Chapter 12: The Central Nervous System
advertisement

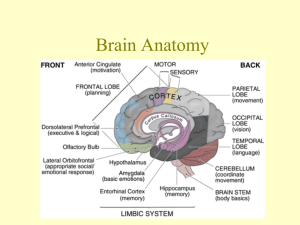
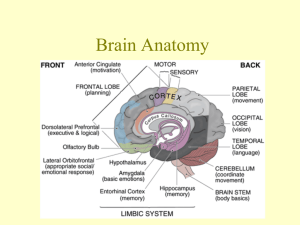
Chapter 12: The Central Nervous System Central Nervous System • Brain and Spinal Cord • Body’s supercomputer • Cephalization – elaboration towards rostal “towards the snout” or anterior portion of CNS • Also increase in the number of neurons Brain • Adult male – 1600 g (3.5 lbs) • Adult female – 1450 g (3.2 lbs) • Brain mass per body mass - equal Embryonic Development 1. 3 week embryo- ectoderm thickens along dorsal midline of body = neural plate 2. Neural tube invaginates – forms groove flanked by neural folds 3. Groove deepens – superior ridges fuse forming neural tube – detached from ectoderm and sinks into a deeper position 4. Neural tube differentiates into CNS – brain anterior and spinal cord - caudal Embryonic Development 5. Neural crest forms – gives rise to some neurons 6. Neural tube – anterior end expands - 3 primary brain vesicles – - 1. prosencephalon – forebrain - 2. mesencephalon – midbrain - 3. rhomben cephalon – hindbrain 7. Week 5 – primary vesicles secondary vesicles - Forebrain telencephalon (endbrain) + diencephalon (hindbrain) - Hindbrain constricts – metencephalon “afterbrain” - Metencephalon – “spinal brain” Embryonic Development 8. 5 – secondary vesicles – develop into major structures of adult brain • 2 cerebral hemispheres – cerebrum – – – – • • • • Diencephalon – hypothalamus Thalamus Epithalamus Retina Mesencephalon = midbrain Metencephalon = pons Myelencephalon = cerebellum Midbrain and hindbrain = spinal cord Surface ectoderm Head Neural plate Tail 1 The neural plate forms from surface ectoderm. Figure 12.1, step 1 Neural folds Neural groove 2 The neural plate invaginates, forming the neural groove, flanked by neural folds. Figure 12.1, step 2 Neural crest 3 Neural fold cells migrate to form the neural crest, which will form much of the PNS and many other structures. Figure 12.1, step 3 Head Surface ectoderm Neural tube Tail 4 The neural groove becomes the neural tube, which will form CNS structures. Figure 12.1, step 4 (a) Neural tube Anterior (rostral) (b) Primary brain vesicles Prosencephalon (forebrain) Mesencephalon (midbrain) Rhombencephalon (hindbrain) Posterior (caudal) Figure 12.2a-b (d) Adult brain structures (e) Adult neural canal regions Telencephalon Cerebrum: cerebral hemispheres (cortex, white matter, basal nuclei) Lateral ventricles Diencephalon Diencephalon (thalamus, hypothalamus, epithalamus), retina Third ventricle Mesencephalon Brain stem: midbrain Cerebral aqueduct Metencephalon Brain stem: pons (c) Secondary brain vesicles Cerebellum Myelencephalon Brain stem: medulla oblongata Spinal cord Fourth ventricle Central canal Figure 12.2c-e Regions of Brain 1. Cerebral Hemispheres 2. Diencephalon 3. Brain stem (pons, midbrain, and medulla) Cortex of gray matter Inner gray matter Central cavity Migratory pattern of neurons Cerebrum Cerebellum Region of cerebellum Outer white matter Gray matter Central cavity Inner gray matter Outer white matter Brain stem Gray matter Central cavity Outer white matter Spinal cord Inner gray matter Figure 12.4 Pattern • Central cavity surrounded by gray matter (neuron cell bodies) • External – white matter (myelinated fiber tracts) • Outer layer of gray matter – cortex – dissapears as you move down the brain stem Ventricles • Arise from expansions of lumen (cavity) of embryonic neural tube • Filled with cerebral spinal fluid • Lined by ependymal cells Lateral ventricle Septum pellucidum Anterior horn Inferior horn Lateral aperture Interventricular foramen Third ventricle Inferior horn Cerebral aqueduct Fourth ventricle Central canal (a) Anterior view (b) Left lateral Posterior horn Median aperture Lateral aperture view Figure 12.5 Lateral Ventricles • Deep in cerebral hemisphere • Large C – shaped chambers separated by septum pellucidum • Communicate with 3rd ventricle – in diencephalon • Channel – intraventricular foramen • 3rd ventricle continuous with 4th – canal cerebral aqueduct • 4th ventricle – 3 openings – 2 lateral apertures and median aperture Lateral ventricle Septum pellucidum Anterior horn Inferior horn Lateral aperture Interventricular foramen Third ventricle Inferior horn Cerebral aqueduct Fourth ventricle Central canal (a) Anterior view (b) Left lateral Posterior horn Median aperture Lateral aperture view Figure 12.5 Cerebral Hemispheres • Superior part of brain • 83 % of brain’s mass • Cover and obscure diencephalon and top of brain stem • Surface – gyri – elevated ridges • Sulci – grooves • Fissures – deeper grooves • Longitudinal fissure – separates cerebral hemispheres • Transverse cerebral fissure – separates cerebral from cerebellum Cerebral Hemisphere • Divided into 5 lobes by sulci • Central sulcus – frontal plane – separates frontal lobe from parietal lobe • Percentral gyrus and postcentral gyrus – border – central sulcus • Occipital lobe – separate from parietal by parietocciplital sulcus • Lateral sulcus – outlines temporal lobe • Insula – 5th lobe – deep in lateral sulcus – forms its floor Precentral gyrus Frontal lobe Central sulcus Postcentral gyrus Parietal lobe Parieto-occipital sulcus (on medial surface of hemisphere) Lateral sulcus Occipital lobe Temporal lobe Transverse cerebral fissure Cerebellum Pons Medulla oblongata Spinal cord Fissure (a deep sulcus) Gyrus Cortex (gray matter) Sulcus White matter (a) Figure 12.6a Frontal lobe Central sulcus Gyri of insula Temporal lobe (pulled down) (b) Figure 12.6b Anterior Longitudinal fissure Frontal lobe