Grades
advertisement
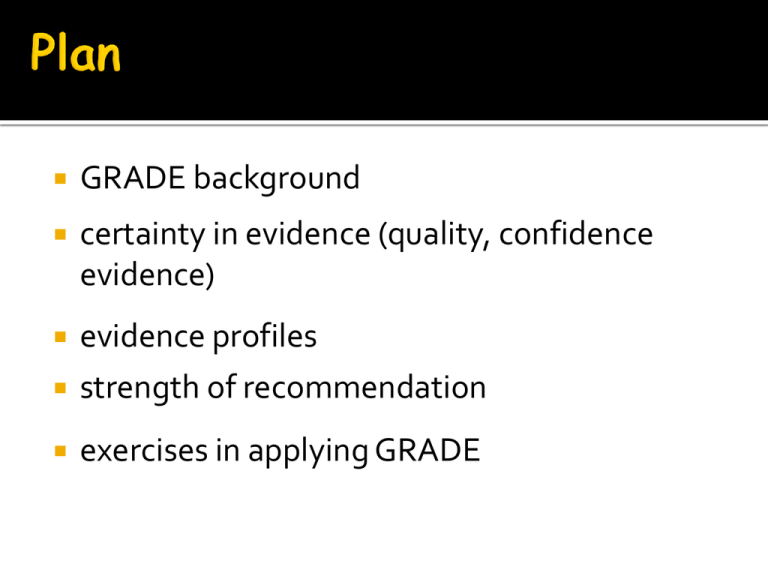
GRADE background certainty in evidence (quality, confidence evidence) evidence profiles strength of recommendation exercises in applying GRADE experience participating guideline panels? clin epi methodology course? is grading recommendations a good idea? If so, why? experience with grading systems used? many available Australian National and MRC Oxford Center for Evidence-based Medicine Scottish Intercollegiate Guidelines (SIGN) US Preventative Services Task Force American professional organizations AHA/ACC, ACCP, AAP, Endocrine society, etc.... cause of confusion, dismay GRADE (Grades of recommendation, assessment, development and evaluation) international group Australian NMRC, SIGN, USPSTF, WHO, NICE, Oxford CEBM, CDC, CC ~ 35 meetings over last 14 years ▪ (~10 – 70 attendants) 2004 BMJ, first description 2008 BMJ six part series for guideline users 2010-13, 21 part series, 15 published for systematic review authors, HTA practitioners, guideline developers interventions management strategy 1 versus 2 what grade is not about individual studies (body of evidence) diagnostic accuracy questions in patients with a sore leg, what is the accuracy of a blood test (D-Dimer) in sorting out whether a deep venous thrombosis is the cause of the pain prognosis what it is about: diagnostic impact are patients better off (improved outcomes) when doctors use the d-dimer test 80+ Organizations 2005 2006 2007 2008 2009 2010 2011 9 GRADE uptake two components certainty in estimate of effect adequate to support decision (quality of body of evidence) high, moderate, low, very low Likelihood of and confidence in an outcome Quality Initial choice, defined as confidence natural to clinicians, but confusion with risk of bias Confidence what we actually mean, but confusion with confidence intervals, and experts always confident Certainty avoids confusion of others, experts might acknowledge uncertainty - Current preferred term two components certainty in evidence adequate to support decision (quality of body of evidence) high, moderate, low, very low strength of recommendation strong and weak weak alternatives conditional, contingent, discretionary Health Care Question (PICO) Systematic reviews Studies S1 S2 S3 S4 Outcomes OC1 OC2 OC3 OC4 OC1 OC2 Important outcomes Critical outcomes S5 OC3 OC4 Generate an estimate of effect for each outcome Rate the quality of evidence for each outcome, across studies RCTs start high, observational studies start low (-) Study limitations Imprecision Inconsistency of results Indirectness of evidence Publication bias likely (+) Large magnitude of effect Dose response Plausible confounders would ↓ effect when an effect is present or ↑ effect if effect is absent Final rating of quality for each outcome: high, moderate, low, or very low Rate overall quality of evidence (lowest quality among critical outcomes) Decide on the direction (for/against) and grade strength (strong/weak*) of the recommendation considering: Quality of the evidence Balance of desirable/undesirable outcomes Values and preferences *also labeled “conditional” or “discretionary” Decide if any revision of direction or strength is necessary considering: Resource use patients: Males over 50 presenting with fatigue, malaise and erecticle dysfunction with laboratory evidence of decreased testosterone intervention, testosterone comparator no testosterone outcomes? Where to start RCTs and observational studies (High, moderate, low, very low)? Recall antioxidant vitamins Observational studies less cancer, CV outcomes RCTs no difference Result observed repeatedly What went wrong? RCTs start high observational studies start low what can lower confidence? risk of bias inconsistency indirectness imprecision publication bias what to consider? well established concealment intention to treat principle observed blinding completeness of follow-up more recent selective outcome reporting bias Stopping early for benefit what to consider? accurate assessment of exposure adjusted analysis for all important prognostic factors, accurately measures accurate assessment of outcome completeness of follow-up 6 studies, 100 patients each 3 studies low risk of bias, 3 high rate down for risk of bias? How did you decide? Similarity of point estimates less similar, less happy Overlap of confidence intervals less overlap, less happy -40 -24 -8 8 RRR (95% CI) 24 40 56 Homogenous test for heterogeneity what is the p-value? what is the null hypothesis for the test for heterogeneity? Ho: RR1 = RR2 = RR3 = RR4 p=0.99 for heterogeneity Heterogeneous test for heterogeneity what is the p-value? p-value for heterogeneity < 0.001 p-value for heterogeneity < 0.001 2 I Interpretation 100% Why are we pooling? 