Top 10 papers in
geriatric psychiatry
Dr. Akshya Vasudev
November 2014
Disclosures
• No aid was received for composing or delivering this
presentation
• PI’s Research funding agencies have no conflict of interest with
this presentation. Current grants from
•
•
•
•
•
Academic Medical Organisation of Southwestern Ontario
Academic Development Fund, Western
Department of Psychiatry and Pediatrics, Western
Institute of Clinical Evaluative Sciences, Toronto
Schulich Research Opportunities Project
An exciting year as ever
• CIT-AD study
• No new drug for dementia!
• New ways of diagnosing Alzheimer’s : disturbance in olfactory
responses as well as retinal and lens changes in the eye.
Exercise is protective and is dose related. (AAIC 2014)
• Porsteinsson, A. P., et al. (2014). "Effect of citalopram on
agitation in Alzheimer disease: the CitAD randomized clinical
trial." Jama 311(7): 682-691
• MPORTANCE: Agitation is common, persistent, and associated with
adverse consequences for patients with Alzheimer disease.
Pharmacological treatment options, including antipsychotics are not
satisfactory.
• OBJECTIVE: The primary objective was to evaluate the efficacy of
citalopram for agitation in patients with Alzheimer disease. Key
secondary objectives examined effects of citalopram on function,
caregiver distress, safety, cognitive safety, and tolerability.
• DESIGN, SETTING, AND PARTICIPANTS: The Citalopram for Agitation in
Alzheimer Disease Study (CitAD) was a randomized, placebo-controlled,
double-blind, parallel group trial that enrolled 186 patients with
probable Alzheimer disease and clinically significant agitation from 8
academic centers in the United States and Canada from August 2009 to
January 2013.
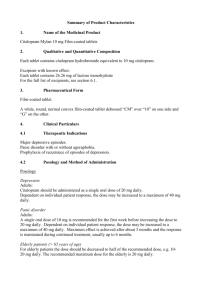
• INTERVENTIONS: Participants (n = 186) were randomized to receive a
psychosocial intervention plus either citalopram (n = 94) or placebo (n =
92) for 9 weeks. Dosage began at 10 mg per day with planned titration
to 30 mg per day over 3 weeks based on response and tolerability.
• MAIN OUTCOMES AND MEASURES: Primary outcome measures were based on
scores from the 18-point Neurobehavioral Rating Scale agitation subscale (NBRSA) and the modified Alzheimer Disease Cooperative Study-Clinical Global
Impression of Change (mADCS-CGIC). Other outcomes were based on scores
from the Cohen-Mansfield Agitation Inventory (CMAI) and the Neuropsychiatric
Inventory (NPI), ability to complete activities of daily living (ADLs), caregiver
distress, cognitive safety (based on scores from the 30-point Mini Mental State
Examination [MMSE]), and adverse events.
• RESULTS: Participants who received citalopram showed significant improvement
compared with those who received placebo on both primary outcome measures.
The NBRS-A estimated treatment difference at week 9 (citalopram minus
placebo) was -0.93 (95% CI, -1.80 to -0.06), P = .04. Results from the mADCSCGIC showed 40% of citalopram participants having moderate or marked
improvement from baseline compared with 26% of placebo recipients, with
estimated treatment effect (odds ratio [OR] of being at or better than a given
CGIC category) of 2.13 (95% CI, 1.23-3.69), P = .01. Participants who received
citalopram showed significant improvement on the CMAI, total NPI, and
caregiver distress scores but not on the NPI agitation subscale, ADLs, or in less
use of rescue lorazepam. Worsening of cognition (-1.05 points; 95% CI, -1.97 to 0.13; P = .03) and QT interval prolongation (18.1 ms; 95% CI, 6.1-30.1; P = .01)
were seen in the citalopram group.
• CONCLUSIONS AND RELEVANCE: Among patients with
probable Alzheimer disease and agitation who were receiving
psychosocial intervention, the addition of citalopram
compared with placebo significantly reduced agitation and
caregiver distress; however, cognitive and cardiac adverse
effects of citalopram may limit its practical application at the
dosage of 30 mg per day.
