patients
advertisement
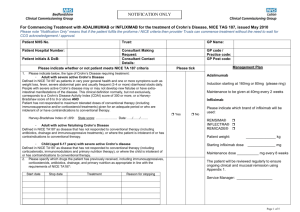
Controversies and challenges in the clinical care of patients with IBD: You can’t always get what you want! Stephen B. Hanauer, MD University of Chicago Medicine Conflicts of Interest Abbott Janssen UCB Prometheus What I want for Hanukkah/Christmas Cost-effective therapeutic drug monitoring for biologics Ability to dose-adjust biologics A reliable surrogate for mucosal healing Therapeutic Drug Monitoring Clinical Gastroenterology and Hepatology Volume 10, Issue 10 , Pages 1079-1087, October 2012 Therapeutic Drug Monitoring of Tumor Necrosis Factor Antagonists in Inflammatory Bowel Disease Ingrid Ordás, Brian G. Feagan, William J. Sandborn 50.0 10.0 5.0 1.0 Adalimumab 160 mg (day 1), 80 mg (day 8) and 40 mg ev ery tw o w eek s Adalimumab 40 mg ev ery tw o w eek s 0.5 Simulated anti-TNF biologic conc Inflix imab 5 mg/k g at day 1, day 15, day 43 and ev ery 8 w eek s Inflix imab 3 mg/k g at day 1, day 15, day 43 and ev ery 8 w eek s 0 20 40 60 Time (day s ) 80 100 120 Effects of absent blood levels Disease recurs (or no primary response) Development of antibodies (immunogenicity) Secondary loss of response Factors Affecting the Pharmacokinetics of Monoclonal Antibodies IMPACT on PK Presence of ADAs Decreases serum [mAbs] Three fold-increased clearance Worse clinical outcomes Concomitant use of IS Reduces formation Increases serum [mAbs] Decreases mAbs clearance Better clinical outcomes High Baseline [TNF-α] May decrease [mAbs] by increasing clearance Low Albumin High Baseline CRP Body size Gender Increases clearance Worse clinical outcomes Increases clearance High BMI may increase clearance Males have higher clearance Ordas I, Feagan B, Mould D, Sandborn WJ. Clin Pharmacol Ther 2012 Effect of Trough Serum Infliximab Concentrations on Clinical Outcome at >52 Weeks Trough serum infliximab Detectable 100 Undetectable Patients with endoscopic improvement >75% (%) Patients in remission (%) 100 82 88 p<0.001 33 p<0.001 6 0 100 0 Patients with CRP <5 mg/dL (%) 76 100 Patients with complete endoscopic remission (%) p<0.001 47 32 p=0.03 19 0 Maser et al. Clin Gastroenterol Hepatol. 2006; 4:1248-54 0 Lower Adalimumab Trough Levels Results in a Lower Rate of Sustained Clinical Response Karmaris Gastro 2009;137:1628–1640 100 90 80 70 60 50 40 30 20 10 0 P< 0.001 Endoscopic Improvement (% of patients) Remissison (% of patients) Clinical outcomes in UC patients treated with infliximab correlate with detectable trough levels 69 15 Detectable Colectomy (% of patients) (% of patients) Undetectable P< 0.001 100 90 76 80 70 60 50 40 28 30 20 10 0 Undetectable P< 0.001 100 90 80 70 60 55 50 40 30 20 7 10 0 Undetectable Seow C H et al. Gut 2010;59:49-54 Detectable Detectable ACT 1+2: Proportion of Patients with Ulcerative Colitis Treated with Infliximab Achieving Clinical Remission by Serum Infliximab Concentration IFX Conc. (% patients) Week 8 Week 30 Week 54 1st Quartile 2nd Quartile 3rd Quartile 4th Quartile <21.3μg/mL ≥21.3-<33μg/mL ≥33-<47.9μg/mL >47.9μg/mL (26.3%) (37.9%) (43.9%) (43.1%) <0.11μg/mL ≥0.11-<2.4μg/mL ≥2.4-<6.8μg/mL >6.8μg/mL (14.6%) (25.5%) (59.6%) (52.1%) <1.4μg/mL ≥1.4-<3.6μg/mL ≥3.6-<8.1μg/mL >8.1μg/mL (21.1%) (55.0%) (79.0%) (60.0%) Reinish W, Sandborn WJ et al., Digestive Disease Week 2012; Abstract # 566 P-values P=0.0504 P<0.0001 P=0.0066 Guidance for Patients Losing Response: Based on mAb Blood Levels and antimAbs Potential Treatment Algorithm Based on Therapeutic Anti-TNF Agent Concentrations change to another anti-TNF agent Positive AntimAb if no response, change to Rx with different mechanism of action (non anti-TNF agent) Increase mAb dose Afif W et al. Am J Gastroenteterol. 