Just Put a Magnet On It
advertisement
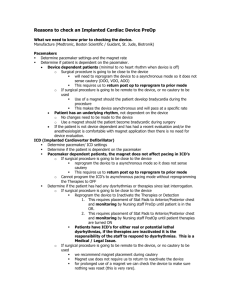
“Just Put a Magnet On It” An Update on Cardiac Implantable Electronic Devices Carolyn Boyle, RN, BSN, SRNA Goldfarb School of Nursing at Barnes-Jewish College Objectives • Review the perioperative implications of Cardiac Implantable Electronic Devices • Discuss the risks of Electromagnetic Interference (EMI) • Examine recommendations for preoperative assessment and preparation, intraoperative management, and postoperative recovery for patients with CIED’s Outline • • • • • • Case Study CIED Review Magnet Mechanism Practice Recommendations The Future of CIED’s Conclusions Case Study • 65 y.o. male with a hx of SCC of the head and neck – Presents with flap necrosis, osteonecrosis, orocutaneous fistula formation, & a complicated open wound – s/p mandibulectomy, tracheostomy, bil neck dissection, split thickness skin grafting, and G tube placement ~ 8 mos prior. – ~2 mos prior, pt had flap and trach revision – presenting for removal of hardware with radial and scapular flap reconstruction • PMH: SCC of head and neck, HTN, CHF (EF 30-40%), AFlutter, DM, COPD, Cardiac Arrest – Torsades arrest following cardioversion in 2012, warranting AICD placement Case Study con’t. • AICD last interrogated preoperatively 2 months prior with recommendations for magnet placement. • Uneventful induction of anesthesia, HOB turned 180 degrees, additional PIV’s and arterial line placed. Magnet placed over device and secured with 2 in silk tape. Case Study con’t. • Approximately 10 min after incision, surgeon using Bovie electrocautery while exposing the mandible • Patient’s AICD fired – No hemodynamic compromise – No arrhythmias • What happened? Pacemakers • Can be single chamber, dual chamber (A-V), or multi-chamber (bi-V) • The leads can be either monopolar or bipolar – Bipolar is most common today – reduces the risk of electromagnetic interference (EMI) In 2001, standardized programming codes were developed: PACING SENSING RESPONSE RATE MODULATION MULTISITE PACING A = Atrium A = Atrium I = Inhibited R = Ratemodulating V = Ventricle V = Ventricle V = Ventricle T = Triggered O = none A = Atrium D = Dual (A&V) D = Dual (A&V) D = Dual (I and/or T) D = Dual (A&V) O = None O = None O = None Internal Cardioverter Defibrillators (ICD) • Detect & treat ventricular arrhythmias – Today, incorporate pacemakers in case defibrillation results in bradycardia or asystole • Can be single chamber (RV lead only), dual chamber (A&V leads), or triple chamber (atrial, RV, LV leads). – Pre-programmed ‘zones’ based on heart rates and chamber of origin. – Based on rate, the device can initiate antitachycardia pacing or deliver a defibrillatory shock Potential Perioperative Problem: Electromagnetic Interference (EMI) Classic Causes: • Surgical electrocautery • Nerve stimulator • Evoked potential monitoring • Radiofrequency Ablation Potential Causes: • Fasciculations • Shivering • Large tidal volumes • Lithotripsy Pacemaker: Inhibition of pacing due to oversensing Brief exposure generally not a problem Prolonged exposure can lead to conversion to asynchronous pacing mode Defibrillator: inappropriate defibrillation Magnet Mechanism: The Reed Switch Source: Sony et al 2011 ***Magnet effect on CIED is extremely variable depending on the device, body habitus, manufacturer, programmed settings, and battery life. Magnet + PACEMAKER • Usually, a magnet will convert a pacemaker to asynchronous mode – Device response to magnet can be programmed – Rate depends on the manufacturer and the battery life – Asynchronous pacing mode depends on prior settings DDD DOO VVI VOO AAI AOO • Caution: Asynchronous rate may not always meet the physiologic demands of the patient • Upon removal, device should revert to originally programmed pacing mode Source: Sony et al 2011 Magnet + DEFIBRILLATOR • Usually, a magnet will prevent antitachycardic pacing and defibrillation – In order to prevent oversensing of EMI • Modern AICD’s are also pacemakers – a magnet will not have any effect on the pacemaker function!! – For patients with AICD’s who are pacemaker dependent preoperative interrogation and reprogramming is recommended Source: Sony et al 2011 February, 2011 Focused Pre-Operative Evaluation – Presence of device • H&P, medical record review, CXR, EKG, physical exam – Type of device • Manufacturer ID card, CXR, supplemental records, consult cardiology, year placed – Dependency on pacemaker function • Verbal