10 year Follow-up - Affinity Health System
advertisement

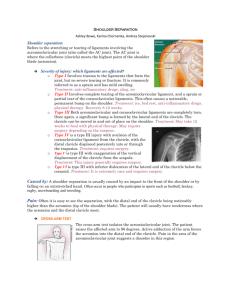
June 11, 2013 Joseph C McCormick III, MD Orthopaedic Surgeon Affinity Medical Group Disclosure Slide • Nothing to disclose in terms of financial or industry relationship. Goals • Review anatomy of acromioclavicular joint • Mechanism of injury • Classification of acromioclavicular injuries • Define treatment based on grade • Review of clinical outcomes and biomechanical literature regarding AC Injury History • Hippocrates first to distinguish AC injuries from GH joint injuries and to delineate the mechanism of injury – “Physicians are particularly liable to be deceived in this accident, so that they may prepare as if for dislocation of the shoulder;…” History • Galen diagnosed his own AC dislocation sustained while wrestling • Treated himself as Hippocrates suggested with tight bandages to hold clavicle down with arm elevated • Abandoned this treatment after a few days because it was so uncomfortable • Hippocrates felt that no “impediment, great or small will result from such an injury” • Furthermore he stated the deformity cannot be restored to its “natural situation” • This statement has been received by the ortho community over the years as a challenge. • First reported surgical procedure for AC dislocation by Cooper in 1861 Anatomy Diarthrodial joint Has fibrocartilaginous disk Clavicle rotates with external rot and abduction AC ligaments stabilize in AP direction, insert on clavicle 1.5 cm from joint – superior and posterior fibers most robust CC ligaments – predominant restraint to vertical translation Anatomy Coraco-clavicular Interval: average 1.1 - 1.3 cm Trapezoid: attaches anterior and lateral on clavicle Average distance distal clavicle to center 2.54 cm males/ 2.29 cm females Conoid: attaches posterior and medial on clavicle Larger of the 2 CC ligmaments Next ligament to fail after AC ligament disruption Ave distance distal clavicle to medial aspect of conoid tuberosity 4.72 cm males/ 4.28 cm females OKU 4 Sports Medicine Dynamic stabilizers Muscles that cross joint important to stability Anterior deltoid helps to suspend arm from clavicle attachment Trapezius has confluent fascial attachment over dorsum of acromion Importance noted in the higher grades of injury, i.e.. Type V Mechanism Direct vs. Indirect Direct by far most common Direct force to acromion with the shoulder adducted, usually result of fall Acromion moves inferiorly and medially while clavicle is stabilized by the SC joint ligaments Force results in systematic failure of stabilizing structures as it propagates AC ligaments/capsule CC ligaments deltotrapezial fascia Indirect is more rare results from fall onto outstretched hand/arm with superiorly directed force typically affect AC ligaments only Diagnosis During exam should be sitting or standing w/o support for the injured arm Check for tenderness to palpation at the AC joint and the CC interspace If patient can tolerate check joint for stability Check to see if reducible Examine SC joint as well Neurologic exam to r/o brachial plexus injury Radiographs AP, axillary lateral and Zanca views can be taken to best assess the joint Should be taken with the patient upright and no support of injured arm Stress views ?? Stress Radiographs ? ASES Survey 81% Not in ER 91% No change in Treatment Stress views are costly, painful, and don’t often provide new info, so aren’t routinely used anymore Radiographs Zanca View Underpenetrated view 10-15 degree cephalic tilt Axillary View Assess horizontal displacement Biplanar Instability/Displacement Vertical Horizontal Dynamic Axillary View Tauber et al AJSM 2010 Gleno-acromio-clavicular angle May help detect previously missed horizontally unstable injuries. Classification Originally described by Tossy and Allman in the 1960’s Included types I,II, and III In 1984, classification modified by Rockwood Now types IV, V, and VI added, better predictor of prognosis, need for surgical intervention Type I No visible deformity Swelling/pain over AC joint No pain over CC interspace Radiographs appear normal Type II AC ligaments disrupted Horizontally unstable Absent or very minimal vertical instability Tenderness over CC interspace Abnormal radiographs Type III Horizontal and vertical instability Radiographically AC joint is dislocated Pain in CC interspace Typically pain is greater with Type III and higher injury