Objectives: Impaired insight into illness is a prevalent feature of
schizophrenia, which negatively influences treatment adherence
and clinical outcomes. Little is known about the effects of aging
on insight impairment. We aimed to review the available
research literature on the effects of aging on insight into illness
in schizophrenia, in relation to positive, negative, and cognitive
symptoms. Ultimately, we propose a trajectory of insight in
schizophrenia across the lifespan.
Method: A systematic Medline® literature search was
conducted, searching for English language studies describing the
relationship of insight into illness in schizophrenia with aging.
• Results: We identified 62 studies. Insight impairment is associated
with illness severity, premorbid intellectual function (i.e. IQ),
executive function, and memory. Insight impairment improves
modestly during midlife, worsening again in late life. It tends to
fluctuate with each episode of psychosis, likely in relation to
worsening positive symptoms that improve with antipsychotic
treatment. The relationship between insight impairment and
cognitive dysfunction appears to attenuate with age, while the
relationship with lower premorbid intellectual function is preserved.
The association between impaired insight and negative symptoms is
unclear.
• Conclusions: The available literature suggests that the course of
insight impairment follows a U-shaped curve, where insight
impairment is severe during the first episode of psychosis, modestly
improves over midlife, and declines again in late life. Future studies
are required to investigate the trajectory of insight into illness and
its core domains across the lifespan from prodromal phase to late
life.
B vitamins to enhance treatment response to
antidepressants in middle-aged and older
adults: results from the B-VITAGE
randomised, double-blind, placebo-controlled
trial
Osvaldo P. Almeida, Andrew H. Ford, Varsha Hirani, Vash Singh,
Frank M. vanBockxmeer, Kieran McCaul, and Leon Flicker
BJP bjp.bp.114.145177; published ahead of print September
25, 2014,
• Background: Depression is common and the efficacy of
antidepressants is suboptimal. High plasma homocysteine has been
consistently associated with depression, and treatment with certain
B vitamins demonstrably reduces its concentration.
• Aims: To determine whether vitamins B6, B12 and folic acid enhance
response to antidepressant treatment over 52 weeks.
• Method: Randomised, double-blind, placebo-controlled trial of
citalopram (20-40 g) together with 0.5 mg of vitamin B12, 2 mg of
folic acid and 25 mg of vitamin B6 for 52 weeks. Participants were
community-dwelling adults aged 50 years or over with DSM-IV-TR
major depression.. The primary outcome was remission of the
depressive episode after 12, 26 and 52 weeks. Secondary outcomes
included reduction of MADRS scores over time and relapse of major
depression after recovery by week 12.
• Results: In total, 153 people were randomised (76 placebo, 77
vitamins. Remission of symptoms was achieved by 78.1 and 79.4% of
participants treated with placebo and vitamins by week 12 (P =
0.840), by 76.5 and 85.3% at week 26 and 75.8 and 85.5% at week
52 (effect of intervention over 52 weeks: odds ratio (OR) = 2.49, 95%
CI 1.12-5.51). Group differences in MADRS scores over time were
not significant (P = 0.739). The risk of subsequent relapse among
those who had achieved remission of symptoms at week 12 was
lower in the vitamins than placebo group (OR = 0.33, 95% CI 0.120.94).
• Conclusions: B vitamins did not increase the 12-week efficacy of
antidepressant treatment, but enhanced and sustained
antidepressant response over 1 year. Replication of these findings
would mandate that treatment guidelines adopt the adjunctive use
of B vitamins as a safe and inexpensive strategy to manage major
depression in middle-aged and older adults.
• Disabato, B. M., et al. (2014). "Comparison of Brain Structural
Variables, Neuropsychological Factors, and Treatment
Outcome in Early-Onset Versus Late-Onset Late-Life
Depression." The American Journal of Geriatric Psychiatry
22(10): 1039-1046.
• Objective: To compare differences in gray matter volumes,
white matter and subcortical gray matter hyperintensities,
neuropsychological factors, and treatment outcome between
early- and late-onset late-life depressed (LLD) subjects.
• Methods: We conducted a prospective, nonrandomized,
controlled trial at the outpatient clinics at Washington
University and Duke University on 126 subjects, aged 60 years
or older, who met Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition criteria for major depression, scored
20 or more on the Montgomery-Asberg Depression Rating
Scale (MADRS), and received neuropsychological testing and
magnetic resonance imaging. Subjects were excluded for
cognitive impairment or severe medical disorders. After 12
weeks of sertraline treatment, subjects' MADRS scores over
time and neuropsychological factors were studied.
