Alloimmune Thrombocytopenia
advertisement
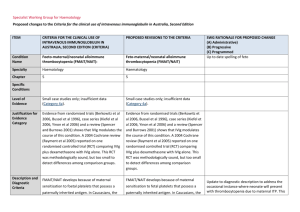
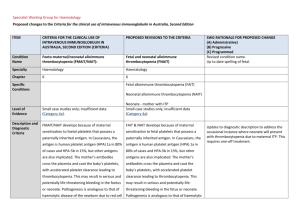
Michael F. McNamara, DO Sanford Maternal Fetal Medicine No disclosures Platelet Disorders in Pregnancy Gestational thrombocytopenia Idiopathic thrombocytopenia (ITP) Thrombotic thrombocytopenia (TTP) Alloimmune thrombocytopenia (NAIT) Gestational Thrombocytopenia Dilution effect Increase of platelet destruction No therapy needed Idiopathic Thrombocytopenia 1-3 / 1000 pregnancies Pregnancy not usually altering disease course Therapy Steroids IVIG Splenectomy Thrombotic Thrombocytopenia Purpura (TTP) TTP/HUS, may be confused with pre eclampsia Microangiopathic hemolytic anemia Thrombocytopenia Neurologic changes (headache, lethargy) Thrombotic occlusions in multiple small vessels Therapy plasma exchange, platelet transfusions Alloimmune Thrombocytopenia Also known as Neonatal Alloimmune Thrombocytopenia (NAIT) 0.2 -1 per 1000 deliveries Low fetal platelets due to maternal antibodies Index case usually affected Antenatal diagnosis often by ultrasound with findings of intracranial hemorrhage Case Study 25 year old female Gravida 5, para 2 Two previous term vaginal deliveries Petechiae, bruising, platelets < 10,000 Counseled on further pregnancies, need of treatment Case Study Presented at 14 weeks gestation Genetic counseling, history reviewed Same paternity as previous infants Father of baby not available for testing (zygosity) Case Study Diagnostic testing (platelet antigen) Maternal Blood HPA 1b/1b Fetal Amniotic fluid HPA 1a/1b Case Study Preventative therapy IVIG 1 gram / kg weekly Prednisone 1mg /kg daily Case Study Antenatal Course Gestational diabetes Severe headaches with IVIG therapy Elevated liver enzymes due to percocet use secondary to headaches Case Study Antenatal steroids at 33 weeks gestation Elected cesarean for delivery with tubal ligation Vaginal delivery if umbilical cord sampling performed with normal fetal platelet count Delivery at 37 weeks, uncomplicated Female infant 5 lbs, 4 oz Alloimmune thrombocytopenia Also know as Neonatal Alloimmune throbocytopenia (NAIT) Incidence 0.2 -1 per 1000 Caucasian births Maternal antigens against fetal platelets NAIT Platelet antigens classified at HPA 1a (PLA1) and HPA 1b (PLA2) 97% adults phenotype HPA 1a (positive for 1a) 69% adults homozygous HPA 1a (1a/1a) 28 % adults heterozygous HPA 1a (1a/1b) 3 % adults homozygous HPA 1b (1b/1b) NAIT Affected pregnancies Most serious complication Intracranial hemorrhage 10-20 % of cases 25-50 % cases diagnosed prenatally Ultrasound findings of intracranial hematoma, porencephalic cysts Antepartum Preventive Therapy Extremely High Risk Previous baby ICH in second trimester High risk Previous baby ICH in third trimester Moderate risk Previous baby with thrombocytopenia but no ICH NAIT Recurrence risk up to 100% Thrombocytopenia is severe and happens earlier in subsequent pregnancies Previous ICH is risk factor for severe thrombocytopenia in next pregnancy Low platelet count goes lower in subsequent pregnancies without treatment in utero NAIT – antenatal therapy IVIG – very uncommon for ICH with IVIG treatment (11/411 for 2.7%) Prednisone (additionally) – no better than IVIG alone Umbilical cord sampling – procedure / bleeding risk Platelet transfusions – unknown efficacy IVIG Mechanism of Action Provision of missing immunoglobulins or neutralizing antibodies, restoration of immune function, and/or suppression of inflammatory and immune-mediated processes Increase the effect of regulatory T cells, contributing to the maintenance of immunologic self-tolerance Prevention of reticuloendothelial uptake of autoantibody-coated blood cells (eg, platelets, red cells) through blockade of macrophage Fc-receptors Case Study #2 Preconception Counseling Gravida 3, Para 3 with recent neonatal demise from ICH delivered at 38 weeks Low platelet count Paternal 1a/1b Maternal 1b/1b Case Study #2 Pregnancy #4, amniocentesis Fetus - male1b/1b, normal pregnancy Pregnancy #5, amniocentesis Fetus – male,1a/1b, affected IVIG, prednisone, cord sampling Cesarean at 37 weeks gestation Case Study #2 First two pregnancies vaginal deliveries with no complications Oldest is a male, second oldest female Recent testing of the female (now an adult), 1b/1b Case Study #2 Platelet antigens classified at HPA 1a (PLA1) and HPA 1b (PLA2) 97% adults phenotype HPA 1a (positive for 1a) 69% adults homozygous HPA 1a (1a/1a) 28 % adults heterozygous HPA 1a (1a/1b) 3 % adults homozygous HPA 1b (1b/1b) 83% chance of having a baby with 1a/1b Summary NAIT cause of neonatal thrombocytopenia Index case possibly severe problems such as ICH Decrease complications with in utero therapy, IVIG, prednisone