Historically more debate with choice of treatment Type IV AC joint dislocation Clavicle displaced posteriorly AC joint irreducible on exam Occasionally associated with SC dislocation Type IV Type V All stabilizing ligaments disrupted Deltoid and trapezius muscles and fascia at least partially detached from clavicle AC joint irreducible May develop symptoms due to brachial plexus traction Type V Type VI High energy variant Result of hyperabduction and external rotation Distal clavicle comes to rest in subcoracoid position Summary Treatment I and II Nonsurgical management is uniformly recommended for type I and II injuries A period of immobilization in a sling for comfort until pain subsides Usually 7-10 days for type I, up to 2 weeks for type II Possible anesthetic injection for return to high level play Unloading foam padding Once acute pain has subsided rehabilitation program is instituted Not So Benign? Mouhsine et al JSES 2003 33 patients Grade I and II injuries treated conservatively 27% required surgery within 36 months (6 distal clavicle excision, 3 Weaver-Dunn) 24 pts remaining assessed 6 yrs post injury both clinically and radiographically Only 16% patients with no radiographic degenerative changes or osteolysis evident Not So Benign? Mikek AJSM 2008 23 patients with Type I and II AC Disruption with 10 year Follow-up 52% reported occasional symptoms Constant score 70.5 injured vs 86.8 (P < .001) UCLA score 24.1 vs 29.2 (P < .001) Simple Shoulder Test 9.7 vs 10.9 (P < .002) Rehabilitation Early focus is on passive and active ROM Once symmetric and painless ROM achieved then progress to isometric shoulder strengthening Isotonic strengthening is next with gradual escalation of strength and endurance with return to sport in mind Return to sport is not allowed until painless/full ROM is achieved and strength has returned. This may take longer for type II injuries, and some recommend contact sports/heavy lifting should be avoided for 2-3 months What about Type III injuries? Type III injuries In 1974 Powers and Bach reported that 92% of 116 type III injuries were treated operatively Of 163 ortho residency program chairmen surveyed at that time 91.5% advocated surgical treatment In 1992 Cox surveyed 231 chairmen and 62 orthopedists participating in care of athletes 72% of chairmen favored non-op management 86% of team orthopedists favored no-op management trend toward non-surgical management is well supported in the literature Natural History of Type III Schlegel et al AJSM 2001 Prospective study non-operative treatment of 20 patients with Type III AC injuries assessed strength, ROM, subjective questionnaire Ave Sling use: 8 days (2-25) Ave return to work: 9 days (1-24) 7 professionals, 8 laborers, 2 students, 3 unemployed/retired Analgesic discontinued: 1 wk (15); 2 wk (5) Natural History of Type III Schlegel et al 1 year results All had full, pain free, symmetric ROM No statistical difference in dynamometer strength A statistically significant 17% decrease in bench press strength on injured side was noted 80% favorable subjective results 20% unfavorable 3 of 4 secondary gain bias Only 1 of 4 elected to undergo surgical intervention Non-op management Galpin et al 1984, retrospective review comparing outcome in type III injuries, 21 treated non-op, 16 with surgery (Bosworth screw and ligament repair) avg 3 yr f/u Showed overall chances of late pain or altered function were not statistically different Surgical patients took longer to become pain free, and longer to return to work 2.8 vs. 4.5 months, and 2.6 vs. 6.8 weeks, respectively Numbers were limited to correlate treatment with patient demands Glick et al 1977, retrospective review of 35 AC dislocations treated non-operatively. 29/35 had no pain, none had disabling pain, 31/35 had no weakness, none had disabling weakness None of the patients who had supervised rehabilitation complained 8/10 throwers were not affected while throwing, two were professional quarterbacks and one a collegiate javelin thrower Concluded that complete reduction not necessary for satisfactory function Randomized prospective trial Bannister et al 1989 – 60 patients with acute AC dislocations random number drawn to allocate operative vs. no-op treatment Faster return to work for manual and clerical workers treated nonoperatively After 4 years of f/u no real difference between the two groups in terms of pain/function with one exception In the 