• Results: Left anterior cingulate thickness was significantly
smaller in the late-onset depressed group than in the earlyonset LLD subjects. The late-onset group also had more
hyperintensities than the early-onset LLD subjects. No
differences were found in neuropsychological factor scores or
treatment outcome between early-onset and late-onset LLD
subjects.
• Conclusion: Age at onset of depressive symptoms in LLD
subjects are associated with differences in cortical thickness
and white matter and subcortical gray matter hyperintensities,
but age at onset did not affect neuropsychological factors or
treatment outcome.
• Mulsant, B. H., et al. (2014). "A systematic approach to
pharmacotherapy for geriatric major depression." Clin Geriatr
Med 30(3): 517-534.
• The broadening use of antidepressants among older
Americans has not been associated with a notable decrease in
the burden of geriatric depression. This article, based on a
selective review of the literature, explores several
explanations for this paradox. The authors propose that the
effectiveness of antidepressants depends in large part on the
way they are used. Evidence supports that antidepressant
pharmacotherapy leads to better outcomes when guided by a
treatment algorithm as opposed to attempting to individualize
treatment. Several published guidelines and pharmacotherapy
algorithms developed for the treatment of geriatric
depression are reviewed, and an updated algorithm proposed.
• Background: There are conflicting results on the impact of anxiety
on depression outcomes. The impact of anxiety has not been
studied in major depression with psychotic features (“psychotic
depression”).
Aims: We assessed the impact of specific anxiety symptoms and
disorders on the outcomes of psychotic depression.
Methods: We analyzed data from the Study of Pharmacotherapy for
Psychotic Depression that randomized 259 younger and older
participants to either olanzapine plus placebo or olanzapine plus
sertraline. We assessed the impact of specific anxiety symptoms
from the Brief Psychiatric Rating Scale (“tension”, “anxiety” and
“somatic concerns” and a composite anxiety score) and diagnoses
(panic disorder and GAD) on psychotic depression outcomes using
linear or logistic regression. Age, gender, education and
benzodiazepine use (at baseline and end) were included as
covariates.
• Results: Anxiety symptoms at baseline and anxiety disorder
diagnoses differentially impacted outcomes. On adjusted linear
regression there was an association between improvement in
depressive symptoms and both baseline “tension” (coefficient =
0.784; 95% CI: 0.169–1.400; p = 0.013) and the composite anxiety
score (regression coefficient = 0.348; 95% CI: 0.064–0.632; p =
0.017). There was an interaction between “tension” and treatment
group, with better responses in those randomized to combination
treatment if they had high baseline anxiety scores (coefficient =
1.309; 95% CI: 0.105–2.514; p = 0.033). In contrast, panic disorder
was associated with worse clinical outcomes (coefficient = −3.858;
95% CI: –7.281 to −0.434; p = 0.027) regardless of treatment.
• Conclusions: Our results suggest that analysis of the impact of
anxiety on depression outcome needs to differentiate psychic and
somatic symptoms.
• Gerhard, T., et al. (2014). "Comparative mortality risks of
antipsychotic medications in community-dwelling older
adults." Br J Psychiatry 205(1): 44-51.
• BACKGROUND: All antipsychotic medications carry warnings of
increased mortality for older adults, but little is known about
comparative mortality risks between individual agents. AIMS:
To estimate the comparative mortality risks of commonly
prescribed antipsychotic agents in older people living in the
community. METHOD: A retrospective, claims-based cohort
study was conducted of people over 65 years old living in the
community who had been newly prescribed risperidone,
olanzapine, quetiapine, haloperidol, aripiprazole or
ziprasidone (n = 136 393). Propensity score-adjusted Cox
proportional hazards models assessed the 180-day mortality
risk of each antipsychotic compared with risperidone.
• RESULTS: Risperidone, olanzapine and haloperidol showed a
dose-response relation in mortality risk. After controlling for
propensity score and dose, mortality risk was found to be
increased for haloperidol (hazard ratio (HR) = 1.18, 95% CI
1.06-1.33) and decreased for quetiapine (HR = 0.81, 95% CI
0.73-0.89) and olanzapine (HR = 0.82, 95% CI 0.74-0.90).
