Malpractice, Clinical Practice Guidelines and
Expert Witnesses: A Case Report
Richard L. Elliott, MD, PhD, FAPA
Professor and Director of Medical Ethics
Mercer University School of Medicine
Adjunct Professor
Mercer University School of Law
PowerPoint on Abuse and Impairment
on Ethics site
Need repeat lecture for Savannah?
Case Report: Initial Contact
Phone call from US Attorney’s office
Teenager prescribed Prozac
Found hanging
Allegation: Failure to warn parents about suicidality
Response: Ask about identities of others, need for
report
Agreement: Review records
Fee: $350/hr record review, consultation, testimony
No retainer
Never a contingency fee
Case Report
16 year-old girl prescribed Prozac 10 mg on
January 26, 2006 for “depression”
February 18, 2006, found hanging in closet
Anoxic brain injury
Died May 2006 from complications
Suit filed in Federal Court
– Bench trial
– Daubert rules
Goals
Rule #1
What is a tort?
–
Medical errors and negligence
Malpractice
– Reasons for malpractice
– Causes – Dx, Rx, informed consent, trainee issues (handoffs)….
Standards of care
–
–
Why do we have a tort system?
Clinical Practice Guidelines
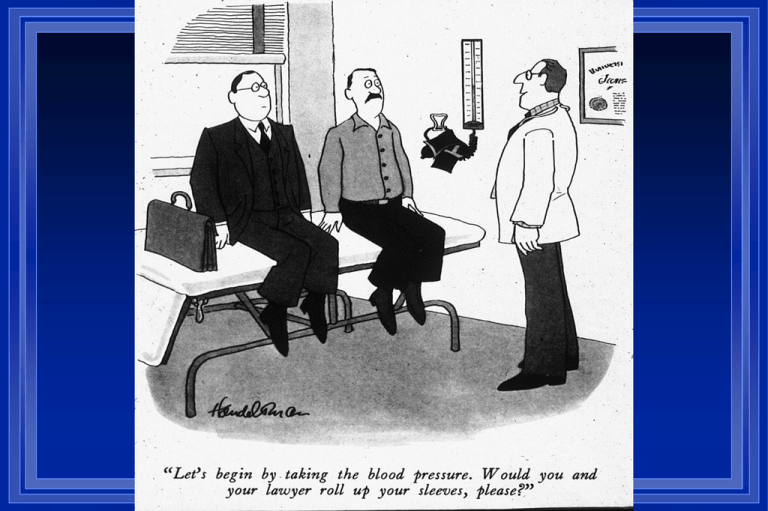
Expert witnesses
Tort reform
Telling patients about errors
Reducing risk Rule #1
– Communication
Rule #1
We are doctors
– (not lawyers, mostly)
– Think clinically
– Let information about risk management
inform you, but do not become overly
defensive
What is malpractice?
A civil, not criminal legal issue
– No imprisonment
A tort
– Breach of duty owed to another individual other
than breach of contract
– Motor vehicle accidents, slander, medical
malpractice, others
– Purpose: to make injured party whole and to
discourage such conduct
Some tortious acts may not be malpractice and not
covered by insurance – sex with patients
Nature of Legal Claim
Civil suit - tort
– Decision based on preponderance of
evidence
– Must have statement from expert for
plaintiff on which to base claim
Case Report - Legal Claim
Malpractice
– Failure to warn patient/parents of
increased risk of suicide associated with
Prozac
– Failure to monitor patient closely
What is malpractice?
The Four Ds:
– Dereliction of
– Duty
– Directly causing
– Damage
Know this!
Four Ds in Our Case
Four D’s of malpractice
– Dereliction of Duty Directly causing Damage
– Was there a duty?
• To properly diagnose and treat
• To inform patient of risks
• Informed consent in Georgia
– Was there dereliction of duty? (failure to meet standard of
care)
– Were there damages?
• Anoxic brain injury
• Financial
– Was Prozac responsible, or were there intervening causes?
• Does Prozac cause suicide?
• Did Prozac cause suicide in this case?
Malpractice and the Four Ds
Dereliction of
Duty
Directly causing
Damage
Was there a duty of care?
Jessica was a patient, records were
kept, patient assessed, medication
prescribed
Was there a duty to inform?
Informed consent in Georgia
– General informed consent overturned 2009
Mother was a nurse
– Ought she to have known the risks?
– Defendant claimed to have informed, but
did not documented
Malpractice and the Four Ds
Dereliction of
Duty
Directly causing
Damage
Negligence and Claims
Harvard Study cited in Studdert
– 2% negligent injuries resulted in claims
– 17% claims resulted from negligent injuries
63% settled claims involve negligence
IOM
– 72.6% of adverse events NOT due to
negligence
– >90% errors do not lead to action
– 30-40% malpractice claims without
negligence
Was there a dereliction of duty?
Dereliction means breach of standard of
care
Standard of Care
“degree of skill and care which under
similar conditions and like surrounding
circumstances is ordinarily employed by
the medical profession generally”
What determines the Standard of Care?