75% Very concerned 50% Getting concerned 25% Only a little concerned 0% No worries Homogenous What is the I2 ? p=0.99 for heterogeneity I2=0% Heterogeneous What is the I2 ? p-value for heterogeneity < 0.001 I2=89% Relative Risk with 95% CI for Vitamin D Non-vertebral Fractures Relative Risk with 95% CI for Vitamin D (Non-Vertebral Fractures, Dose >400) Relative Risk with 95% CI for Vitamin D (Non-Vertebral Fractures, Dose = 400) within-study comparison? No unlikely chance Yes, p = 0.006 consistent across studies Yes one of small number a priori hypothesis with direction Yes biologically compelling Yes shall we believe sub-group analysis? no way 0 sure thing 100 populations older, sicker or more co-morbidity interventions warfarin in trials vs clinical practice outcomes important versus surrogate outcomes glucose control versus CV events Directness interested in A versus B available data A vs C, B vs C Alendronate Risedronate Placebo small sample size small number of events wide confidence intervals uncertainty about magnitude of effect how do you decide what is too wide? primary criterion: would decisions differ at ends of CI atrial fib at risk of stroke warfarin increases serious gi bleeding 3% per year 1,000 patients 1 less stroke 30 more bleeds for each stroke prevented 1,000 patients 100 less strokes 3 strokes prevented for each bleed where is your threshold? how many strokes in 100 with 3% bleeding? 1.0% 0 1.0% 0 1.0% 0 1.0% 0 pts with threatened stroke RCT of clopidogrel vs ASA 19,185 patients ischaemic stroke, MI, or vascular death compared 939 events (5·32%) clopidogrel 1021 events (5·83%) with aspirin RR 0.91 (95% CI 0.83 – 0.99) (p=0·043) rate down for precision? Clopidogrel or ASA for threatened vascular events RCT 19,185 patients 1.7% - 0.9 – 0.1% 1.0% 0 RR 0.91 (95% CI 0.83 – 0.99) small trials, large effect likely to be overestimate analogy to stopping early lack of prognostic balance solution: optimal information size # of pts from conventional sample size calculation specify control group risk, α, β, Δ Fluoroquinolone prophylaxis in neutropenia: infection-related mortality Total number of events: 47 Fluoroquinolone prophylaxis in neutropenia: infection-related mortality sample size 1,002 α 0.05, β 0.20, Δ 0.25 RRR, CER 7% N = 6,000 high likelihood could lower quality when to suspect number of small studies industry sponsored What do you do high certainty, no RCTs? common criteria everyone used to do badly almost everyone does well quick action insulin for diabetic ketoacidosis? thyroxine for thyroid deficiency? hydrocortisone for adrenal insufficiency? childhood lymphoblastic leukemia risk for CNS malignancies 15 years after cranial irradiation no radiation: 1% (95% CI 0% to 2.1%) 12 Gy: 1.6% (95% CI 0% to 3.4%) 18 Gy: 3.3% (95% CI 0.9% to 5.6%). Cetainty assessment criteria What to do when certainty differs across outcomes? options ignore all but primary previous approach least certainty of any outcome some blended approach least certainty of critical outcomes Trading off desirable and undersirable what do patients/clinicians need to know relative risk reduction? absolute risk difference? Toxic treatment, 50% RRR mortality? OK? 1% to 1/2% OK? 40% to 20%, OK? body of evidence how do we get risk difference? meta-analysis get pooled relative risk obtain baseline risk and multiply BR 10%, RRR 50%, RD 5% why not get risk difference directly? RR 0.67 RD 10% RR 0.67 RD 3.3% RR 0.67 RD 1% High versus low PEEP in ALI and ARDS Population No. of participants (trials) † Higher PEEP Lower PEEP Adjusted Relative Risk (95% CI; P-value) ‡ Adjusted Absolute Risk Difference (95% CI) Patients with ARDS 1892 (3) 324/951 (34.1%) 368/941 (39.1%) 0.90 (0.81 to 1.00; 0.049) -3.9% (-7.4% to -0.04%) Patients without ARDS 404 (3) 50/184 (27.2%) 41/220 (18.6%) 1.37 (0.98 to 1.92; 0.065) 6.9% (-0.4% to 17.1%) Quality High Moderate (imprecision) strong recommendation benefits clearly