CONCLUSIONS: Significant variation in mortality risk across
commonly prescribed antipsychotics suggests that
antipsychotic selection and dosing may affect survival of older
people living in the community.
• Gildengers, A. G., et al. (2014). "Longer lithium exposure is
associated with better white matter integrity in older adults
with bipolar disorder." Bipolar Disorders
• OBJECTIVES: Bipolar disorder (BD) is associated with cognitive
dysfunction and structural brain abnormalities. In human and
non-human studies, lithium has been related to
neuroprotective and neurotrophic effects. We explored
whether lithium treatment is related to better brain integrity
and cognitive function in older adults with BD.
• METHODS: We examined cognitive and neuroimaging data in
58 individuals with BD [mean (standard deviation) age = 64.5
(9.8) years] and 21 mentally healthy comparators (controls) of
similar age and education. Subjects received comprehensive
neurocognitive assessment and structural brain imaging,
examining total gray matter volume, overall white matter
integrity (fractional anisotropy), and total white matter
hyperintensity burden.
• RESULTS: In comparison to controls, subjects with BD had
worse overall cognitive performance, lower total gray matter
volume, and lower white matter integrity. Among subjects
with BD, longer duration of lithium treatment was related to
higher white matter integrity after controlling for age and
vascular disease burden, but not with better cognitive
performance.
• CONCLUSIONS: Lithium treatment appears to be related to
better brain integrity in older individuals with BD, in particular,
in those who take lithium long-term. While intriguing, these
findings need to be confirmed in a larger sample.
• Kryscio, R. J., et al. (2014). "Self-reported memory complaints:
Implications from a longitudinal cohort with autopsies."
Neurology.
• Objective: We assessed salience of subjective memory
complaints (SMCs) by older individuals as a predictor of
subsequent cognitive impairment while accounting for risk
factors and eventual neuropathologies.
• Methods: Subjects (n = 531) enrolled while cognitively intact
at the University of Kentucky were asked annually if they
perceived changes in memory since their last visit. A
multistate model estimated when transition to impairment
occurred while adjusting for intervening death. Risk factors
affecting the timing and probability of an impairment were
identified. The association between SMCs and Alzheimer-type
neuropathology was assessed from autopsies (n = 243).
• Results: SMCs were reported by more than half (55.7%) of the
cohort, and were associated with increased risk of impairment
(unadjusted odds ratio = 2.8, p < 0.0001). Mild cognitive impairment
(dementia) occurred 9.2 (12.1) years after SMC. Multistate modeling
showed that SMC reporters with an APOE ε4 allele had double the
odds of impairment (adjusted odds ratio = 2.2, p = 0.036). SMC
smokers took less time to transition to mild cognitive impairment,
while SMC hormone-replaced women took longer to transition
directly to dementia. Among participants (n = 176) who died without
a diagnosed clinical impairment, SMCs were associated with
elevated neuritic amyloid plaques in the neocortex and medial
temporal lobe.
• Conclusion: SMC reporters are at a higher risk of future cognitive
impairment and have higher levels of Alzheimer-type brain
pathology even when impairment does not occur. As potential
harbingers of future cognitive decline, physicians should query and
monitor SMCs from their older patients.
• Kuźma, E., et al. "History of Alcohol Use Disorders and Risk of
Severe Cognitive Impairment: A 19-Year Prospective Cohort
Study." The American Journal of Geriatric Psychiatry 22(10):
1047-1054.
• OBJECTIVE: To assess the effects of a history of alcohol use disorders
(AUDs) on risk of severe cognitive and memory impairment in later
life.
• METHODS: We studied the association between history of AUDs and
the onset of severe cognitive and memory impairment in 6,542
middle-aged adults born 1931 through 1941 who participated in the
Health and Retirement Study, a prospective nationally
representative U.S. cohort. Participants were assessed at 1992
baseline and follow-up cognitive assessments were conducted
biannually from 1996 through 2010. History of AUDs was identified
using the three-item modified CAGE questionnaire. Cognitive
outcomes were assessed using the 35-item modified Telephone
Interview for Cognitive Status at last follow-up with incident severe
cognitive impairment defined as a score </=8, and incident severe
memory impairment defined as a score </=1 on a 20-item memory
subscale.