history of syncope or bradycardia requiring CIED placement, AV node ablation, 100% paced on EKG – Device function • Best way: comprehensive evaluation (interrogation) • At minimum: evaluation of EKG or rhythm strip, discussion with patient CXR Interpretation CXR Interpretation CXR Interpretation CXR Interpretation CXR Interpretation Preparation is Everything! • Likelihood of Electromagnetic Interference (EMI) • Need for preoperative CIED reprogramming – Asynchronous pacing – Suspension anti-tachyarrhythmia functions • Suggest the use of Bipolar/ Harmonic electrocautery • Assure presence of external pacing/ defibrillation capabilities before, during, and after the procedure • Evaluating the possible effect of anesthetic technique on CIED function – Consider positioning of the patient EMI above umbilicus? From: Neelankavil et al. 2013. YES NO No reprogramming or magnet necessary. Have magnet available. Pacemaker Dependent? YesMagnet/ reprogram to asynch ICD Deactivate ICD – magnet/ reprogram Pacemaker Dependent? NoConsider reprogram/ magnet if source is <15 cm from generator. Have magnet avail. No- Yes- No reprogram necessary Reprogram to asynch. Intra-operative Management • If a magnet is placed or the device is reprogrammed, external defibrillation should be immediately available! – Place pads as far away from generator as possible – A-P placement is preferred Intraoperative Management • Monitor patient appropriately, monitor function of device, and monitor for signs of EMI • Assure the cautery grounding pad is positioned so that the current pathway doesn’t cross through or near the device – This may mean that sites other than the thigh should be used • Surgeon should avoid cautery near the device • Short, intermittent bursts of cautery at the lowest possible energy level is ideal • Risk of EMI is much greater with monopolar than bipolar cautery Algorithm for Emergent Cardioversion or Defibrillation Observe for appropriate CIED response Magnet placed preop Remove Magnet! Prepare for external defib or cardioversion Surgeon terminates all sources of EMI Device reprogrammed preop Re-enable therapies if programmer immediately available Post-Operative Care • Continuous monitoring • Pacing & defibrillation available • Regardless of the anesthetic approach to the CIED, electrocautery within 6 inches of the device can damage to the internal circuitry and post-operative interrogation is recommended • If there is any question, device should be interrogated to assess function Case Study Conclusion • Electrocautery removed from the field, device representative called to the room – Interrogated device, confirmed defibrillation – Unsure why magnet failed – Manual reprogramming of defibrillator • Surgery proceeded without further incident • Device interrogated postoperatively and returned to preoperative settings The Future of CIED’s NanostimTM Leadless PM Subcutaneous ICD THANK YOU! QUESTIONS? References American Society of Anesthesiologists Committee on Standards and Practice Parameters. (2011). Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: Pacemakers and implantable cardioverter-defibrillators. Anesthesiology, 114, 247-261. doi: 10.1097/ALN.0b013e3181fbe7f6 Neelankavil, J. P., Thompson, A., Mahajan, A. (2013). Managing cardiovascular implantable electronic devices (CIED’s) during perioperative care. APSF Newsletter, 28, 31-35. Jacob, S., Panaich, S. S., Maheshwari, R., Haddad, J. W., Padanilam, B. J., John, S. K. (2011). Clinical applications of magnets on cardiac rhythm management devices. Europace, 13, 1222-1230. doi: 10.1093/europace/eur137 Lanzman, R. S., Winter, J., Blondin, D., Furst, G., Scherer, A., Miese, F. R., Abbara, S., Kropil, P. (2011). Where does it lead? Imaging features of cardiovascular implantable electronic devices on chest radiograph and CT. Korean J Radiol, 12 (5), 611-619. doi: 10.3348/kjr.2011.12.5.611. Schulman, P. M., Rozner, M. A. (2013). Use caution when applying magnets to pacemakers or defibrillators during surgery. Anesthesia & Analgesia, 117, 422-427. doi:10.1213/ANE.0b013e31829003a1 Rooke, G. A., Bowdle, T. A. (2013). Perioperative management of pacemakers and implantable cardioverter defibrillators: It’s not just about the magnet. Anesthesia & Analgesia, 117, 292-294. doi: 10.1213/ANE.0b013e31829799f3 Rozner, M. (2004). Pacemaker misinformation in the perioperative period: Programming around the problem. Anesthesia & Analgesia, 99, 1582-1584. doi: 10.1213/01.ANE.0000140244.35896.D7