integrated care - Health Education England
advertisement
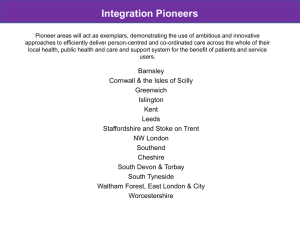
Integrated Care Pioneer The view from Islington Dr Josephine Sauvage Vice Chair Islington CCG In collaboration with NHS England “We are sick of falling through the gaps. We are tired of organisational barriers and boundaries that delay or prevent our access to care. We do not accept being discharged from a service into a void. We want services to be seamless and care to be continuous.” Individual’s viewpoint on fragmented care National Voices, May 2013 What do patients want? Coordinated care, centred on me Emergencies are not treated as isolated cases but within the context of my care plan My goals and desired outcomes are understood by all Providers are communicating with one another about me and my needs Information is common so I only have to give it once 3 I do not have to manage transitions between providers myself My care is planned to achieve my goals / desired outcomes Decisions are made based on my care plan Ethos of Pioneer ‘Integrated Care and Support: Our Shared Commitment’ (2013) A collaboration of national partners set out an ambitious vision of making person-centred coordinated care and support the norm across England over the coming years Association of Directors of Adult Social Care, Association of Directors of Children’s Services, Care Quality Commission, Department of Health, Health Education England, Local Government Association, Monitor, NHS England, NHS Improving Quality, National Institute for Health and Care Excellence, Public Health England, Social Care Institute for Excellence, Think Local Act Personal • • • • • • • • • • • Support of better person-centred, coordinated care Local innovation Realisations of local aspirations on integrated care Address barriers Disseminate and promote learning Focus on benefit for patients, services users, their carers and their local communities Provide bespoke expertise, support and constructive challenge Range of national and international experts This approach builds on the community budget pilots co-designing integrated health and care at scale and pace. Successive cohorts of Pioneers, supporting them for up to five years Expectation of Pioneers to contribute to accelerated learning across the system 5 year Expectations from pioneers • Be regarded as exemplars: – deliver improved outcomes, including better experiences for patients and people who use services – tackle local cultural and organisational barriers – realise savings and efficiencies for re-investment • Have used the Narrative developed by National Voices, in association with Making it Real, to help shape good, person-centred coordinated care and support for individuals in their area • Have demonstrated a range of approaches and models involving whole system transformation across a range of settings • Have demonstrated the scope to make rapid progress • Have tested radical options, including new reimbursement models and taking the risk of ‘failure to integrate’ in some cases • Have overcome the barriers to delivering coordinated care and support • Have accelerated learning across the system to all localities • Have improved the robustness of the evidence base to support and build the value case for integrated care and support Selection criteria (not prescriptive about models for adoption) • Articulate a clear vision of innovative approaches to integrated care and support • Plan for whole system integration • Demonstrate commitment to integrate care and support across the breadth of relevant stakeholders • Demonstrate the capability and expertise to deliver successfully a public sector transformation project at scale and pace • Commit to sharing lessons on integrated care and support across the system • Demonstrate that its vision and approach are based on a robust understanding of the evidence Integration Pioneers • The national collaborative announced details of an integration ‘Pioneer’ programme in May - over 110 applications were received nationally • Significant interest in becoming a pioneer across London with 15 applications crossing 22 boroughs demonstrating London’s commitment to integration • 4 Pioneers (NWL, Islington, WELC, Greenwich) have been selected in London covering approximately 1/3 of London’s population. • London’s Pioneers vary significantly in scale with large system and borough approaches. • The Pioneer community in London provides a significant opportunity to help London deliver integrated care at scale and pace, by sharing learning and developing solutions to complex issues. 