Cerebral veins and arteries covered by arachnoid mater Parietal lobe Right cerebral hemisphere Occipital lobe Left cerebral hemisphere (c) Posterior Figure 12.6c Left cerebral hemisphere Brain stem Transverse cerebral fissure Cerebellum (d) Figure 12.6d Brain • • • • Fits snuggly in skull Frontal lobes – lie in anterior cranial fossa Middle cranial fossa – temporal lobe Each hemisphere – 3 regions 1. cerebral cortex – gray 2. internal white matter 3. basal nuclei Cerebral Cortex • “executive suite” of NS conscious mind • Enables awareness of ourselves, our sensations, and enables us to communicate, remember, and understand • Also voluntary movement • Composed of gray matter – neuron cell bodies, dendrites, glial and blood vessels Cerebral Cortex • Billions of neurons – arranged in 6 layers • 2-4 mm thick – 40 % of total brainmass • 52 cortical areas – Broadman areas Cerebral Cortex • 3 functional areas – – 1. motor area – 2. sensory area – 3. association area • All neurons – interneurons • Each hemisphere – sensory and motor functions of opposite sides of body • Hemispheres – not entirely equal in function – Lateralization or specialization of cortical functions • No functional area acts alone • Conscious behavior involves the entire cortex Motor areas Central sulcus Primary motor cortex Premotor cortex Frontal eye field Broca’s area (outlined by dashes) Prefrontal cortex Working memory for spatial tasks Executive area for task management Working memory for object-recall tasks Solving complex, multitask problems (a) Lateral view, left cerebral hemisphere Sensory areas and related association areas Primary somatosensory cortex Somatic Somatosensory sensation association cortex Gustatory cortex (in insula) Taste Wernicke’s area (outlined by dashes) Primary visual cortex Visual association area Auditory association area Primary auditory cortex Vision Hearing Motor association cortex Primary sensory cortex Primary motor cortex Sensory association cortex Multimodal association cortex Figure 12.8a Motor Areas • Control voluntary movement • Posterior part of frontal lobes: primary motor cortex, premotor cortex, Broca’s area, and frontal eye field Motor Area – Primary Motor Cortex • • • • Primary (somatic) motor cortex – Located in precentral gyrus of frontal lobe Large neurons – pyramidal cells Allow control of precise or skilled voluntary movements • Long axons – project into spinal cord – pyramidal tracts • Somatotrophy – control of body structures mapped to places • Muscles controlled by multiple spots Posterior Motor Motor map in precentral gyrus Anterior Toes Jaw Tongue Swallowing Primary motor cortex (precentral gyrus) Figure 12.9 Motor Area – Premotor Cortex • Just anterior to precentral gyrus • Controls learned motor skills of repetitious pattern or nature • Coordinates movements of several muscle groups • Memory bank for skilled motor activites Motor Area – Broca’s Area • Lies anterior to inferior region of premotor area • Considered to be 1. present in one hemisphere only (usually the left) 2. special motor speech area – directs muscles involved in speech production Recently shown to “light up” as we prepare to think or even think about voluntary activities other than speech Motor Area – Frontal Eye Field • Located partial in and anterior to premotor cortex and superior to Broca’s area • Controls voluntary movement of eyes Damage • Damage to areas of primary motor cortex – paralyzes the body muscles controlled by those areas • Voluntary control lost, muscles can still contract reflexively • Premotor cortex - damage results in a loss in motor skills programmed in that region, but muscle strength and ability to perform movements are not Sensory Areas • Occur in parietal lobe, insular, temporal, and occipital lobes 1. Primary Somartosensory Cortex – • In post central gyrus of parietal lobe • Neurons receive info from general (somatic) sensory receptors in the skin and proprioceptors (position sense receptors) in skeletal muscle, joints and tendons • Neurons identify body region being stimulated – spatial discrimination • Right hemisphere – receive input from left side of body • Face & fingertips – most sensitive – largest part Motor areas Central sulcus Primary motor cortex Premotor cortex Frontal eye field Broca’s area (outlined by dashes) Prefrontal cortex Working memory for spatial tasks Executive area for task management Working memory for object-recall tasks Solving complex, multitask problems (a) Lateral view, left cerebral hemisphere Sensory areas and related association areas Primary somatosensory cortex Somatic Somatosensory sensation association cortex Gustatory cortex (in insula) Taste Wernicke’s area (outlined by dashes) Primary visual cortex Visual association area Auditory association area Primary auditory cortex Vision Hearing Motor association cortex Primary sensory cortex Primary motor cortex Sensory association cortex Multimodal association cortex Figure 12.8a Sensory Areas 2. Somatosensory Association Cortex – posterior to primary somatosensory cortex • Integrates sensory inputs – temp, pressure, etc. – relayed to produce understanding of object being felt – size, texture, relationship Posterior Sensory Anterior Sensory map in postcentral gyrus Genitals Primary somatosensory cortex (postcentral gyrus) Intraabdominal Figure 12.9 Sensory Areas 3. Visual Areas – primary visual (striate) cortex • Extreme posterior tip of occipital lobe • Most buried deep in calcarine sulcus • Largest • Receives visual input from retina • Visual association areas – surround primary – uses past visual