2010;105:1133-1139. Potential Treatment Algorithm Based on Therapeutic Anti-TNF Agent Concentrations Sub-therapeutic mAb concentration Increase mAb dose or frequency change to different antiTNF agent Afif W et al. Am J Gastroenteterol. 2010;105:1133-1139. If no response, change to different anti-TNF agent if no response, change to Rx with different mechanism of action (non anti-TNF agent) Potential Treatment Algorithm Based on Therapeutic Anti-TNF Agent Concentrations * Therapeutic mAb concentration endoscopy/CTE with active disease endoscopy/CTE with inactive disease change to Rx with different mechanism of action (non anti-TNF agent) investigate for alternate etiology of symptoms * Patients should have endoscopic or radiologic imaging Afif W et al. Am J Gastroenteterol. 2010;105:1133-1139. Clinical Utility of Measuring IFX and HACA Levels in Patients with IBD Clinical outcomes in patients with detectable HACA (N = 35)* Clinical outcomes in patients with sub-therapeutic concentrations (N = 69)* 100 100 92 P<0.004 80 60 40 17 20 Complete / Partial Response (%) Complete / Partial Response (%) P<0.016 86 80 60 40 40 20 0 0 Anti-TNF changed (11/12) Infliximab increased (1/6) * 6 discontinued IFX, 3 continued same dose 3, 3 proceeded to surgery, 5 patients could not be assessed Afif W, et al. Am J Gastroenterol 2010 May;105(5):1133-9. Anti-TNF changed Infliximab (2/6) increased (25/29) * 10 continued same dose, 9 discontinued IFX, 8 proceeded to surgery and 7 patients could not be assessed Prospective studies of maintaining trough levels and cost effectiveness in progress What about dose adjustments? Major issue (hassle factor) with 3rd Party Payors Efficacy of Intensification Regimes: Experience of a Single Referral Centre Objective: To evaluate the efficacy of intensification regimes of infliximab (IFX) and adalimumab (ADA) in patients with IBD with regard to therapeutic response and ability to return to normal dosing Methods: Retrospective review for intensification of therapeutic regimes of biological therapy in patients with IBD treated in center with IFX or ADA between October 2007 and September 2010 19 Lukas M, et al. DDW 2011. Abstract Mo1239. Anti-TNF Therapy for CD: Dose Escalation and Early Discontinuation Infliximab (n=199) Adalimumab (n=136) 10.9 yrs 15 yrs % on combined IS 64% 93% 1st anti-TNF used -- 37.5% Required dose escalation 38% 39% Required dose escalation by 1 yr 14% 32% Mean disease duration Predictors for dose escalation by longer disease duration Stopped therapy by 1 yr* Reasons for stopping therapy by stricturing phenotype; by prior anti-TNF exposure 29% Treatment failure, ADRs/drug allergy 13% Treatment failure, ADRs/drug allergy *Patients on combined IS therapy were less likely to stop therapy at 1 yr. Naik AS et al. Gastroenterology 2009;136(Suppl 1):A-654. Loss of Response to Adalimumab Dose Increase – CHARM Study 27 % over 1 year Approximately half of these maintain benefit and continue at the increased dose Colombel JF et al. Gastroenterology. 