7 The London Landscape Risk stratifying the population shows us that different patients have different intensity and complexity of need Very high risk High risk (0.5-5%) Moderate risk (5-20%) ~20% of the population Care for people with very complex needs Care for people with manageable long term conditions More complex (often multiple) conditions and facing higher risks to their health (end of life, frail elderly, dementia, multiple long term conditions) In frequent contact with multiple parts of the health and social care system i.e. the most complex and costly care Low risk (20-50%) Very low risk (50-100%) 9 “Care at short notice” for the rest of the population SOURCE: NWL whole systems integrated care The Case for Change Groups for whom the case for integrating care is most compelling • Frailty • Multiple co-morbidity • End of life Care • Dementia 10 The case for change for dementia Trends • There are around 65,000 Londoners with dementia, this is forecast to rise by 16% to 2021 and by 32% to 2031 [8] Outcomes and Experience • Half of all people with dementia never receive a diagnosis [9] - just 31% of the capital’s GPs believe they have received sufficient basic and post-qualification training to diagnose and manage dementia [10] • Earlier diagnosis and treatment can be critical in delaying the onset of dementia [6] • Carers and other family members of people with dementia are often older and frail themselves, with high levels of depression, physical illness, and a diminished quality of life [11] • London is struggling to meet the needs of older black and minority ethnic Londoners who have dementia [10] Activity and Cost • Older people with dementia occupy 20% of acute hospital beds across England but 70% of these may be medically fit to be discharged [12] • 80% of people living in care homes have dementia or severe memory problems [13] • Estimated cost of dementia to the English economy is about £20 billion p/a • This is set to increase to over £27 billion by 2018 [14] • Delaying the on set of dementia by 5 years would reduce deaths directly attributable to dementia by 30,000 a year [13] 11 INTEGRATED CARE: THE KEY INGREDIENTS WHY POOR PATIENT EXPERIENCE Lack of independence and control Fragmented services that are difficult to navigate POOR OUTCOMES Poor quality of life for people and carers Too many people living with preventable ill-health and dying prematurely Avoidable emergency and residential care admissions/readmissions Unsafe transfers and transitions INCREASING DEMAND Aging Population Medical innovation Poor population health UNSUSTAINABLE MODELS OF CARE “30%” of people in hospital and care institutions who do not need to be there Insufficient prevention/early intervention Unrealised citizen and community capacity Limited primary care offer Limited community services Uneven quality across many services UNPRECEDENTED FINANCIAL CHALLENGE NHS – flat in real terms Local Government - 28% NHS in London expected to save £3.1bn by 2015 (15.5% of the national £20bn savings requirement) NHS nationally - £30bn funding gap by 2020 Financial system not fit for purpose, encouraging acute activity and costshunting WHAT GREATER INTEGRATION OF SERVICES AROUND THE PERSON Risk profiling Care coordination and care planning Integrated case management Single point of access 24/7 urgent response Admission avoidance and timely transfers of care Reablement A GREATER EMPHASIS ON SELF & HOME CARE Personal budgets Expert patient Carers strategy Technology for independence Support related Housing BUILDING COMMUNITY CAPACITY TO MANAGE DEMAND Early diagnosis Care navigators Mutual support Micro enterprises Information for all Population Health A NEW PRIMARY CARE OFFER Accessible Proactive Coordinated RECONFIGURATION OF ACUTE SERVICES Reduced activity in acute / realigned acute services HOW WHOLE HEALTH AND CARE SYSTEM LEADERSHIP Joint Governance Political alignment Joint Outcomes Joint public / patient engagement strategy 3-5 YEAR LOCAL PLANS signed off by Health and Wellbeing Boards LOCAL & CITY WIDE COHERENCE Acute Service reconfiguration SCALE / FOCUS Those at highest risk of needing urgent health and/or social care (adults and children) COMMISSIONING Alignment between LA/CCG/NHS England Engagement of providers Release of primary care commissioning to CCGs A WAY TO MOVE MONEY AROUND THE SYSTEM to address the perverse effects of activity-based payments. That might include: • contracting for populations and outcomes • Risk-sharing by commissioners and providers SHARED INFORMATION ACROSS AGENCY BOUNDARIES FLEXIBLE, ENGAGED WORKFORCE AND IMPROVED TRAINING TRANSPARENT MEASUREMENT OF OUTCOMES A DEVELOPING EVIDENCE BASE OUTCOMES IMPROVED CITIZEN EXPERIENCE People “in control and independent” IMPROVED HEALTH AND CARE OUTCOMES Enhanced quality and safety of services – to agreed standards IMPROVED SUSTAINABILITY OF THE HEALTH AND CARE SYSTEMS Increased investment in, quality of and productivity of primary and community services Large scale reduction in unplanned attendances, admissions to hospital and length of stay Reduction in admissions to residential Care EFFECTIVE DEMAND MANAGEMENT Management of demand at the front door of care and support services, The main aims & objectives of the Islington pioneer: ‘I want to be treated as a whole person and for you to recognise how disempowering being ill is’ ‘I want to have longer appointments with someone who is well prepared so that I do not have to tell my story again Care planning My goals / outcomes ‘I want my care to be coordinated and to have the same appointment systems across services’ ‘Better access to health care through social services and vice versa” ‘No clear systems and processes through all healthcare services’ Information ‘Person Centred Co-ordinated Care: The Islington Way’ ‘I want to feel supported by my community and get the most out of services available locally’ ‘I want to