experiences to interpret stimuli Sensory Areas 4. Auditory Areas – primary auditory cortex – superior margin of temporal lobe • Impulses from ear transmitted here – interpreted as pitch, loudness, location, etc. • Auditory Association area – permits perception of sound • Memories of past sounds Sensory Areas 5. Olfactory cortex – • Medial aspect of temporal lobes • Small region – piriform lobe • Smell receptors send impulses Sensory Areas 6. Gustatory Cortex – taste stimuli • Insula just deep to temporal lobe Sensory Areas 7. Visceral Sensory Area – conscious perception of visceral stimulation • Upset stomach, full bladder, lung bursting – holding breath to long Sensory Areas 8. Vestibular (equilibrium) cortex – difficult to find • Imaging – shows it in the posterior part of insula and adjacent parietal cortex Posterior Sensory Anterior Sensory map in postcentral gyrus Genitals Primary somatosensory cortex (postcentral gyrus) Intraabdominal Figure 12.9 Multimodal Association Areas • Cortex – complex • Input from multiple senses and outputs to multiple areas • Meaning to info we receive, stores memories, ties to previous experiences, and decide actions • Sensations, thoughts, and emotions Multimodal Association Areas 1. Anterior Association Areas – frontal lobe – prefrontal cortex • Most complicated • Intellect, complex learning abilities (cognition), recall, and personality • Working memory – abstract ideas, judgment, reasoning, persistence, and planning • Abilities develop slowly in children – region of the brain that matures slowly Multimodal Association Areas 2. Posterior Association areas – large region encompassing part of temporal, parietal, and occipital lobes • Recognizes patterns and faces Multimodal Association Areas 3. Limbic Association Areas – cingulate gyrus • Parahippocampal gyrus • Hippocampus • Part of limbic system • Emotional impact • Sense of danger Lateralization of Cortical Functioning • Division of labor • Each hemisphere has unique abilities not shared by its partner – lateralization • Cerebral dominance – designates hemisphere – dominant for language • Left hemisphere – 90 % - language, math, and logic • Right – more free spirited – visual-spatial skills, intuition, emotion, artistic and musical skills • Remaining 10 % of people – roles reversed • Typically – male and left handed Cerebral White Matter • White matter – deep to cortical gray matter – responsible for communication between cerebral area and cerebral cortex and lower CNS centers • Consists of – myelinated fibers classified according to the direction they run – 1. Commissural fibers – connect gray area of 2 hemispheres 2. Association fibers – connect different parts of same hemisphere 3. Projection fibers – cortex to rest of NS Longitudinal fissure Lateral ventricle Superior Commissural fibers (corpus callosum) Association fibers Basal nuclei • Caudate • Putamen • Globus pallidus Corona radiata Thalamus Internal capsule Fornix Gray matter Third ventricle White matter Pons Projection fibers Medulla oblongata (a) Decussation of pyramids Figure 12.10a Cerebral White Matter • • • • • Basal nuclei - Subcortical nuclei Deep within cerebral white matter Input from entire cerebral cortex Functions overlap with those of cerebellum Part in regulating attention and cognition Fibers of corona radiata Caudate nucleus Lentiform Corpus nucleus striatum • Putamen • Globus pallidus (deep to putamen) Projection fibers run deep to lentiform nucleus (a) Thalamus Tail of caudate nucleus Figure 12.11a Diencephalon • Central core of forebrain • Surrounded by cerebral hemispheres • 3 parts – thalamus, hypothalamus, and epithalamus Cerebral hemisphere Septum pellucidum Interthalamic adhesion (intermediate mass of thalamus) Interventricular foramen Anterior commissure Hypothalamus Optic chiasma Pituitary gland Mammillary body Pons Medulla oblongata Corpus callosum Fornix Choroid plexus Thalamus (encloses third ventricle) Posterior commissure Pineal gland (part of epithalamus) Corpora quadrigemina MidCerebral brain aqueduct Arbor vitae (of cerebellum) Fourth ventricle Choroid plexus Cerebellum Spinal cord Figure 12.12 Diencephalon - Thalamus • • • • • Bilateral egg shaped nuclei Superolateral walls of 3rd ventricle 80 % of diencephalon Relay station for info Nuclei – each functional specialty receives from a specific area • Info sorted and edited Diencephalon - Hypothalamus • Below thalamus • Caps brain stem and forms infolateral walls of 3rd ventricle • Extends from optic chiasma to mammillary bodies • Infundibulum – stalk of hypothalamic tissue connects pituitary • Main visceral controlling center of body Diencephalon - Hypothalamus • Homeostatic roles – 1. Autonomic Control Center – influences BP, rate and force of heart beat, digestive tract motility, pupil size, etc. 2. Emotional response – perception of pleasure, fear, and rage, biological rhythms and drives 3. Body temperature – monitor blood temperature and other thermoreceptors 4. Food Intake – hunger and satiety in response to changing blood levels 5. Water balance and thirst – osmoreceptors, ADH 6. Sleep – wake Cycles 7. Endocrine System functioning – releasing and inhibiting hormones Diencephalon - Hypothalamus • Number of Disorders – • Obesity, sleep disturbances, dehydration, emotional impulses • Infant failure to thrive – delay child’s growth or development when deprived of a warm, nurturing relationship Diencephalon - Epithalamus • Most dorsal • Roof of 3rd ventricle • Pineal gland – secrets hormone melanin – sleep signal and antioxidant Cerebral hemisphere Septum