Sustaining a Financially Vibrant Healthcare Organization
advertisement

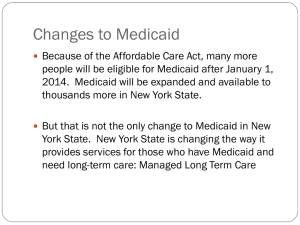
June 5, 2013 MS Healthcare Executives Summer Meeting Sustaining a Financially Vibrant Healthcare Organization Panelists • Moderator – Gwen Combs VP for Policy & General Counsel, Mississippi Hospital Association • Panelists Dr. Mark Williams, Chief Medical Officer North Mississippi Medical Center Chandler Ewing, CPA, FACHE, Chief Executive Officer Select Specialty Hospital – Jackson Kevin Gore, CPA, BKD National Health Care Group Reimbursement Drives the Delivery System In an economic impact study of hospitals, funded and published by the Mississippi Hospital Association in 2011, we learned that statewide our hospitals’ revenue streams break down as follows: • 43% Medicare • 16% Medicaid • 42% Private pay & uncompensated care Critical Care: The Economic Impact of Hospitals on the State’s Economy Reimbursement Drives the Delivery System Reimbursement Drives the Delivery System Changing how Medicare pays for inpatient acute care services: • Value-Based Purchasing • Reduction in Readmissions • No payment for Hospital Acquired Conditions • EHR Meaningful Use and other Information Technology Value-Based Purchasing Source: Triple-Tree.com Readmissions Reduction Source: 2007 MEDPAC report No Payments for HACs Source: The-Hospitalist.org By FFY 2015, hospitals will see reductions in payment, or no payment, for treatment of hospital acquired conditions. The newly proposed IPPS regulations from CMS indicate a 2% reduction in payment for those hospitals in the highest quartile for HACs. Reductions for Failure to Utilize EHR and IT By FFY 2015, hospitals that do not meet IQR requirements face a 2% reduction in reimbursement under newly proposed regulations. Reductions in Medicare DSH Source: Horne-LLP.com Financial Impact of ACA Medicare Reimbursement Reductions The Middle Class Tax Relief and Job Creation Act of 2012 authorized reduction to Medicare payments for reimbursable bad debts for all provider settings to 65%. Financial impact on Mississippi hospitals over 10 years is $37,001,400. The American Taxpayer Relief Act of 2012 authorized coding adjustment cuts for inpatient claims and for outpatient radiosurgery claims. Financial impact on Mississippi hospitals over 10 years is $123,512,800. CMS imposed a prospective coding adjustment of 1.9% for FFY 2013. This coding adjustment continues under newly proposed regulations. The financial impact on Mississippi hospitals is $246,752,400. Financial Impact of Reductions Medicaid • Under the Affordable Care Act, effective June 12, 2012, providers will no longer be paid for Hospital Acquired Conditions (HACs) or Provider Preventable Conditions (PPCs). • These are quarterly adjustments for Never Events that can be isolated from claims, such as: – Performance of wrong procedure on correct patient – Performance of procedure on patient not scheduled for surgery – Performance of correct procedure on wrong body part/side Medicaid • Under the Affordable Care Act, beginning in FFY 2014 (October 2013), Medicaid Disproportionate Share Hospital payments are to be phased down. • The federal DSH “pot” will be reduced each year as follows: – – – – 2014 2015 2016 2017 $500 million $600 million $600 million $1.8 billion 2018 $5 billion 2019 $5.6 billion 2020 $4.0 billion Medicaid • The application of the Medicaid DSH reductions must take into account the following: – The percentage of uninsured individuals in the State – Whether the State targets its DSH payments to hospitals with high uncompensated care – Whether the state is defined as a “low DSH state” (if so, the state faces a lower reduction) Other Medicaid Reimbursement Issues • Effective October 1, 2012, the Division of Medicaid implemented a new inpatient reimbursement system, APR-DRG, which, unlike the previous cost-based per diem, now pays for “stays” not “days.” • The object of this reimbursement methodology change is transparency in the care that Medicaid pays for. (In other words, Medicaid wants to pay for acuity of care rather than just having beds filled with Medicaid patients no matter the acuity of care.) Other Medicaid Reimbursement Issues • Effective September 1, 2012, the Division of Medicaid implemented an APC outpatient reimbursement methodology, replacing the historical cost-to-charge ratio and Medicare fee schedule methodology. • The new outpatient methodology uses Medicare rates, APC fees, and a state reimbursement fee schedule when no Medicare or APC rate exists. Medicaid Under the Affordable Care Act, effective January 1, 2013, primary care physician reimbursement will be at 100% of Medicare, the difference being paid by the federal government for 2 years. Medicare & Medicaid And don’t forget RACs, MACs, SMRCs, ZPIX, pre-payment reviews, utilization review, and prior authorization. Reasons for Denial of Claims • • • • • • Medical necessity 63% Incorrect MS-DRG or other coding error 26% Insufficient or no documentation in the medical record 3% All other 8% 85% of the medical necessity denials seem to center around the 1 day stay, leading auditors to conclude that the medically necessary care was delivered in the wrong setting. Do Commercial Insurance Payers Follow or Lead? • Is the Affordable Care Act a game changer in the delivery of health care services and the payment for them? • For 59% of the revenue streams for our hospitals, the answer is a resounding yes. • However, is not the commercial piece of the hospitals’ revenue stream using reimbursement to drive change in the delivery of health care as well? How do hospitals maintain their financial viability in the face of the revolution and evolution of payment for hospital care and health care? - Quality Initiatives - Business Model - Initiatives - Financial Initiatives