outweigh risks/hassle/cost risk/hassle/cost clearly outweighs benefit what can downgrade strength? low confidence in estimates close balance between up and downsides aspirin after myocardial infarction 25% reduction in relative risk side effects minimal, cost minimal benefit obviously much greater than risk/cost warfarin in low risk atrial fibrillation warfarin reduces stroke vs ASA by 50% but if risk only 1% per year, ARR 0.5% increased bleeds by 1% per year Strength of Recommendations Aspirin after MI – do it Warfarin rather than ASA in Afib -- probably do it -- probably don’t do it variability in patient preference strong, almost all same choice (> 90%) weak, choice varies appreciably interaction with patient strong, just inform patient weak, ensure choice reflects values use of decision aid strong, don’t bother; weak, use the aid quality of care criterion strong, consider; weak, don’t consider choice more preference dependent risk aversion steroids for pulmonary fibrosis low quality evidence in support of benefit high quality evidence of toxicity recommendation to the hopeful patient I’m likely to deteriorate if something might work, let’s try it damn the torpedoes recommendation to the fearful patient doctor, you mean you know it’s toxic diabetes, skin changes, body habitus, infection, osteoporosis you don’t know for sure it works? are you crazy? weak recommendation mandated Comparator often not clear Children with suspected or confirmed tuberculous meningitis should be treated with a four-drug regimen (HRZE) for 2 months, followed by a twodrug regimen (HR) for 10 months Offer and promote postpartum and post-abortion contraception to adolescents through multiple home visits and/or clinic visits Strong recommendations, Low certainty: Discordant recs Experts use often Why? What are the possibilities? panels don’t believe their own confidence ratings personal conviction trumps evidence believe weak recommendations ignored influence funders Discordant recommendations: What are the possibilities? good practice mistaken judgment inappropriate exceptional situation they got it right For patients with congenital adrenal hyperplasia, we recommend monitoring patients for signs of glucocorticoid excess Wealth of indirect linked evidence High confidence in net benefit Benefit clear Minimal harms or costs Poor use of guideline panel time effort summarize symptoms and signs appear not infrequently Collect cohort studies of incidence Studies of accuracy of symptoms and signs patients suffer if clinicians fail to recognize Reports of untreated glucocorticoid excess clinical action can ameliorate the problem Evidence supporting therapy describe how evidence is linked Is the statement clear and actionable? Is the message really necessary? Is the net benefit large and unequivocal? Is the evidence difficult to collect and summarize? If a public health guideline, are there specific issues that should be considered (e.g. equity) Have you made the rationale explicit? Is this better to be formally GRADEd? For patients with congenital adrenal hyperplasia, we recommend monitoring patients for signs of glucocorticoid excess Monitor how often? Nature of monitoring What to do if signs of excess found For patients with congenital adrenal hyperplasia, we recommend monitoring patients for signs of glucocorticoid excess Really plausible that clinicians won’t monitor? If not, not necessary relevant symptoms and signs appear not infrequently patients will suffer if clinicians fail to recognize these signs clinical action can ameliorate the problem. 1 LQE in a life-threatening situation Fresh frozen plasma and intracranial bleed 2 LQoE benefit and HQoE suggests harm Head-to-toe CT/MRI screening for cancer. 3 LQoE suggests equivalence, HQoE less harm for one alternative Helicobacter pylori eradication early stage gastric MALT lymphoma 4 HQoE suggests equivalence, LQoE suggests harm in one alternative ACEI in hypertension in women planning conception and in pregnancy. 5 HQoE suggests benefit in one Testosterone in males with or at outcome, LQoE suggests harm risk of prostate cancer in more highly valued outcome 1 LQE in a life-threatening situation Fresh frozen plasma and intracranial bleed 2 LQoE benefit and HQoE suggests harm Head-to-toe CT/MRI screening for cancer. 