12 dislocations with more severe dislocation, i.e.. Type V, surgery gave better results Concluded that younger patients with severe displacement are more likely to achieve an excellent result if stabilized early Felt that surgical treatment created greater morbidity in the lesser grades of injury Slight strength loss? Wojtys et al, 1989, retrospective review of 22 patients with type III treated non-operatively Showed that laborers and athletes can recover strength and endurance, return to pre-injury level of activity without surgery Strength testing showed some statistically insignificant strength loss, indicating that the strength and endurance advantage one might expect of the dominant arm may be lessened or lost May be a factor to consider for those requiring high levels of shoulder strength for work/athletics, or those involved in highly repetitious endurance activities such as swimming/pitching Rarity of type III AC separation precludes study of significant numbers with controls to determine treatment that is best for athletes who rely on their elite throwing ability McFarland MLB Survey Study 1997 American Journal of Orthopedics, Nov 1997 Phillips et. al CORR 1998 Meta-analysis Type III AC Injury Pain absent or minimal ROM normal/near normal Strength normal /near normal Subsequent surgery OP 93% 86% 87% 59% vs NON-OP 95% 95% 91% 6% Operative results and Timing Weinstein et al AJSM 1995 44 patients Type III Injury 27 acute, 17 late repairs CC nonabsorbable suture repair/recon 15/27 and 17/17 CA transfer 89% satisfactory results, 93% return to sports Timing Acute (<3 wk) vs Late (> 3wk) Satisfactory results 96% vs 77% Loss of reduction 15% vs 29% Types IV, V, IV All require operative intervention All stabilizers, static and dynamic are injured Treatment Old School Not well tolerated, Dermal Complications Surgical management Fixation across AC joint Fixation between coracoid and clavicle Ligament reconstruction Distal clavicle excision Acromioclavicular Fixation Pin fixation Has been abandoned since reports of rare pin migration Heart, Lung, Great vessels Acromioclavicular fixation Hook Plate Only used for acute injury Requires subsequent surgery for removal Fixation between coracoid and clavicle Bosworth popularized the use of a screw for fixation of the clavicle to the coracoid This technique initially did not include recommendation for repair or reconstruction of the CC ligaments Today the use of screws and suture loops has been described alone and in combo with ligament reconstruction Placement of synthetic loops between the coracoid and clavicle can be done arthroscopically, main advantage: doesn’t require staged screw removal Ligament reconstruction Weaver and Dunn were the 1st to describe transfer for the native CA ligament to reestablish AC joint stability Their technique described excision of the distal clavicle with this ligament transfer Construct can be augmented with a suture loop for protection until the transferred ligament heals Ligament Reconstruction orthoillustrated.com Open and Arthroscopic techniques Restore Anatomy Anatomic Ligament Reconstruction Alternative technique is use of semitendinosus autograft for reconstruction Loop around or fix into coracoid, then fix through two separate clavicle bone tunnels to approximate normal anatomic location of CC ligaments Recent biomechanical studies have demonstrated the superiority of this construct Biomechanical studies Lee et al., 2003 – 11 cadaveric shoulders tensile tested to failure comparing suture loop, CA transfer, and free tendon recon Reconstructions found to have failure strengths as strong as those of native CC ligaments CA transfer was the weakest construct, and shows that greatest elongation at failure Concluded tendon graft reconstruction to be an alternative to CA lig transfer possibly providing a permanent biologic reconstruction Given its biomechanical properties similar to native CC ligaments, reconstruction with tendon graft may allow for shorter post op immobilization and accelerated rehab program Biomechanical studies Mazzocca et al, 2006, studied 42 cadaveric specimens comparing stability of 3 AC joint reconstruction techniques Anatomic CC reconstruction with tendon graft provided ant, post, and superior stability similar to intact state Modified Weaver-Dunn had significantly greater laxity compared to anatomic CC recon and arthroscopic reconstruction Concluded that anatomic