2007;132:52 EMEA website Influence of Trough Adalimumab Serum Levels and AAA on Long-term Outcome in Crohn’s Disease Study design: Patients with CD were treated adalimumab in a single tertiary center N=176 patients Follow-up: Median f/u 2 years Efficacy 71% response @ 4 wks 67% response @ 12 wks 65.4% (102/156) receiving maintenance therapy required dose escalation at end of f/u period 9.2% of patients developed AAA Karmaris Gastro 2009;137:1628–1640 Patients with sustained clinical response without dose escalation TR before & after escalation (µg/ml) Adalimumab Trough Levels and clinical response to dose escalation 25 20 Mann-Whitney: p<0.0001 15 10 5 5.9 0.0 0 absent CR (n=9) at least partial CR (n=24) CRto 40ew es calation Karmaris Gastro 2009;137:1628–1640 Efficacy of Intensification Regimes: Experience of a Single Referral Centre Results: IFX ADA 341 111 Intensification 47 (14%) 14 (13%) Interval ↓ 33 (70%) 100% Dose ↑ 6 (13%) n/a Both 8 (17%) n/a Median time to intervention 6 mo (3-21) 3 mo (1-7) Response after interval ↓ 22/33 (67%) 5/14 (36%) Return to normal dosing 50% 40% Courses of therapy Conclusions: Intensification of biological therapy restored clinical response in 54% of therapeutic interventions, with shortening of interval in IFX treatment being the most effective Approximately in half of the cases the normal dosing regime was possible to restore 24 Lukas M, et al. DDW 2011. Abstract Mo1239. WE NEED A COST-EFFECTIVE BIOMARKER FOR MUCOSAL HEALING 25 Correlations Between hsCRP, IL-6, Fecal Markers, CDAI, and Endoscopic Activity in Crohn’s Disease (N=164) hsCRP IL-6 Calprotectin Lactoferrin CDAI SES-CD 0.65 0.47 0.52 0.16 0.46 0.45 0.55 0.15 0.43 0.76 0.23 0.45 0.19 0.48 IL-6 Calprotectin Lactoferrin CDAI Correlation coefficients highlighted in red were significant (P < 0.05). When stratified by extent, correlation coefficients were highest for colonic disease. hs-CRP = high-sensitivity C-reactive protein; IL-6 = interleukin 6; CDAI, = Crohn’s Disease Activity Index; SES-CD, = Simple Endoscopic Score for Crohn's Disease. Jones JL, et al. Clin Gastroenterol Hepatol. 2008;6:1218-1224. 0.15 Use of fecal calprotectin as marker of disease activity in patients under maintenance treatment with infliximab for ulcerative colitis • N=113 UC patients on IFX 5mg/kg in stable remission with 5mg/kg IFX q8. Fecal calprotectin (FC) measured monthly for 1 year Deep remission (DR) = normal endoscopy at BL and wk 52 + Mayo score < 3 Active disease = clinical Mayo score or endoscopic score >2 at wek52 median FC < 50 mg/kg at all measured time points. # of Patients % of Patients – – – 25 Median FC 477 mg/kg. Increase in FC observed already 3mo before. Two consecutive FC measurements >300 mg/kg predicted flare FC levels highly correlate with disease activity in pts on IFX maintenance therapy for UC. DR is associated with very low levels of FC. A flare is associated with high levels (median >300 mg/kg). Two consecutive cp levels of >300 mg/kg predict a flare. De Vos et al. ECCO 2012, abstract OP 07 Close monitoring of CRP and fecal calprotectin levels to predict relapse in Crohn's disease patients. A sub-analysis of the STORI study • N= 113 CD patients in corticosteroid-free remission for ≥ 6mos on IFX and immunosuppressants (IS) . - IFX discontinued , CRP and calprotectin measured every 2 mos through 18 