3 LQoE suggests equivalence, HQoE less harm for one alternative Helicobacter pylori eradication early stage gastric MALT lymphoma 4 HQoE suggests equivalence, LQoE suggests harm in one alternative ACEI in hypertension in women planning conception and in pregnancy. 5 HQoE suggests benefit in one Testosterone in males with or at outcome, LQoE suggests harm risk of prostate cancer in more highly valued outcome 1 LQE in a life-threatening situation Fresh frozen plasma and intracranial bleed 2 LQoE benefit and HQoE suggests harm Head-to-toe CT/MRI screening for cancer. 3 LQoE suggests equivalence, HQoE less harm for one alternative Helicobacter pylori eradication early stage gastric MALT lymphoma 4 HQoE suggests equivalence, LQoE suggests harm in one alternative ACEI in hypertension in women planning conception and in pregnancy. 5 HQoE suggests benefit in one Testosterone in males with or at outcome, LQoE suggests harm risk of prostate cancer in more highly valued outcome 1 LQE in a life-threatening situation Fresh frozen plasma and intracranial bleed 2 LQoE benefit and HQoE suggests harm Head-to-toe CT/MRI screening for cancer. 3 LQoE suggests equivalence, HQoE less harm for one alternative Helicobacter pylori eradication early stage gastric MALT lymphoma 4 HQoE suggests equivalence, LQoE suggests harm in one alternative ACEI in hypertension in women planning conception and in pregnancy. 5 HQoE suggests benefit in one Testosterone in males with or at outcome, LQoE suggests harm risk of prostate cancer in more highly valued outcome 1 LQE in a life-threatening situation Fresh frozen plasma and intracranial bleed 2 LQoE benefit and HQoE suggests harm Head-to-toe CT/MRI screening for cancer. 3 LQoE suggests equivalence, HQoE less harm for one alternative Helicobacter pylori eradication early stage gastric MALT lymphoma 4 HQoE suggests equivalence, LQoE suggests harm in one alternative ACEI in hypertension in women planning conception and in pregnancy. 5 HQoE suggests benefit in one Testosterone in males with or at outcome, LQoE suggests harm risk of prostate cancer in more highly valued outcome systematic survey of all published ES guidelines between 2005 and 2011 screening and extraction in duplicate for each recommendation: confidence in estimates, strength of recommendation strong recommendations based on LQE taxonomy for paradigmatic recommendations applied Condition 1 Best practice statements 2 Additional research 3 4 Example For patients with Congenital Adrenal Hyperplasia, we recommend monitoring patients for signs of glucocorticoid excess We recommend additional investigation using rodents and primates to further define the specific targets of androgen action Mistaken judgment For overweight and obese children and adolescents, intensive lifestyle modification for the patient and entire family Inappropriate strong recommendation In patients with primary aldosteronism who are unable or unwilling to undergo laparascopic adrenalectomy, we recommend medical treatment with mineralocorticoids Strong recommendations (n=206): n (%) High/moderate confidence in estimates 85 (41%) Very low/low confidence in estimates 121 (59%) Totals (%) 206 (100%) Weak recommendations (n=151): High/moderate confidence in estimates Very low/ low confidence in estimates Totals (%) n (%) 16 (8%) 135 (92%) 151 (100%) N - 35 1 LQE in a life-threatening situation 13 LQoE benefit and HQoE suggests harm or a very high cost 7 LQoE suggests equivalence, HQoE less harm for one of the competing alternatives. 5 HQoE suggests equivalence of two alternatives and LQoE suggests harm in one alternative 9 HQoE suggests modest benefits and LQoE suggests possibility of catastrophic harm Appropriate 29% Inappropriate 71% Condition N = 86 Condition 43 Best practice 5 Appropriate 29% Mistaken judgment 5 Additional research 33 Inappropriate strong recommendation Inappropriate 71% majority ES recommendations strong 121 (59%) discordant 35/121 (29%) of discordant appropriate of 86 inappropriate, 43 (50%) best practice statements 33/86 inappropriate, should have been weak recommendations underlying values and preferences always present sometimes crucial important to make explicit Stroke guideline: patients with TIA clopidogrel over aspirin (Grade 2B). Underlying values and preferences: This recommendation to use clopidogrel over aspirin places a relatively high value on a small absolute risk