Hospital Care Anticoagulant Therapy Class I Unfractionated Heparin Enoxaparin Bivalarudin Fondaparinux Relative choice depends on invasive vs conservative strategy and bleeding risk Early Hospital Care Statin Therapy MIRACL Trial Inclusion Criteria 3086 patients with Non ST ACS Total cholesterol <270 mg/dl No planned PCI Randomized to Atorvastatin vs Placebo Drug started at 24-96 hours Statin Evidence: MIRACL Study Primary Efficacy Measure Placebo Cumulative Incidence (%) 15 17.4% 14.8% Atorvastatin 10 Time to first occurrence of: • Death (any cause) • Nonfatal MI • Resuscitated cardiac arrest • Worsening angina with new objective evidence and urgent rehospitalization 5 Relative risk = 0.84 P = .048 95% CI 0.701-0.999 0 0 4 8 12 Time Since Randomization (weeks) Schwartz GG, et al. JAMA. 2001;285:1711-1718. 16 Statin Evidence: MIRACL Study Fatal and Nonfatal Stroke Cumulative Incidence (%) 2 Placebo 1.5 1 Atorvastatin 0.5 Relative risk = 0.49 P = .04 95% CI 0.24-0.98 0 0 4 8 12 16 Time Since Randomization (weeks) Waters DD, et al. Circulation. 2002;106:1690-1695. S24 PROVE-IT Trial All-Cause Death or Major CV Events in All Randomized Subjects 30 Pravastatin 40mg (26.3%) 25 20 % with 15 Event Atorvastatin 80mg (22.4%) 10 16% RR (P = 0.005) 5 0 0 3 6 9 12 15 18 21 Months of Follow-up 24 27 30 Summary of PROVE-IT Results In patients recently hospitalized within 10 days for an acute coronary syndrome: “Intensive” high-dose LDL-C lowering (median LDL-C 62 mg/dL) compared to “moderate” standard-dose lipid-lowering therapy (median LDL-C 95 mg/dL) reduced the risk of all cause mortality or major cardiac events by 16% (p=0.005) Benefits emerged within 30 days post ACS with continued benefit observed throughout the 2.5 years of follow-up Benefits were consistent across all cardiovascular endpoints, except stroke, and most clinical subgroups Invasive vs Conservative Strategies Invasive vs Conservative Strategy Clinical Trials ISARCOOL VANQWISH (98) ICTUS (05) RITA-3 (02) MATE VINO TIMI IIIB (94) TRUCS TACTICSTIMI 18 (01) Weight of the evidence Conservative Strategy Favored N=920 No difference N=2,874 FRISC II (99) Invasive Strategy Favored N=7,018 How Early is Early? Secondary Prevention Class I Indications Aspirin Beta-blockers: (all pts, slow titration with moderate to severe failure ACE-Inhibitors: CHF, EF<40%, HTN, DM (All pts-Class IIa) ARB when intolerant to ACE. (Class IIa as alternative to ACEI) Aldosterone blockade: An ACEI, CHF with either EF<40% or DM and if CrCl>30 ml/min and K<5.0 mEq/L Statins Standard Risk Factor Management Long-Term Antithrombotic Therapy at Hospital Discharge after UA/NSTEMI New UA/NSTEMI Patient Groups at Discharge Medical Therapy without Stent ASA 75 to 162 mg/d indefinitely (Class I, LOE: A) Bare Metal Stent Group Drug Eluting Stent Group ASA 162 to 325 mg/d for at least 1 month, then 75 to 162 mg/d indefinitely (Class I, LOE: A) & & Clopidogrel 75 mg/d for at least 1 month and up to 1 year (Class I, LOE:B) Clopidogrel 75 mg/d at least 1 month (Class I, LOE: A) and up to 1 year (Class I, LOE: B) ASA 162 to 325 mg/d for at least 3 to 6 months, then 75 to 162 mg/d indefinitely (Class I, LOE: A) & Clopidogrel 75 mg/d for at least 1 year (Class I, LOE: B) Indication for Anticoagulation? Yes Add: Warfarin (INR 2.0 to 2.5) (Class IIb, LOE: B) No Continue with dual antiplatelet therapy as above Anderson JL, et al. J Am Coll Cardiol 2007;50:e1–e157, Figure 11. INR = international normalized ratio; LOE = level of evidence. Secondary Prevention Class III Hormone Replacement Therapy Antioxidants (Vit C, Vit E) Folic Acid New and Controversial Drug Therapies Early Treatment with Clopidogrel Shortcomings of the CURE Trial Conducted primarily at centers without routine use of early invasive strategy Only 462 (3.7%) patients enrolled from the U.S. 44% had catheterization during index hospitalization Adverse event reduced only in nonfatal MI set Major Bleeding rate of 9.6% among patients who were administered clopidogrel within 5 days of CABG Clopidogrel Bleeding Risk and CABG “In hospitals in which patients with UA/NSTEMI undergo rapid diagnostic catheterization within 24 hours of admission, clopidogrel is not started until it is clear that CABG will not be scheduled within the next several days. However, unstable patients should receive clopidogrel or be take for immediate angiography.” Clopidogrel vs. Prasugrel Prasugrel-Key Facts Contraindicated in pts with prior TIA/Stroke Not recommended for patients >75 years 5 mg maintenance dose suggested in patients <60 Kg, though this dose has not been studied Summary ACS includes UA, NSTEMI, and STEMI Management guideline focus Immediate assessment/intervention (MONA+BAH) Risk stratification (UA/NSTEMI vs. STEMI) RAPID reperfusion for STEMI (PCI vs. Thrombolytics) Conservative vs Invasive therapy for UA/NSTEMI Aggressive attention to secondary prevention initiatives for ACS patients Beta blocker, ASA, ACE-I, Statin Questions?