pellucidum Interthalamic adhesion (intermediate mass of thalamus) Interventricular foramen Anterior commissure Hypothalamus Optic chiasma Pituitary gland Mammillary body Pons Medulla oblongata Corpus callosum Fornix Choroid plexus Thalamus (encloses third ventricle) Posterior commissure Pineal gland (part of epithalamus) Corpora quadrigemina MidCerebral brain aqueduct Arbor vitae (of cerebellum) Fourth ventricle Choroid plexus Cerebellum Spinal cord Figure 12.12 Brain Stem • • • • • • Midbrain, pons, medulla oblongata 2.5 % of total brain mass Deep gray matter surrounded by white fibers Automatic behaviors Pathway Innervation of head Midbrain • • • • 2 cerebral peduncles – “little feet” Cruscerbui – “leg” Fight or flight Reflexive responses – startle response View (a) Optic chiasma Optic nerve (II) Crus cerebri of cerebral peduncles (midbrain) Diencephalon • Thalamus • Hypothalamus Mammillary body Thalamus Hypothalamus Diencephalon Midbrain Oculomotor nerve (III) Trochlear nerve (IV) Pons Brainstem Medulla oblongata Trigeminal nerve (V) Pons Facial nerve (VII) Middle cerebellar peduncle Abducens nerve (VI) Vestibulocochlear nerve (VIII) Pyramid Glossopharyngeal nerve (IX) Hypoglossal nerve (XII) Vagus nerve (X) Ventral root of first cervical nerve Decussation of pyramids Accessory nerve (XI) Spinal cord (a) Ventral view Figure 12.15a Pons • • • • • Bulging brainstem region Conduction tracts Deep fibers – longitudinal Superficial – transverse and dorsal Cranial nerves Crus cerebri of cerebral peduncles (midbrain) Thalamus View (b) Infundibulum Pituitary gland Superior colliculus Inferior colliculus Trochlear nerve (IV) Trigeminal nerve (V) Pons Superior cerebellar peduncle Middle cerebellar peduncle Facial nerve (VII) Abducens nerve (VI) Glossopharyngeal nerve (IX) Hypoglossal nerve (XII) Inferior cerebellar peduncle Vestibulocochlear nerve (VIII) Olive Thalamus Vagus nerve (X) Hypothalamus Diencephalon Midbrain Accessory nerve (XI) Pons Brainstem Medulla oblongata (b) Left lateral view Figure 12.15b Medulla Oblongata • Medulla • Inferior part of brain stem • Visceral motor nuclei – Cardio center – adjusts heart rate • Vasomotor center – changes blood vessel diameter – Respiratory = respiratory rhythm – Various others – vomiting, coughing, swallowing, hiccupping , and sneezing Thalamus View (c) Diencephalon Pineal gland Anterior wall of fourth ventricle Choroid plexus (fourth ventricle) Dorsal median sulcus Dorsal root of first cervical nerve Midbrain • Superior Corpora colliculus quadrigemina • Inferior of tectum colliculus • Trochlear nerve (IV) • Superior cerebellar peduncle Pons • Middle cerebellar peduncle Medulla oblongata • Inferior cerebellar peduncle • Facial nerve (VII) • Vestibulocochlear nerve (VIII) • Glossopharyngeal nerve (IX) • Vagus nerve (X) • Accessory nerve (XI) Thalamus Hypothalamus Midbrain Pons (c) Dorsal view Diencephalon Brainstem Medulla oblongata Figure 12.15c Cerebellum • • • • Cauliflower like 11 % of total brain mass Under occipital lobes Input from – cerebral motor cortex, brain stem, and sensory receptors • Coordinated movement – driving, typing, etc Anterior lobe Cerebellar cortex Arbor vitae Cerebellar peduncles • Superior • Middle • Inferior Medulla oblongata (b) Flocculonodular lobe Posterior lobe Choroid plexus of fourth ventricle Figure 12.17b Cerebellum • • • • • Anatomy – bilateral symmetry 2 apple sized hemispheres Fola – pleat-like gyri Deep fissures Outer cortex – gray matter and deeply situated paired mass of gray matter • Neurons – Purkinje cells Cerebellum • Cerebellar Processing – functional scheme 1. Cerebral cortex motor areas notify cerebellum of intent to initiate voluntary muscle control 2. Receives info from proprioceptors throughout the body – body position and momentum 3. Cerebellar cortex – calculated best way to coordinate force, direction, and extent 4. Superior peduncles – dispatches “blue print” for coordinated movement Functional Brain Systems • Network of neurons that work together but span large distances in brain • Cannot be localized to specific regions Limbic System • Group of structures located in medial aspect of each cerebral hemisphere and diencephalon • Cerebral structures that encircle upper part of brain stem • Emotional or affective (feelings) brain • Odors – trigger emotional reactions – rhinencephalon – “smell brain” • Interacts with prefrontal lobes – intimate relationship between feelings and thoughts Reticular Formation • Extends central core of medulla oblongata, pons, and midbrain • Loosely clustered neurons 1. 2. 3. - - Midline raphe neuclei Medial (large cell) group Lateral (small cell) group flung axonal connections Reticular activating system (RAS) – impulses from great ascending sensory tracts – keep them active and enhance effect on cerebrum Filter sensory inputs Inhibited sleep centers Depressed by alcohol, sleep aid drugs, and tranquilizers Higher Mental Functions • Brainwaves reflect the electrical activity of higher mental functions • Electroencephalogram – record some aspects of activity • Electrodes on scalp measure potential energy differences • Brainwaves – generated by synaptic activity at surface of cortex (a) Scalp electrodes are used to record brain wave activity (EEG). Figure 12.20a Brain Waves • –4 categories 1. Alpha Waves – 8-13 Hz - Regular rhythmic - Low amplitude - Synchronous waves - Brain – ‘idling’ – calm, relaxed state of wakefulness Brain Waves 2. Beta Waves – 14-30Hz – rhythmic, but not as regular, occur when mentally alert 3. Theta Waves – 4-7 Hz – irregular, common in children, uncommon