reduction in stroke rates, and a relatively low value on minimizing drug expenditures. peripheral vascular disease: aspirin be used instead of clopidogrel (Grade 2A). Underlying values and preferences: This recommendation places a relatively high value on avoiding large expenditures to achieve small reductions in vascular events. Consider UpToDate style of values and preferences Weak recommendation low certainty evidence for trial of testosterone in men with apparent testosterone deficiency and cardiovascular disease Men who place a high value on minimizing risk of an adverse cardiovascular event and a relatively low value in ameliorating the symptoms of testosterone deficiency are likely to choose against testoserone use venotonic agents mechanism unclear, increase venous return popularity 90 venotonics commercialized in France none in Sweden and Norway France 70% of world market possibilities French misguided rest of world missing out 14 trials, 1432 patients key outcome risk not improving/persistent symptoms 11 studies, 1002 patients, 375 events RR 0.4, 95% CI 0.29 to 0.57 minimal side effects is France right? what is the certainty of evidence? risk of bias lack of detail re concealment questionnaires not validated indirectness – no problem inconsistency, need to look at the results Review : Comparison: Outcome: Study or sub-category Phlebotonics for hemorrhoids 01 Venotonics vs placebp 08 Overall improvement: no improvement/some improvement RR (random) 95% CI log[RR] (SE) Weight % 01 Up to seven days -0.8916 (0.2376) Chauvenet -2.2073 (0.6117) Cospite -0.4308 (0.2985) Thanapongsathorn Subtotal (95% CI) Test for heterogeneity: Chi² = 6.92, df = 2 (P = 0.03), I² = 71.1% Test for overall effect: Z = 2.67 (P = 0.008) 02 Up to four w eeks -1.6094 (0.7073) Annoni F -0.9943 (0.3983) Clyne MB -1.1712 (0.3086) Pirard J -1.1087 (1.1098) Thanapongsathorn 0.2624 (0.3291) Thorp -0.8916 (0.3691) Titapan -0.5978 (0.1375) Wijayanegara Subtotal (95% CI) Test for heterogeneity: Chi² = 13.87, df = 6 (P = 0.03), I² = 56.7% Test for overall effect: Z = 3.57 (P = 0.0004) 12.67 5.51 11.18 29.36 0.41 0.11 0.65 0.37 [0.26, [0.03, [0.36, [0.18, 0.65] 0.36] 1.17] 0.77] 4.50 8.94 10.94 2.18 10.46 9.56 14.97 61.54 0.20 0.37 0.31 0.33 1.30 0.41 0.55 0.48 [0.05, [0.17, [0.17, [0.04, [0.68, [0.20, [0.42, [0.32, 0.80] 0.81] 0.57] 2.91] 2.48] 0.85] 0.72] 0.72] 03 Further than four w eeks -1.7719 (0.3906) Godeberg Subtotal (95% CI) Test for heterogeneity: not applicable Test for overall effect: Z = 4.54 (P < 0.00001) Total (95% CI) Test for heterogeneity: Chi² = 28.66, df = 10 (P = 0.001), I² = 65.1% Test for overall effect: Z = 5.14 (P < 0.00001) 0.001 0.01 0.1 Favours treatment 1 10 100 Favours control RR (random) 95% CI 9.10 9.10 0.17 [0.08, 0.37] 0.17 [0.08, 0.37] 100.00 0.40 [0.29, 0.57] 1000 size of studies 40 to 234 patients, most around 100 all industry sponsored Phlebotonics for hemorrhoids Review : Comparison: 01 Venotonics vs placebp 08 Overall improvement: no improvement/some improvement Outcome: 0.0 0.4 0.8 1.2 1.6 0.001 0.01 0.1 1 10 100 1000 RR (fixed) risk of bias lack of detail re concealment questionnaires not validated inconsistency almost all show positive effect, trend heterogeneity p < 0.001; I2 65.1% indirectness imprecision RR 0.4, 95% CI 0.29 to 0.57 publication bias 40 to 234 patients, most around 100 recommendation yes no against use strength strong weak Beta blockers in non-cardiac surgery Summary of Findings Quality Assessment Quality Relative Effect (95% CI) Outcome Number of participants (studies) Risk of Bias Consistency Directness Precision Publication Bias Myocardial infarction 10,125 (9) No serious limitations No serious imitations No serious limitations No serious limitations Not detected High 0.71 (0.57 to 0.86) Mortality 10,205 (7) No serious limitations No serious limiations No serious limitations Imprecise Not detected Moderate 1.23 (0.98 – 1.55) Stroke 10,889 (5) No serious limitaions No serious limitations No serious limitations No serious limitations Not detected High 2.21 (1.37 – 3.55) Absolute risk difference 1.5% fewer (0.7% fewer to 2.1% fewer) 0.5% more (0.1% fewer to 1.3% more) 0.5% more (0.2% more to 1.3% more0 GRADE values and preferences GRADE diagnosis Aspirin for primary prevention Culprit only vs complete revascularization in STEMI Management of esophageal varices