• RESULTS: During up to 19 years of follow-up (mean: 16.7
years, standard deviation: 3.0, range: 3.5-19.1 years), 90
participants experienced severe cognitive impairment and 74
participants experienced severe memory impairment. History
of AUDs more than doubled the odds of severe memory
impairment (odds ratio [OR] = 2.21, 95% confidence interval
[CI] = 1.27-3.85, t = 2.88, df = 52, p = 0.01). The association
with severe cognitive impairment was statistically nonsignificant but in the same direction (OR = 1.80, 95% CI = 0.973.33, t = 1.92, df = 52, p = 0.06).
• CONCLUSION: Middle-aged adults with a history of AUDs have
increased odds of developing severe memory impairment
later in life. These results reinforce the need to consider the
relationship between alcohol consumption and cognition from
a multifactorial lifespan perspective.
• Lopez, O. L., et al. (2014). "Amyloid, neurodegeneration, and
small vessel disease as predictors of dementia in the oldestold." Neurology.
• Objective: To examine the association between brain
structural changes and β-amyloid deposition, and incident
dementia in 183 elderly subjects without dementia (mean age
85.5 years) 2 years later.
• Methods: Subjects had a brain structural MRI scan and a PET
scan with 11C-labeled Pittsburgh compound B (PiB) in 2009,
and were evaluated clinically in 2011.
• Results: At baseline evaluation, of the 183 participants (146 cognitively normal
[CN]); 37 mild cognitive impairment [MCI]), 139 (76%) were PiB+, had small
hippocampal volume (<25th percentile), or had high white matter lesion (WML)
volume (>75th percentile). Two years later, 111 (61%) were classified as CN, 51
(28%) as MCI, and 21 (11%) as dementia. At baseline, 51% of the CN participants
and 67.5% of the MCI cases were PiB+. Thirty percent of the CN and 51% of the
MCI cases had small hippocampi, and 24% of the CN and 40.5% of the MCI cases
had abnormal WMLs. Of the 21 participants who progressed to dementia, 20
(95%) had at least one imaging abnormality. Only 3 (14%) were only PiB+, 1 (5%)
had only small hippocampi, 1 (5%) had only WMLs, 1 (5%) was biomarker
negative, and the other 16 had various pairs of imaging abnormalities.
Continuous variables of PiB retention, left and right hippocampal volume, and
WML volume were independent predictors of dementia in a logistic regression
analysis controlling for age, sex, education level, and Mini-Mental State
Examination scores.
• Conclusions: The prevalence of β-amyloid deposition, neurodegeneration (i.e.,
hippocampal atrophy), and small vessel disease (WMLs) is high in CN older
individuals and in MCI. A combination of 2 or 3 of these factors is a powerful
predictor of short-term incidence of dementia.
• Rej, S., et al. "Prevalence and Correlates of Renal Disease in
Older Lithium Users: A Population-Based Study." The
American Journal of Geriatric Psychiatry 22(11): 1075-1082.
• OBJECTIVE: Lithium is an important treatment for mood disorders,
but concern about its association with renal disease has contributed
to its limited use, particularly in older adults. Because high-quality
evidence examining renal disease in this population is lacking, this
study aims to quantify the prevalence and identify clinical correlates
of renal disease in geriatric lithium users.
• METHODS: In a population-based cross-sectional study on 2,480
lithium users aged 70 or more years, the authors searched the
provincial administrative health data from Ontario, Canada between
April 1, 2005 and March 31, 2011. Prevalence of chronic kidney
disease (CKD), acute kidney injury (AKI), and nephrogenic diabetes
insipidus (NDI) was measured using International Classification of
Diseases, Tenth Revision codes. Logistic regression analyses were
used to identify independent correlates of renal disease.