reconstruction with free tendon graft may provide stronger, more permanent biologic solution for AC joint dislocation Newer proposed techniques Grutter and Petersen 2005 AJSM (Cadaveric study) Anatomic Reconstruction using FCR graft to reconstruct CC and superior AC ligament Similar strength as native AC joint in coronal plane Newer Proposed Techniques Freedman et al AJSM 2010 (Cadaveric study) Intramedullary AC reconstruction with 5 cm semitendinosus graft and fibertape AP translation Intact: 2.34 - 7.86 mm Recon: 1.20 - 2.95 mm Superior/Inferior translation Intact: 2.56 - 6.16 mm Recon: 2.42 - 4.57 mm Did not reproduce similar stiffness, load to failure, and energy absorption as intact AC complex Newer proposed techniques AJSM 2010 Improved horizontal stability with addition of intramedullary AC ligament reconstruction. -50% less AP translation No difference in: - Superior/inferior translation - Load to failure Complications Non operative Pain Post traumatic arthritis/osteolysis Possible neurologic injury Possible strength deficit Surgical Same as above plus… Clavicle or coracoid fracture Loss of reduction Pneumothorax Neurovascular injury Summary Type I, II restricted activity initially Analgesic, Injection Rehabilitation Type III Controversial- trends toward initial non-operative management Late reconstruction if symptomatic Optimal strategy has changed and alternated over time Type IV,V, VI Repair/reconstruction Case HPI: 21 yo R HD male college student presents to clinic after fell off bike over the handle bars onto his R shoulder Exam: Ecchymosis, Gross deformity R AC joint TTP distal clavicle and CC interspace Distally NVI R upper extremity Radiographs Post op Acute CC repair with Fiberwire Suture Loops References • Bannister, G, Wallace, W, Stableforth, P.G.: The Management f Acute Acromioclavicular Dislocation. JBJS(Br) 1989; 71-B:848 -50 • Galpin, R, Hawkins, R, Grainger, R: A Comparative Analysis of Operative Versus Nonoperative Treatment of Grade III Acromioclavicular Separations. CORR 1985;193:150-155 • Glick, J, Milburn, L, Haggerty, J, et al: Dislocated acromioclavicular joint. Follow-up study of 35 unreduced acromioclavicular dislocations. Am J Sports Med 1977;5: 264270 • Lemos, M: The Evaluation and Treatment of the Injured Acromioclavicular Joint in Athletes. Am J Sports Med 1998;26:137-144 • Lee, S, Nicholas, S, Akizui, K, et al: Reconstruction of the Coracoclavicular Ligaments with Tendon Grafts. Am J Sports Med 2003;31:648-654 • Mazzocca, A, Santangelo, S, Johnson, S, et al: A Biomechanical Evaluation of an Anatomical Coracoclavicular Ligament Reconstruction. Am J Sports Med 2006;34:236246 • McFarland, EG, Blivin, SJ, Doehring, CB, et al: Treatment of Grade III Acromioclavicular Separations in Professional Throwing Athletes. Am J Orthop 1997;11:771-774 • Simovitch, R, Sander, B, Lavery, K, et al: Acromioclavicular Joint Injuries: Diagnosis and Management. JAAOS 2009;17:207-219 • Wojtys, E, Nelson, G: Conservative Treatment of Grade III Acromioclavicular Dislocations. CORR 1991;268:112-119 • Galatz, L, Williams, G: Acromioclavicular Joint Injuries. Rockwood and Green’s Fractures in Adults, 5th ed. 2002;1210-1244 • Mazzocca, A. Arciero , R . Evaluation and Treatment of Acromioclavicular Joint Injuries. Am J Sports Med 2007 35: 316 • Grutter, P. Petersen, S. Anatomical Acromioclavicular Ligament Reconstruction. Am J Sports Med 2005 33: 1723 • Mikek, M. Long-Term Shoulder Function After Type I and II Acromioclavicular Joint Disruption. Am J Sports Med 2008 36: 2147 • Schlegel, T et al. A Prospective Evaluation of Untreated Acute Grade III Acromioclavicular Separations. Am J Sports Med 2001 29: 699 • Gonzalez-Lomas, G et al. Intramedullary Acromioclavicular Ligament Reconstruction Strengthens Isolated Coracoclavicular Ligament Reconstruction in Acromioclavicular Dislocations. Am J Sports Med 2010 38: 2113 • Tauber, M, et al. Dynamic Radiologic Evaluation of Horizontal Instability in Acute Acromioclavicular Joint Dislocations. Am J Sports Med 2010 38: 1188 • Mouhsine E, Garofalo R, Crevoisier X, Farron A. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599-602 • Phillips A, Smart C, Groom A. Acromioclavicular dislocation. Clin Orthop Relat Res. 1998;353:10-17 • Weinstein, D et al Surgical Treatment of complete acromioclavicular dislocations. AJSM 1995 23: 324-330 • • Kibler, B. AAOS OKU Sports Medicine 4 2009 Google Images Thank You • Questions?