in adults 4. Delta Waves – 4 Hz or less – high amplitude waves, deep sleep – reticular activating system is damped – anesthesia - Indicated brain damage in awake adults Brain Waves • Change with age, sensory stimuli, brain disease and chemical state of body • Flat EEG – clinical evidence of brain death • Epilepsy – seizures – torrent of electrical charges of groups of brain neurons • Uncontrolled activity – no other messages can get through 1-second interval Alpha waves—awake but relaxed Beta waves—awake, alert Theta waves—common in children Delta waves—deep sleep (b) Brain waves shown in EEGs fall into four general classes. Figure 12.20b Consciousness • Encompass conscious perception of sensations, voluntary initiation and control of movements and capabilities associated with higher mental functioning • Defined by behavior in response to stimuli – Alertness – Drowsiness or lethargy – Stupor – coma Consciousness • Difficult to determine • Current suppositions – 1. Simultaneous activity of large areas of cerebral cortex 2. It is superimposed on other types of neural activity 3. Is it holistic and totally interconnected Consciousness • Fainting or Syncope – brief loss of consciousness • Most often from inadequate cerebral blood flow due to low BP • Coma – total unresponsiveness • Not deep sleep – oxygen level lower than deep sleep • Blows to head – widespread cerebral or brain stem trauma • Tumors or infections, hypoglycemia, drug overdose, kidney failure • Brain Death – irreparable damage to brain Sleep and Sleep Wake Cycles • Sleep – state of partial unconsciousness from which a person can be aroused by stimulation • Coma – cannot be aroused Types of Sleep • 2 major types that alternate throughout the sleep cycle 1. Non-rapid eye movement (NREM) 2. Rapid Eye movement (REM) - Defined by EEG patterns Sleep • • • • 1st 30 -45 minutes – 2 stages of NREM Then stage 3 and 4 – NREM- slow wave sleep Deeper sleep – EEG wave declines – amplitude increase 90 minutes – NREM stage 4 – changes rapidly – appears to backtrack until alpha waves appear – onset of REM sleep – – – – – – Increase in heart rate Increase respiratory rate Increase in blood pressure Decrease in gastrointestinal activity Increase in oxygen use Eyes move rapidly, skeletal muscles limp, dreams Awake REM: Skeletal muscles (except ocular muscles and diaphragm) are actively inhibited; most dreaming occurs. NREM stage 1: Relaxation begins; EEG shows alpha waves, arousal is easy. NREM stage 2: Irregular EEG with sleep spindles (short high- amplitude bursts); arousal is more difficult. NREM stage 3: Sleep deepens; theta and delta waves appear; vital signs decline. (a) Typical EEG patterns NREM stage 4: EEG is dominated by delta waves; arousal is difficult; bed-wetting, night terrors, and sleepwalking may occur. Figure 12.21a Sleep Patterns • • • • Alternating patterns of sleep and wakefulness Natural circadian, or 24 hour, rhythm Hypothalamus response Suprachaismatic nucleus – biological clock regulates preoptic nucleus – sleep inducing center Sleep Patterns • Young/middle aged adult – 4 stages of NREM then alternate with occasional partial analysis • REM ~ every 90 minutes • 1st REM – 5-10 minutes long • Final REM – 20 -50 minutes long • Wake – hypothermic neurons release peptides (exins) “wakeup” chemical Awake REM Stage 1 Stage 2 Non REM Stage 3 Stage 4 Time (hrs) (b) Typical progression of an adult through one night’s sleep stages Figure 12.21b Importance of Sleep • Slow wave sleep – restorative – neural activity winds down • REM – deprived – moody and depressed – Analyze days events – Get rid of meaning less communication • Alcohol and sleep meds – suppress REM but not slow wave sleep • Tranquilizers – suppress slow wave more than REM Importance of Sleep • Requirements – infant – 16 hrs • 7 ½ 8 ½ - early adulthood • REM – ½ sleep time in infants – declines until 10 years old • Stabilizes ~ 25% • Stage 4 – declines steadily – often disappears by age 60 Sleep • Narcolepsy – lapse into REM from an awake state • Lasts ~ 15 min, can occur at any time, most often triggered by a pleasurable event – Fewer cells in hypothalamus that secrete orexins • Insomnia – inability to obtain amount or quantity of sleep needed to adequately function – Varies – 4 -9 hrs/day • Sleep Apnea – temporary cessation of breathing during sleep – – – – Victim wakes due to hypoxia Associated with obesity Made worse by alcohol Must wear a mask when sleeping Language • Involves almost all of association cortex on left side • 2 important areas – 1. Broca’s area – can’t speak, but can understand 2. Wericke’s area – can speak but can’t understand - Areas work together to form a single implementation system Memory • Storage and retrieval of information essential for learning and incorporating experiences • Stages 1. Short term Memory (STM) – working memory - Limited to 7 or 8 chunks of information 2. Long term Memory (LTM) – limitless capacity - Can be forgotten - Memory bank changes with time - Ability to store and retrieve information declines with age From STM to LTM 1. Emotional state – we learn when surprised, alert, motivated, or aroused - Norephinephrine released when excited 2. Rehearsal – repetition – enhances memory 3. Association – tying new info to old info already stored 4. Automatic Memory – not all impressions are consciously formed - Memory consolidation – fitting new facts into knowledge already stored Outside stimuli General and special sensory receptors Afferent inputs Temporary storage (buffer) in cerebral cortex Automatic memory Data permanently lost Data