Management of Anticoagulants & Antiplatelet Agents Pre and Post
advertisement

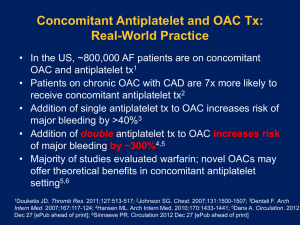
Management of Anticoagulants & Antiplatelet Agents Pre and Post Endoscopy Thomas Savides, M.D. Professor of Clinical Medicine University of California, San Diego Disclosures • None Learning Objectives • Accurately assess the risk of bleeding in patients on anticoagulants and antiplatelet agents before endoscopic procedures • Learn the cardiovascular risk of modifying antiplatelet therapy in the peri-endoscopic setting • Understand current best-practice recommendations for management of anticoagulants after endoscopic procedures Balancing Risks of Bleeding vs Risk of Thromboembolism Bleed after endoscopy Thromboembolic Event Issues to Consider • • • • Risk of bleeding vs risk of thrombosis Bleeding risk from endoscopic procedure Thromboembolism risk if stop antithrombotics Emergency vs elective procedure Anti-Thrombotic Agents • Anticoagulants – Warfarin – Heparin – Low molecular weight heparin • Anti-platelet agents – Aspirin – Non-steroidal antiinflammatory agents (NSAID) – Thienopyridine (clopidogrel, ticlopidine) – Glycoprotein IIb/IIIa receptor inhibitors ASGE and ESGE Guidelines on Endoscopy and Antithrombotic Agents Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Bleeding Risks For Endoscopic Procedures Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Bleeding Risk During Endoscopic Procedures - ESGE Low Risk High Risk • • • • • • • • • • • • EGD Colonoscopy EUS EUS FNA solid lesion Colon polypectomy <1 cm Stricture dilation Stent placement ERCP with stent or balloon dilation • Argon plasma coagulation • • • • EMR/ESD Ampullectomy ERCP with sphincterotomy ERCP with large balloon dilation of papilla Colon polypectomy > 1 cm EUS FNA of cystic lesions Percutaneous endoscopic gastrostomy (PEG) Esophageal variceal band ligation Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 What are the risks of thromboembolic events around endoscopy? • Depends on the condition for which antithrombotic therapy is being used Low Risk High Risk High Risk Conditions for Thromboembolic Events • Atrial Fibrillation with h/o embolic events or valve disease • Prosthetic Valve • Coronary artery disease and stents • Deep Venous Thrombosis/Pulmonary Embolus • Stroke/Transient Ischemic Attack • Hypercoagulable states Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Atrial Fibrillation High risk conditions for thomboembolic events • Previous stroke (CVA) or transient ischemic attack (TIA) • CHADS2 score ≥ 3 • • • • • CHF=1 HTN=1 Age ≥ 75=1 Diabetes=1 Previous CVA/TIA=2 • Associated valvular heart disease Kwok and Faigel, AJG 2009 Prosthetic Valve High risk conditions for thomboembolic events • Bioprosthetic valve <3 months old • Mechanical valve in mitral position • Mechanical valve with previous thromboembolic event Coronary Artery Disease and Stents High risk conditions for thomboembolic events • Recent acute coronary event <4-6 weeks • Discontinuing dual antiplatelet therapy in: – Drug-eluting stent < 1 year – Bare metal stent < 1 month Deep Venous Thrombosis/Pulmonary Emboli High risk conditions for thomboembolic events • Discontinuing anticoagulation <3 months from event • Recurrent DVT/PE • Severe hypercoagulable states – Cancer – Paroxysmal nocturnal hemoglobinuria – Myeloproliferative syndrome Stroke/Transient Ischemic Attack High risk conditions for thomboembolic events • • • • Cardioembolic events Carotid artery disease Recent carotid endarterectomy Hypercoagulable state General Approach to Patients on Antithrombotic agents who need endoscopy • Delay elective endoscopy until patient at lower risk for thromboembolism • Discuss with patient’s cardiovascular or neurovascular physician whether (or when) drugs can be stopped • Realize that only limited data exist • Guidelines from ASGE, ESGE are only suggestions Need to weigh the risks and benefits for each individual patient Elective Procedures in Patients on antithrombotic drugs EGD Procedures Procedure Risk Bleeding Stop Aspirin? Stop Clopidogrel or Prasugrel? EGD ± biopsy Low No No EGD with stricture dilation Low No No EGD with APC Low No Yes EGD with stent placement Low No Yes EGD with variceal band ligation High No Yes EGD with PEG placement High No ? EGD with EMR/ESD High Yes Yes Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 