Res ipsa loquitur
Clinical Practice Guidelines
Recommendations of consultants
Testimony of expert witnesses
Can expert witnesses say anything?
– The problem of “junk science”
Other documents, laws, standards
– FDA warning
Daubert and Constraints on Expert Testimony
Testimony must assist trier of fact to understand
evidence or determine a fact
Expert qualified by knowledge, skill, training,
experience, or education
Testimony based upon sufficient facts or data
Testimony is the product of reliable principles or
methods
Witness has applied those principles and methods to
the facts of the case
Does the FDA establish the Standard of Care?
"Antidepressants increased the risk of suicidal
thinking and behavior (suicidality) in short-term
studies in children and adolescents with Major
Depressive Disorder (MDD) and other psychiatric
disorders. Anyone considering the use of [Drug
Name] or any other antidepressant in a child or
adolescent must balance this risk with the clinical
need. Patients who are started on therapy should be
observed closely for clinical worsening, suicidality, or
unusual changes in behavior."
What is “suicidality?”
No deaths in 22 studies reviewed by
FDA including over 4400 patients
Placebo overdoses less likely to be
reported than drug overdoses
Confusion among panel members
FDA Advisory Committee on “Suicidality”
Dr. Irwin “Is there a word suicidality?”
Dr. Goodman (Chair) “Every time I write it in Word it gets red
underlined.”
Dr. Irwin “I am not certain anyone really knows what it is we are
saying, what we are voting on”
Ms Griffith (patient representative) “It’s not in Webster’s”
Dr. Irwin “I think it may lead to a kind of misrepresentation”
Dr. Goodman “I am interested in what parents think when they
read “suicidality” – my guess is they are going to think “suicide””
Dr. Goodman (later) “Hopefully the public will understand what
we mean, specifically that we are not talking about completed
suicide”
What was the standard of care?
Bhatia – 2008
– Surveyed 1521 physicians in Nebraska
– 96.8% aware of FDA warning
– 76.9 prescribed antidepressants to children
and adolescents
– 31.9% saw patients more frequently, only
7.5% saw weekly
Malpractice and the Four Ds
Dereliction of
Duty
Directly causing
Damage
Damages
Hanging leading to anoxic brain injury
and ultimately death
Financial costs of care
Loss of lifetime earnings
Non-economic damages
Predictor of Payment
Harvard New York data
– Key predictor of payment for malpractice
claim was degree of plaintiff disability, not
degree of negligence
Georgia’s Cap on non-Economic Damages
Overturned by Georgia Supreme Court
2010
Malpractice and the Four Ds
Dereliction of
Duty
Directly causing
Damage
Did Prozac directly cause Jessica’s death?
Does Prozac cause suicide?
– General causation
– Specific to the case
Were there intervening causes?
– “But for” test
Does Prozac Cause Suicide in Adolescents?
No deaths in data reported to FDA
– 22 RCT, 4400 patients
– RCT not helpful means of studying relationship between
SSRI and suicide
• Small numbers, high risk screened out, short time
Teen suicides rarely have antidepressant in blood
– Dudley et al 2010 574 adolescent suicides, SSRI present
1.6% Australasia Psychiatry June p. 242
Declining rates of prescription associated with increasing
rates of suicide
– 33% decline in suicides in 1990s while SSRI increasing
– Compare county/state SSRI use and suicide rates show
increasing prescription rates associated with lower suicide
rates
Does Prozac cause suicide in adolescents?
No credible evidence that, in general,
Prozac causes suicide (as opposed to
“suicidality”) in adolescents
Did Prozac cause Jessica to commit suicide?
Lack of general causation
Intervening causes
– Medication prescribed January 26
– Break-up with boyfriend February 14
– 40 minute phone call February 18
– Hanging minutes after phone call
Case Weaknesses
Poor documentation
– Single word “depressed”
Black box warning from FDA 2004
Young girl
– Sympathy factor
Case Strengths
Lack of clear evidence for general causation
Intervening causes
– Cell phone records, mother’s deposition, boy
friend testimony, linking hanging to break-up with
boyfriend
Mother described Jessica as depressed, and
attributed hanging to break-up
Mother as nurse – to what extent should she have
been aware of warning?