• RESULTS: The 6-year prevalence rates of CKD, AKI, and NDI were
13.9%, 1.3%, and 3.0%, respectively. Hypertension (odds ratio [OR]:
2.05; 95% confidence interval [CI]: 1.50-2.79), diabetes mellitus (OR:
1.86; 95% CI: 1.45-2.38), ischemic heart disease (OR: 1.65; 95% CI:
1.24-2.20), NDI (OR: 2.54; 95% CI: 1.47-4.40), AKI (OR: 11.7; 95% CI:
5.26-26.1), lithium use for more than 2 years (OR: 1.71; 95% CI: 1.052.81), loop diuretic use (OR: 1.74; 95% CI: 1.26-2.41),
hydrochlorothiazide use (OR: 1.48; 95% CI: 1.07-2.05), and atypical
antipsychotic use (OR: 1.49; 95% CI: 1.17-1.89) were all
independently associated with CKD.
• CONCLUSION: Older lithium users have high rates of CKD. Lithium
use duration was independently associated with CKD. Longitudinal
studies including individuals without lithium exposure will be
necessary to confirm whether lithium is indeed a risk factor for CKD
in older adults.
• Robinson, M., et al. (2014). "Acute and Long-term Treatment
of Late-Life Major Depressive Disorder: Duloxetine Versus
Placebo." The American Journal of Geriatric Psychiatry 22(1):
34-45.
• Objective: To compare the efficacy of duloxetine with placebo on
depression in elderly patients with major depressive disorder.
• Design: Multicenter, 24-week (12-week short-term and 12-week
continuation), randomized, placebo-controlled, double-blind trial.
Setting United States, France, Mexico, Puerto Rico. Participants Age
65 years or more with major depressive disorder diagnosis (one or
more previous episode); Mini-Mental State Examination score ≥20;
Montgomery-Asberg Depression Rating Scale total score ≥20.
Intervention Duloxetine 60 or 120 mg/day or placebo; placebo
rescue possible. Measurements Primary-Maier subscale of the 17item Hamilton Depression Rating Scale (HAMD-17) at week 12.
Secondary-Geriatric Depression Scale, HAMD-17 total score,
cognitive measures, Brief Pain Inventory (BPI), Numeric Rating Scales
(NRS) for pain, Clinical Global Impression-Severity scale, Patient
Global Impression of Improvement in acute phase and acute plus
continuation phase of treatment.
• Results: Compared with placebo, duloxetine did not show
significantly greater improvement from baseline on Maier subscale
at 12 weeks, but did show significantly greater improvement at
weeks 4, 8, 16, and 20. Similar patterns for Geriatric Depression
Scale and Clinical Global Impression-Severity scale emerged, with
significance also seen at week 24. There was a significant treatment
effect for all BPI items and 4 of 6 NRS pain measures in the acute
phase, most BPI items and half of the NRS measures in the
continuation phase. More duloxetine-treated patients completed
the study (63% versus 55%). A significantly higher percentage of
duloxetine-treated patients versus placebo discontinued due to
adverse event (15.3% versus 5.8%).
• Conclusions: Although the antidepressant efficacy of duloxetine was
not confirmed by the primary outcome, several secondary measures
at multiple time points suggested efficacy. Duloxetine had significant
and meaningful beneficial effects on pain.
• Sampson, E. L., et al. (2014). "Behavioural and psychiatric
symptoms in people with dementia admitted to the acute
hospital: prospective cohort study." Br J Psychiatry 205(3):
189-196.
• Background: Dementia is common in older people admitted to
acute hospitals. There are concerns about the quality of care
they receive. Behavioural and psychiatric symptoms of
dementia (BPSD) seem to be particularly challenging for
hospital staff.
• Aims: To define the prevalence of BPSD and explore their
clinical associations.
• Method: Longitudinal cohort study of 230 people with
dementia, aged over 70, admitted to hospital for acute
medical illness, and assessed for BPSD at admission and every
4 (+/- 1) days until discharge. Other measures included length
of stay, care quality indicators, adverse events and mortality.
• Results: Participants were very impaired; 46% at Functional
Assessment Staging Scale (FAST) stage 6d or above (doubly
incontinent), 75% had BPSD, and 43% had some BPSD that
were moderately/severely troubling to staff. Most common
were aggression (57%), activity disturbance (44%), sleep
disturbance (42%) and anxiety (35%).
• Conclusions: We found that BPSD are very common in older
people admitted to an acute hospital. Patients and staff would
benefit from more specialist psychiatric support.