be listened to and be heard’ Communication Transitions Decision making ‘Helping people to help themselves’ Successful delivery from partnership working: COPD: NHS Innovation Challenge Prize 2013 ~ Integrated respiratory consultant across secondary & primary care Clinical leadership & support Incentivised GPs to proactively identify, diagnose & manage Supportive self-management Focus: Early diagnosis & management to prevent further illness & death Multi-disciplinary partnership: instrumental to introducing & promoting coordination & integration of COPD care Emphasis on self-care & lifestyle Focus on community assets Education in primary care Skill-building, networks & clinical champions OUTCOMES 25% increase in diagnosed prevalence between 2010 - 2013 93% increase in referrals to pulmonary rehabilitation between 2010-2012 72% of people on COPD register now have self management plan 16% decrease in emergency admissions in 2011/12 vs 2010/11 Plans for development: 2013/14 2014/15 2015/16 Service model Established population based community teams Single point of contact, reablement & rehabilitation Enhanced Care at home Self-care Motivational interview training/LT6 PAM scores facilitating targeted commissioning Systematic, supported selfmanagement based on need Prevention Closing the prevalence gap Utilisation of systematic care pathways Goal orientated personalised care plans Enablers Risk stratification tool Information governance /workforce development Linked & shared information / data Clear pathways of accountability: Clinical Leadership Supported by PMO approach Supported by UCLP Health & Wellbeing Board Chair: Leader of the Council. Members: Council, CCG, Healthwatch, Public Health, NHS England Rigour and challenge Patient Engagement Reporting arrangements Link to Making It Real Board Area specific workstreams (linking to four localities) Integrated Care Board Chair: CCG Vice-Chair. Members: patients, social care, Public Health, providers, UCLP, voluntary sector Area specific workstreams (linking to four localities) Working across North Central London (e.g. value based commissioning) Area specific workstreams (linking to four localities) Area specific workstreams (linking to four localities) Measures of success: When, and who, will assess impact? 1. Pilot 2. Project evaluation 3. Whole-system Interim reporting to HWBB & ICPB: provide challenge, rigour & development. Acknowledge we won’t get it all right first time - embed learning & iterative approach. What The whole pathway Total costs Quality & Experience Health outcomes Process Who Collaboration Patients and carers: coproduction Academic insight Frontline staff experience How Linked datasets Matched case-control Clearly defined intentions Qualitative & quantitative PMO Approach Opportunities and Challenges: Opportunities Challenges • • • • • • • • • • • • Collaboration – national & London Flexibility to trial new approaches Accelerated learning Increased pace of mobilisation Opportunity to apply academic rigor Whole system approach Strengthen collaborative leadership Participate in and inform the development of future models of care • Recognition and peer challenge • Permission to “do things differently” • Harnessing rich diversity of voluntary sector • • • • • Information governance IT resolution Revising contacting mechanisms Development of greater value based approach, with focus on outcome Models for workforce development Empowering people at population level to embrace behaviour change as a preventative strategy Provider capacity, capability & focus Understanding financial flow and impact Polarised demographic What are the important contextual factors: What help do we need? Contextual Factors Inequalities Whittington ICO UCLP Collaboration on value based commissioning Financial drivers Making prevention a reality for population Recognition & challenge Peer to peer learning Support & technical advice “Permission” to do things differently What we can offer? Ambition Commitment Track record Co-production Pooled budgets Information exchange Information governance PAM Work force development strategy How our plans can have a practical impact on the care of individuals? Aligning Education and Service Re-design in Primary Care Sanjiv Ahluwalia Head, London School of General Practice HENCEL Non-executive Primary Care GP, North London Challenges • • • • • • • Primary care workforce data Population need and workforce planning Workforce development and education needs Emerging service models Level of geography Changing workforce roles Centralisation versus localisation Potential solutions • Link population needs to workforce and education planning • Borough/CCG level information • Service commissioners and providers at the heart of this process • Future and current workforce needs • Multiprofessional and lay engagement • Locally owned with LETB facilitation Community Educational Provider Networks Ahluwalia et al (2013). Education for Primary Care Back to Dementia • Improve quality of care for the most vulnerable in our society • Empower and entrust our workforce to make the best possible decisions • Recognise the intimate relationship between quality and costs • System turbulence is a challenge but also an opportunity