selected for transfer Short-term memory (STM) Forget Forget Data transfer influenced by: Retrieval Excitement Rehearsal Association of old and new data Long-term memory (LTM) Data unretrievable Figure 12.22 Categories of Memory • Declarative (fact) memory – learning explicit info – names, faces, dates • Non-declarative memory – less conscious • Procedural (skills) memory – ex. Playing the piano • Motor Memory – riding a bike • Emotional memory – pounding heart when see a rattlesnake Brain Structures • Visual memories – stored in occipital cortex • Music – temporal cortex • Damage to hippocampus and medial temporal lobe result in slight memory loss • Bilateral destruction - amnesia Protection of Brain • Nervous tissue – soft and delicate • Brain – protected by bone, membranes, and CSF • Harmful substances – blood-brain barrier Superior sagittal sinus Subdural space Subarachnoid space Skin of scalp Periosteum Bone of skull Periosteal Dura Meningeal mater Arachnoid mater Pia mater Arachnoid villus Blood vessel Falx cerebri (in longitudinal fissure only) Figure 12.24 Meninges • 3 connective tissue membranes that lie external to CNS organs • Functions: – Cover and protect CNS – Protect blood vessels and enclose venous sinuses – Contain cerebral spinal fluid – Form partitions in skull Meninges • • • • • Dura Matter “tough mother’ Strongest meninx Surround brain – 2 layered sheet of fibrous CT Dura septa –dura matter extends into brain, limit excessive movement of brain • Arachnoid Matter • Middle meninx • Loose brain covering Superior sagittal sinus Subdural space Subarachnoid space Skin of scalp Periosteum Bone of skull Periosteal Dura Meningeal mater Arachnoid mater Pia mater Arachnoid villus Blood vessel Falx cerebri (in longitudinal fissure only) Figure 12.24 Superior sagittal sinus Straight sinus Crista galli of the ethmoid bone Pituitary gland Falx cerebri Tentorium cerebelli Falx cerebelli (a) Dural septa Figure 12.25a Meninges • Pia Mater – “gentle matter” • Delicate connective tissue • Clings to brain • Meningitis – inflammation of meninges • Serious threat – can spread to CNS • Encephalitis – brain inflammation Cerebrospinal Fluid • • • • • CSF – found in and around the brain Liquid cushion Prevents brain from crushing itself Protects against trauma Watery “broth” similar to blood plasma – less proteins and plasma • CSF contains more Na, Cl, and H, and less Ca and K Superior sagittal sinus 4 Choroid plexus Arachnoid villus Interventricular foramen Subarachnoid space Arachnoid mater Meningeal dura mater Periosteal dura mater 1 Right lateral ventricle (deep to cut) Choroid plexus of fourth ventricle 3 Third ventricle 1 CSF is produced by the Cerebral aqueduct Lateral aperture Fourth ventricle Median aperture Central canal of spinal cord (a) CSF circulation 2 choroid plexus of each ventricle. 2 CSF flows through the ventricles and into the subarachnoid space via the median and lateral apertures. Some CSF flows through the central canal of the spinal cord. 3 CSF flows through the subarachnoid space. 4 CSF is absorbed into the dural venous sinuses via the arachnoid villi. Figure 12.26a Blood Brain Barrier • Protective mechanism that helps maintain a stable environment for brain • If brain exposed to chemical variations in blood – neurons would fire uncontrollably • Blood born substances must pass through 3 layers before they reach neurons – 1. epithelium of capillary walls 2. relatively thick basal lamina surrounding capillaries 3. bulbous “feet” of astrocytes clinging to capillaries - Barrier is selective – nutrients pass, wastes can not Capillary Neuron Astrocyte (a) Astrocytes are the most abundant CNS neuroglia. Figure 11.3a Homeostatic Imbalances of the Brain • Traumatic brain injuries – Concussion—temporary alteration in function – Contusion—permanent damage – Subdural or subarachnoid hemorrhage—may force brain stem through the foramen magnum, resulting in death – Cerebral edema—swelling of the brain associated with traumatic head injury Homeostatic Imbalances of the Brain • Cerebrovascular accidents (CVAs)(strokes) – Blood circulation is blocked and brain tissue dies, e.g., blockage of a cerebral artery by a blood clot – Typically leads to hemiplegia, or sensory and speed deficits – Transient ischemic attacks (TIAs)—temporary episodes of reversible cerebral ischemia – Tissue plasminogen activator (TPA) is the only approved treatment for stroke Homeostatic Imbalances of the Brain • Degenerative brain disorders – Alzheimer’s disease (AD): a progressive degenerative disease of the brain that results in dementia – Parkinson’s disease: degeneration of the dopaminereleasing neurons of the substantia nigra – Huntington’s disease: a fatal hereditary disorder caused by accumulation of the protein huntingtin that leads to degeneration of the basal nuclei and cerebral cortex The Spinal Cord: Embryonic Development • By week 6, there are two clusters of neuroblasts – Alar plate—will become interneurons; axons form white matter of cord – Basal plate—will become motor neurons; axons will grow to effectors • Neural crest cells form the dorsal root ganglia sensory neurons; axons grow into the dorsal aspect of the cord Dorsal root ganglion: sensory neurons from neural crest Alar plate: interneurons White matter Basal plate: motor neurons Neural tube cells Central cavity Figure 12.28 Spinal Cord • Location – Begins at the foramen magnum – Ends as conus medullaris at L1 vertebra • Functions – Provides two-way communication to and from the brain – Contains spinal reflex centers Spinal Cord: Protection • Bone, meninges, and CSF • Cushion of fat and a network of veins in the epidural space between the vertebrae and spinal dura mater • CSF in subarachnoid space Spinal Cord: Protection • Denticulate ligaments: extensions of pia mater that secure cord to dura mater • Filum terminale: fibrous extension from conus medullaris; anchors the spinal cord to the coccyx T12 Ligamentum flavum Lumbar puncture needle entering subarachnoid space L5 L4 Supraspinous ligament L5 Filum terminale S1 Intervertebral disc Arachnoid matter Dura mater Cauda equina in subarachnoid space Figure 12.30 Cervical enlargement Dura and arachnoid mater Lumbar enlargement Conus medullaris Cauda equina Filum terminale (a) The spinal cord and its nerve roots, with the bony vertebral arches removed. The dura mater and arachnoid mater are cut open and reflected laterally. Cervical spinal nerves Thoracic spinal nerves Lumbar spinal nerves Sacral spinal nerves Figure 12.29a Spinal Cord • Spinal nerves – 31 pairs • Cervical and lumbar enlargements – The nerves serving the upper and lower limbs emerge here • Cauda equina – The collection of nerve roots at the inferior end of the vertebral canal Cross-Sectional Anatomy • Two lengthwise grooves divide cord into right and left halves – Ventral (anterior) median fissure – Dorsal (posterior) median sulcus • Gray commissure—connects masses of gray matter; encloses central canal Epidural space (contains fat) Subdural space Subarachnoid space (contains CSF) Pia mater Arachnoid mater Dura mater Spinal meninges Bone of vertebra Dorsal root ganglion Body of vertebra (a) Cross section of spinal cord and vertebra Figure 12.31a Dorsal median sulcus Dorsal funiculus White Ventral funiculus columns Lateral funiculus Dorsal root ganglion Gray commissure Dorsal horn Gray Ventral horn matter Lateral horn Spinal nerve Dorsal root (fans out into dorsal rootlets) Ventral root (derived from several ventral rootlets) Central canal Ventral median fissure Pia mater Arachnoid mater Spinal dura mater (b) The spinal cord and its meningeal coverings Figure 12.31b Gray Matter • Dorsal horns—interneurons that receive somatic and visceral sensory input • Ventral horns—somatic motor neurons whose axons exit the cord via ventral roots • Lateral horns (only in thoracic and lumbar regions) –sympathetic neurons • Dorsal root (spinal) gangia—contain cell bodies of sensory neurons Dorsal root (sensory) Dorsal root ganglion Dorsal horn (interneurons) Somatic sensory neuron Visceral sensory neuron Visceral motor neuron Somatic motor neuron Spinal nerve Ventral root (motor) Ventral horn (motor neurons) Interneurons receiving input from somatic sensory neurons Interneurons receiving input from visceral sensory neurons Visceral motor (autonomic) neurons Somatic motor neurons Figure 12.32 White Matter • Consists mostly of ascending (sensory) and descending (motor) tracts • Transverse tracts (commissural fibers) cross from one side to the other • Tracts are located in three white columns (funiculi on each side—dorsal (posterior), lateral, and ventral (anterior) • Each spinal tract is composed of axons with similar functions Pathway Generalizations • Pathways decussate (cross over) • Most consist of two or three neurons (a relay) • Most exhibit somatotopy (precise spatial relationships) • Pathways are paired symmetrically (one on each side of the spinal cord or brain) Ascending tracts Fasciculus gracilis Dorsal white Fasciculus cuneatus column Dorsal spinocerebellar tract Ventral spinocerebellar tract Lateral spinothalamic tract Ventral spinothalamic tract Descending tracts Ventral white commissure Lateral reticulospinal tract Lateral corticospinal tract Rubrospinal tract Medial reticulospinal tract Ventral corticospinal tract Vestibulospinal tract Tectospinal tract Figure 12.33 Ascending Pathways • Consist of three neurons • First-order neuron – Conducts impulses from cutaneous receptors and proprioceptors – Branches diffusely as it enters the spinal cord or medulla – Synapses with second-order neuron Ascending Pathways • Second-order neuron – Interneuron – Cell body in dorsal horn of spinal cord or medullary nuclei – Axons extend to thalamus or cerebellum Ascending Pathways • Third-order neuron – Interneuron – Cell body in thalamus – Axon extends to somatosensory cortex Ascending Pathways • Two pathways transmit somatosensory information to the sensory cortex via the thalamus – Dorsal column-medial lemniscal pathways – Spinothalamic pathways • Spinocerebellar tracts terminate in the cerebellum Dorsal Column-Medial Lemniscal Pathways • Transmit input to the somatosensory cortex for discriminative touch and vibrations • Composed of the paired fasciculus cuneatus and fasciculus gracilis in the spinal cord and the medial lemniscus in the brain (medulla to thalamus) Dorsal spinocerebellar tract (axons of second-order neurons) Medial lemniscus (tract) (axons of second-order neurons) Nucleus gracilis Nucleus cuneatus Medulla oblongata Fasciculus cuneatus (axon of first-order sensory neuron) Axon of first-order neuron Muscle spindle (proprioceptor) (a) Spinocerebellar pathway Joint stretch receptor (proprioceptor) Cervical spinal cord Fasciculus gracilis (axon of first-order sensory neuron) Lumbar spinal cord Dorsal column–medial lemniscal pathway Touch receptor Figure 12.34a (2 of 2) Primary somatosensory cortex Axons of third-order neurons Thalamus Cerebrum Midbrain Cerebellum Pons (a) Spinocerebellar pathway Dorsal column–medial lemniscal pathway Figure 12.34a (1 of 2) Anterolateral Pathways • Lateral and ventral spinothalamic tracts • Transmit