Red Herrings
Jessica described as “Goth”
Outcome of Legal Case
Mediation June 17, 2010
– Plaintiffs had previously rejected mediation
No ruling as of 11/1/10
Clinical Recommendations
Suicide should always be considered
when prescribing an antidepressant
“Warning” – don’t need to link to
antidepressant, just advise to observe
for worsening, including suicidal
thoughts/behaviors
Follow-up
Three Pillars of Protection against suits
Communication with patient and family
Consultation - Rule #1 – clinical utility
– If you disagree with consultant, resolve – no chart fights
Documentation
– Not more, but more appropriate
– Rule #1 – documentation should be clinically
relevant, not merely CYA
– NEVER alter records
– Documentation after an incident should be viewed
in light of potentially public nature
Rules for Expert Witnesses
Agree only to review a case
Retainers are ethical
Contingency fees are not ethical
Avoid creating a doctor-patient
relationship as an expert witness
Make concerns about case or your
participation known ASAP
Tort Reform I
Malpractice – 2-3% of healthcare costs
Costs of malpractice insurance not tied solely
to physician risk
Goals of tort reform
– Reduce costs of insurance
– Reduce disincentives to practice (e.g., OB)
– Reduce costs and risks of defensive
medicine
Tort Reform Proposals
Cap non-economic damages
Health courts
– Neutral experts, greater expertise
– Evidence-Based Medicine
– Analogous to workers’ compensation
Limit attorney contingency fees
Losing plaintiff pays all costs
Eliminate “joint and several” liability
2010 9/574 (1.6%) adolescent suicides
exposed to SSRIs
Were there intervening causes?
Medication prescribed January 26
Break-up with boyfriend February 14
40 minute phone call February 18
Hanging minutes after phone call
Annual Suicide Rates for Males and Females Aged 10 to 19 Years, U.S., 1996 - 2005
.
Copyright restrictions may apply.
We're would like to expose the
students to information regarding
malpractice, evidence-based
practice, and standards of care, i.e.,
what legal implications are there
when physicians fail to follow such
standards. Perhaps a case or two?
2030 BC when the Code of
Hammurabi provided that “If the
doctor has treated a gentlemen with
a lancet of bronze and has caused
the gentleman to die, or has opened
an abscess of the eye for a
gentleman with a bronze lancet, and
has caused the loss of the
gentleman’s eye, one shall cut off
his hands
In 1532, during the reign of Charles
V, a law was passed that required
the opinion of medical men to be
taken formally in every case of
violent death; this was the precursor
to requiring expert testimony from a
member of the profession in medical
negligence claims, to establish the
standard of care.
In the United States, medical malpractice suits first
appeared with regularity beginning in the 1800s [3].
However, before the 1960s, legal claims for
medical malpractice were rare, and had little impact
on the practice of medicine [21]. Since the 1960s
the frequency of medical malpractice claims has
increased; and today, lawsuits filed by aggrieved
patients alleging malpractice by a physician are
relatively common in the United States. One survey
of specialty arthroplasty surgeons reported that
more than 70% of respondents had been sued at
least once for medical malpractice during their
career
Medical malpractice is defined as any act or omission by a physician during
treatment of a patient that deviates from accepted norms of practice in the
medical community and causes an injury to the patient. Medical malpractice is a
specific subset of tort law that deals with professional negligence. “Tort” is the
Norman word for “wrong,” and tort law is a body of law that creates and
provides remedies for civil wrongs that are distinct from contractual duties or
criminal wrongs [24]. “Negligence” is generally defined as conduct that falls
short of a standard; the most commonly used standard in tort law is that of a socalled “reasonable person.” The reasonable person standard is a legal fiction,
created so the law can have a reference standard of reasoned conduct that a
person in similar circumstances would do, or not do, in order to protect another
person from a foreseeable risk of harm.
In the United States, medical malpractice law is under the authority
of the individual states; the framework and rules that govern it
have been established through decisions of lawsuits filed in state
courts. Thus, state law governing medical malpractice can vary
across different jurisdictions in the United States, although the
principles are similar. In addition, during the last 30 years, statutes
passed by states’ legislatures have further influenced the
governing principles of medical malpractice law. Thus medical
malpractice law in the United States is based on common law,
modified by state legislative actions that vary from state to state.
One exception to medical liability can arise in the context of
those who volunteer assistance to others who are injured or ill;
this exception is embodied in “Good Samaritan” laws that
address bystanders’ fear of being sued or prosecuted for
unintentional injury or wrongful death, In the United States, Good
Samaritan laws vary from jurisdiction to jurisdiction and specify
who is protected from liability and the circumstances pertaining
to such protection. In general, Good Samaritan statutes do not
require any person to give aid to a victim, although a handful of
states, such as Vermont and Minnesota, specify a duty to provide
reasonable assistance to an
Medical Liability Claim Frequency by Specialty,2007-2008
% Ever Sued
General & family practice
38.9%
General internal medicine
34.0%
Internal medicine sub-specialties 40.2%
General surgery
69.2%
Surgical sub-specialties
57.0%
Pediatrics
27.3%
Obstetrics/gynecology
69.2%
Radiology
47.4%
Psychiatry
22.2%
Anesthesiology
42.4%
Pathology
34.9%
Emergency medicine
49.8%
Terminology
Plaintiffs
Defendants
Bench trial
Jury trial
Deposition
Why serve as an Expert Witness?
Rule #1
– We are doctors
Advantages
– Flexible hours, challenging environment
Disadvantages
– Inflexible hours, hostile environment
What is an expert witness?
Ordinary witness can testify to first hand
experiences related to facts of an event
(what he/she saw, heard, etc.)
Expert witness has education, training,
expertise which can help trier of fact to
understand aspects of case beyond the
knowledge of the average person
Expert may give opinions