Colonoscopy Procedures Procedure Risk of Bleeding Stop aspirin Stop clopidogrel or prasugrel? Colonoscopy ± biopsy Low No No Colonoscopy with polypectomy <1 cm Low No No Colonoscopy with polypectomy >1 cm High No Yes Colonoscopy with EMR/ESD High Yes Yes Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 ERCP Procedures Procedure Risk Bleeding Stop Aspirin? Stop Clopidogrel or Prasugrel? ERCP Diagnostic Low No No ERCP with Stent Placement Low No No ERCP with sphincterotomy High No Yes ERCP with High sphincterotomy and large balloon papillary dilation Yes Yes Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 EUS Procedures Procedure Risk Bleeding Stop Aspirin? Stop Clopidogrel or Prasugrel? EUS Diagnostic Low No No EUS with FNA Solid Mass Low No Yes EUS FNA Cysts High Yes Yes ERCP FNA Therapeutic High Yes Yes Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 Warfarin Management prior to Endoscopy • Avoid using Vitamin K to reverse anticoagulation before elective procedures because delays therapeutic reanticoagulation after procedure • Warfarin can usually be stopped for 4-7 days and then be restarted the following day • 1% risk of thromboembolic events after temporary warfarin cessation (Garcia, Arch Intern Med 2008) • High risk patients for thromboembolic events should consider bridging therapy with low molecular weight heparin. Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Management of antithrombotic agents in the ELECTIVE endoscopic setting Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Endoscopic Techniques Can Decrease Bleeding After Elective Polypectomy Boustiere, ESGE Guidelines: Endoscopy and antiplatelet agents. Endoscopy 2011 Endoscopy in the Acutely Bleeding Patient Receiving Antithrombotic Therapy Stopping or Reversing Antithrombotic Agents in the acutely bleeding patient • Warfarin – Consider holding warfarin – Consider vitamin K, FFP, Factor VIIa • AHA/ACC recommendations – Fresh frozen plasma (FFP) preferable to high dose Vitamin K – Avoid high-dose Vitamin K (10 mg) in patients with mechanical valves as may cause hypercoagulable state » Low dose Vitamin K (1-2 mg) may be fine • Antiplatelet agents – Consider stopping drug – Consider platelet transfusion Efficacy of endoscopic therapy in patients actively taking antithrombotic drugs • Retrospective studies suggest endoscopic therapy seems safe and effective (even with INR >4) • Mechanical hemostasis (i.e. clips) preferred – Especially if will resume antithrombotic meds Restarting antithrombotic agents after endoscopic hemostasis • Resumption of aspirin + PPI has lower rate of recurrent peptic ulcer bleeding than switching to clopidogrel (Chan, NEJM 2005) • Continuation of low dose aspirin after endoscopic hemostasis results in lower all cause mortality (12.9% vs 1.3%) and higher rebleed rate (10.3% vs 5.4%) (Sung JJ, Ann Int Med 2010) Asia-Pacific Working Group Consensus on Non-Variceal Bleeding (Sung JJ,Gut 2011) • Among aspirin users with high cardiothrombotic risk who develop ulcer bleeding, aspirin should be resumed as soon as possible once hemostasis is established – Because risk of rebleeding is greatest in 1st 72 hours, consider restart aspirin 3-5 days after hemostasis – Uncertain about clopidogrel, but perhaps restart in 35 days – If dual therapy; no data; depends on type of stent and when placed Endoscopy in the Setting of Acute Coronary Syndrome • 1-3% of patients with ACS will have GIB • GIB in setting of ACS has 4-7 fold increased risk of in-hospital morality • Risk of EGD and Colonoscopy 1-2% in setting of ACS • Note that with advent of intravenous PPI, less need for emergent need for EGD in mildmoderate UGI bleeds Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Management of antithrombotic agents in the URGENT endoscopic setting Management of antithrombotic agents for endoscopic procedures. ASGE Standards of Practice Committee. 2009 Do proton pump inhibitors impair efficacy of clopidogrel? • Mixed initial data • Recent NEJM article (Bhatt 2010) suggests no Conclusions • Most endoscopic procedures safe to perform even if patient taking aspirin and/or NSAIDs • Continuing antithrombotic therapy may improve overall outcomes (i.e. survival after ACS) even if higher rate of rebleeding • Need to individualize for each patient given limited data available for guidelines Thank You Del Mar, California