pain, temperature, and coarse touch impulses within the lateral spinothalamic tract Lateral spinothalamic tract (axons of second-order neurons) Medulla oblongata Pain receptors Cervical spinal cord Lumbar spinal cord Axons of first-order neurons Temperature receptors (b) Spinothalamic pathway Figure 12.34b (2 of 2) Primary somatosensory cortex Axons of third-order neurons Thalamus Cerebrum Midbrain Cerebellum Pons (b) Spinothalamic pathway Figure 12.34b (1 of 2) Spinocerebellar Tracts • Ventral and dorsal tracts • Convey information about muscle or tendon stretch to the cerebellum Dorsal spinocerebellar tract (axons of second-order neurons) Medial lemniscus (tract) (axons of second-order neurons) Nucleus gracilis Nucleus cuneatus Medulla oblongata Fasciculus cuneatus (axon of first-order sensory neuron) Axon of first-order neuron Muscle spindle (proprioceptor) (a) Spinocerebellar pathway Joint stretch receptor (proprioceptor) Cervical spinal cord Fasciculus gracilis (axon of first-order sensory neuron) Lumbar spinal cord Dorsal column–medial lemniscal pathway Touch receptor Figure 12.34a (2 of 2) Primary somatosensory cortex Axons of third-order neurons Thalamus Cerebrum Midbrain Cerebellum Pons (a) Spinocerebellar pathway Dorsal column–medial lemniscal pathway Figure 12.34a (1 of 2) Descending Pathways and Tracts • Deliver efferent impulses from the brain to the spinal cord – Direct pathways—pyramidal tracts – Indirect pathways—all others Descending Pathways and Tracts • Involve two neurons: 1. Upper motor neurons • Pyramidal cells in primary motor cortex 2. Lower motor neurons • • Ventral horn motor neurons Innervate skeletal muscles The Direct (Pyramidal) System • Impulses from pyramidal neurons in the precentral gyri pass through the pyramidal (corticospinal)l tracts • Axons synapse with interneurons or ventral horn motor neurons • The direct pathway regulates fast and fine (skilled) movements Pyramidal cells (upper motor neurons) Primary motor cortex Internal capsule Cerebrum Midbrain Cerebral peduncle Cerebellum Pons (a) Pyramidal (lateral and ventral corticospinal) pathways Figure 12.35a (1 of 2) Ventral corticospinal tract Pyramids Decussation of pyramid Lateral corticospinal tract Medulla oblongata Cervical spinal cord Skeletal muscle Lumbar spinal cord Somatic motor neurons (lower motor neurons) (a) Pyramidal (lateral and ventral corticospinal) pathways Figure 12.35a (2 of 2) Indirect (Extrapyramidal) System • Includes the brain stem motor nuclei, and all motor pathways except pyramidal pathways • Also called the multineuronal pathways Indirect (Extrapyramidal) System • These pathways are complex and multisynaptic, and regulate: – Axial muscles that maintain balance and posture – Muscles controlling coarse movements – Head, neck, and eye movements that follow objects Indirect (Extrapyramidal) System • Reticulospinal and vestibulospinal tracts— maintain balance • Rubrospinal tracts—control flexor muscles • Superior colliculi and tectospinal tracts mediate head movements in response to visual stimuli Cerebrum Red nucleus Midbrain Cerebellum Pons (b) Rubrospinal tract Figure 12.35b (1 of 2) Rubrospinal tract Medulla oblongata Cervical spinal cord (b) Rubrospinal tract Figure 12.35b (2 of 2) Spinal Cord Trauma • Functional losses – Parasthesias • Sensory loss – Paralysis • Loss of motor function Spinal Cord Trauma • Flaccid paralysis—severe damage to the ventral root or ventral horn cells – Impulses do not reach muscles; there is no voluntary or involuntary control of muscles – Muscles atrophy Spinal Cord Trauma • Spastic paralysis—damage to upper motor neurons of the primary motor cortex – Spinal neurons remain intact; muscles are stimulated by reflex activity – No voluntary control of muscles Spinal Cord Trauma • Transection – Cross sectioning of the spinal cord at any level – Results in total motor and sensory loss in regions inferior to the cut – Paraplegia—transection between T1 and L1 – Quadriplegia—transection in the cervical region Poliomyelitis • Destruction of the ventral horn motor neurons by the poliovirus • Muscles atrophy • Death may occur due to paralysis of respiratory muscles or cardiac arrest • Survivors often develop postpolio syndrome many years later, as neurons are lost Amyotrophic Lateral Sclerosis (ALS) • Also called Lou Gehrig’s disease • Involves progressive destruction of ventral horn motor neurons and fibers of the pyramidal tract • Symptoms—loss of the ability to speak, swallow, and breathe • Death typically occurs within five years • Linked to glutamate excitotoxicity, attack by the immune system, or both Developmental Aspects of the CNS • CNS is established during the first month of development • Gender-specific areas appear in both brain and spinal cord, depending on presence or absence of fetal testosterone • Maternal exposure to radiation, drugs (e.g., alcohol and opiates), or infection can harm the developing CNS • Smoking decreases oxygen in the blood, which can lead to neuron death and fetal brain damage Developmental Aspects of the CNS • The hypothalamus is one of the last areas of the CNS to develop • Visual cortex develops slowly over the first 11 weeks • Neuromuscular coordination progresses in superior-to-inferior and proximal-to-distal directions along with myelination Developmental Aspects of the CNS • Age brings some cognitive declines, but these are not significant in healthy individuals until they reach their 80s • Shrinkage of brain accelerates in old age • Excessive use of alcohol causes signs of senility unrelated to the aging process