mos or clinical relapse. P = 0.001 P = 0.07 • CRP > 5mg/l and Calpro >250μg/g were associated with relapse in short term • After discontinuation of IFX in CD patients, elevated levels of CRP and calpro were associated with increased risk of short term relapse, even with high variability of markers during follow-up de Suray, et al. ECCO 2012, abstract P274 Fecal lactoferrin level is an indicator of mucosal healing 85 pts monitored for the complete 12-months 49 pts experienced sustained remission defined by CAI 44 achieved mucosal healing based on Endoscopy Score 0–1 41 did not show any signs of acute histological activity (Riley Score) FLA was the only biomarker to show a median level above cut-off for active disease defined by endoscopy as well as histology for pts in sustained clinical remission 29 Langhorst J., et al. ECCO 2012. Abstract P095. Fecal lactoferrin level is an indicator of mucosal healing Fecal lactoferrin (FLA) level is an indicator of mucosal healing in patients with ulcerative colitis: A prospective 12-month monitoring study 85 pts monitored for the complete 12-months 36 pts suffered a flare 49 pts experienced sustained remission defined by CAI. Flare Remission P-value Median FLA levels (µg/g) 40 5 <0.0001 Median CRP levels (mg/dl) 0.6 0.1 <0.001 Median WBC levels 7.6 6.0 0.01 Mucosal activity Mucosal healing Median FLA levels (µg/g) 37 5 0.09 Median CRP levels (mg/dl) 0.1 0.2 0.882 Median WBC levels 6.0 5.9 0.787 Histologic activity No histologic activity Median FLA levels (µg/g) 14.4 4.6 0.198 Median CRP levels (mg/dl) 0.2 0.1 0.948 Median WBC levels 6.0 6.0 P-value P-value 0.759 30 Langhorst J., et al. ECCO 2012. Abstract P095. Calprotectin and Disease Activity Author Patient Assessment Lactoferrin Calprotectin CRP popula endoscopic (Sensitivity / (Sensitivity / (Sensitivity / tion disease Specificity) Specificity) Specificity) activity Roseth(2004) Solem (2005) CD and UC CD Siponnen (2008) CD Study specific index CDEIS 77% / 100% Siponnen (2008) CD CDEIS 66%-71% / 83%-92% 70%-91% / 44%-92% Siponnen (2010) CD SES-CD 80% / 67% 80% / 89% D’Inca (2007) CD SES-CD 77% / 80% 81% / 80% D’Inca (2007) UC Mayo score 75% / 60% 78% / 70% Schoepfer (2009) UC Rachmilewitz Index 86% - 93% / 71% - 88% Schoepfer (2010) CD CDEIS 89% / 58% Farup method Lewis JD. Gastroenterology 2011;13: 100% / 100% 54% / 75% 87% / 100% 48% / 91% 68%/58% Predictive Value of Calprotectin for Clinical Relapse Tibble JA et al. Gastroenterology 2000:119:15-22 Calprotectin to Predict Relapse Author Gisbert* Tibble Tibble Costa Costa D’Inca Sipponen Walkiewicz Patients UC UC CD UC CD UC UC+CD CD Duration of remission at entry >6 mos. 1-4 mos. 1-4 mos. 1-12 mos. 1-12 mos. 3-36 mos. > 3mos (51% >12 months) Not stated * NPV 100% at 12 weeks Lewis JD. Gastroenterology 2011;13 Elevated Level >150μg/g >50μg/g >50μg/g >150μg/g >150μg/g >130μg/g >100μg/g Relapse Rate with Low Calpro 9% 10%* 15% 10% 57% 30% 25% Relapse Rate with High Calpro 31% 85%* 85% 81% 87% 79% 39% >400μg/g 11% 56% Monitoring Inflammation Can Fecal Calprotectin detect subclinical inflammation? predict future flares? 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% CD and UC in clinical remission Cutoff of 167 Prediction of future flares 100% 72% 69% 75% Sensitivity Specificity 3 months Gisbert, IBD 2009; 15: 1190. 1 year You Can’t Always Get What you Want….