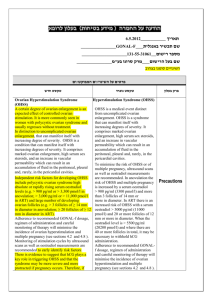
OHSS is a serious, potentially lifethreatening, iatrogenic complication of
“controlled” ovarian stimulation.
To optimize the ovarian response without
provoking OHSS is the best compromise
that should be reached by an ideal
regimen of stimulation, which is
unfortunately still not consistently
achievable.
PCO-like ovarian ultrasound features
(more than 10 follicles) are a predictive
factor for OHSS in IVF.
Tibi, 1989
Increased risk for OHSS in patients with a
LH/FSH ratio of more than 2.
Delvigne, Human Reprod 1993
The incidence of OHSS in PCOS patients
is 6%
Brinsden, Br J Obstet Gynecol 1995
Clomiphen citrate
Nonstimulated – natural cycle
Low dose gonadotropin protocols
› Agonist
› Antagonist
Trigger the ovulation
Luteal phase support
Metformin
IVM
Coasting
Patients with PCOS are unlikely to benefit
from this procedure since their success in
development of a single follicle leading
to the retrieval of a single, good quality
oocyte during a spontaneous cycle
remains uncertain.
Ovulation is restored in 80%, but
pregnancy is achieved in 35% of patients
Imani, Fertil Steril 2002
75% of the pregnancies occur within the
first three cycles of CC treatment
Gysler, Fertil Steril 1982
20-25% of PCOS patients remain resistant
to CC
CC is rarely associated with severe OHSS
Kistner, Obstet Gynecol Surv 1965
Two reviews from The Cochrane Library
on clinical trials investigating
gonadotropin therapy for ovulation
induction in women with
clomipheneresistant PCOS, concluded
that no significant benefit could be
demonstrated from urinary FSH versus
hMG in terms of pregnancy rate, but a
significant reduction in OHSS associated
with FSH was observed. Hughes 1997, Nugent 2002
Early reports suggested a relationship
between the type of gonadotropin
preparation utilized and the risk of OHSS.
More recent comparisons between
recombinant follicle-stimulating hormone
(rFSH) and human menopausal
gonadotropins (hMG) did not show
significant differences among variable
drug regimens.
The clinical pregnancy rates per cycle
started were higher with rFSH than uFSH,
although the magnitude of the observed
difference was small, 3.7%. No significant
differences were detected in the rates of
miscarriage, multiple pregnancy and
OHSS.
European and Middle East Orgalutran Study
Group, Human Reprod 2001
During cycles without GnRH-a
suppression, either a significant LH surge
or at least marked luteinization will limit
continued gonadotropin stimulation and
thus lead to a concomitantly lower risk of
OHSS.
FIVNAT results showed that the use of
GnRH-a led to significantly higher
preovulatory estradiol concentrations,
and to more frequent severe
hyperstimulation (4.6% vs. 0.6% for
nonGnRH-a/hMG cycles).
FIVNAT, Contracept Fertil Sex 1989
The type of GnRH agonist to be used in
patients at risk of OHSS has not been
extensively studied. It is obvious that the
short protocol should not be proposed,
as the initial flare-up effect could lead to
an excessive ovarian response.
In the long protocol, depot formulation
versus daily injection and follicular versus
luteal start have not been compared
prospectively in patients at risk of OHSS.
It has been proposed that a longer
period of desensitization (30 instead of 15
days) is of benefit by reducing androgen
levels.
The longer duration of treatment did not
improve pregnancy rates but did
apparently decrease the incidence of
hyperstimulation.
Salat-Baroux, Human Reprod 1988
Patients receiving antagonist treatment
have lower estradiol serum levels at the
time of hCG administration, mostly
because of a lower number of follicles,
which could explain the lower incidence
of OHSS.
Ludwig M, Arch Gynecol Obstet 2000
There was a statistically significant
reduction in incidence of severe OHSS
with antagonist protocol. The relative risk
ratio was 0.61 (P=0.01; 95% CI 0.42 - 0.89).
In addition, interventions to prevent
OHSS (e.g. coasting, cycle cancellation)
were administered more frequently in
the agonist group (P=0.03; OR 0.44, 95%
CI 0.21 - 0.93).
Al-Inany, Cochrane Database 2006
The GnRH-antagonist protocol involved
starting gonadotropins on day 3 of the
menstrual cycle. Transvaginal ultrasound
monitoring was commenced on day 5 of
ovarian stimulation and repeated every
2-3 days.
USG
HCG
USG
300 IU
225 IU
150 IU
Antagonist (start at 6th day)
3th day
7th day
12th day
The starting dose for gonadotropin is
based on
› age,
› body mass index (BMI)
› existence of PCOS,
› previous history of OHSS or high response.
Two comparative prospective studies of
the conventional regimen, with the
chronic low-dose step-up protocol using
urinary FSH or rhFSH for ovulation
induction in PCOS patients, showed that
the low-dose approach eliminated
complications of OHSS and multiple
pregnancies without jeopardizing the
incidence of pregnancy.Homburg, Fertil Steril 1995
Hedon, Human Reprod 1998
USG
HCG
USG
Mid
luteal
300 IU
225 IU
150 IU
Agonist
3th day
7th day
12th day
HCG
USG
150 IU
75 IU
Agonist
Mid
luteal
3th day
7th day
USG
USG
112.5 IU
75 IU
3th day
150 IU
14th day
21st day
The step-down protocol applies decremental
doses of gonadotropins once ovarian response
is established, but the starting dose is higher
than in the step-up approach.
Monitoring of follicular growth is, however,
more stringent than with the step-up
approach. In addition, the long half-life of
currently available FSH preparations makes it
difficult to judge the correct reduction of dose.
Clinical results are similar to those obtained
with the step-up approach.
van Santbrink, Human Reprod 1995
USG
HCG
300 IU
150 IU
Agonist
Mid
luteal
3th day
6th day
Unlike a step-up protocol, which
continuously rescues follicles from
atresia, a step-down protocol will allow
more follicles to undergo atresia, thus
reducing the overall number of follicles
capable of secretory activity by the time
hCG is administered.
An alternative method for ovulation
induction with FSH in PCOS patients is the
so-called sequential protocol, which
combines an initial step-up gonadotropin
administration followed by a step-down
regimen after follicular selection (leading
follicle > 14 mm). In a comparative study
with the standard low-dose step-up
regimen, both approaches were shown to
be safe and effective.
Hugues, Human Reprod 1996
More recently, Filicori et al. proposed
conducting the end of stimulation using
a treatment composed of low-dose
hCG. Low-dose hCG as a source of LH
activity was associated with FSH or was
used alone in the second part of the
follicular phase.
Filicori, Human Reprod Update 2002
Ovarian stimulation with daily late follicular phase administration of
low-dose human chorionic gonadotropin for in vitro fertilization:
a prospective, randomised trial Serafini, et al, Fertil Steril 2006
Ovarian stimulation with daily late follicular phase administration of
low-dose human chorionic gonadotropin for in vitro fertilization:
a prospective, randomised trial Serafini, et al, Fertil Steril 2006
Use
a combination of frequent
serum estradiol measurements
and ultrasonographic
assessments of follicular
growth.
Decrease in hCG dose
› 10.000 IU vs. 5.000 IU or 3.000 IU no difference
The use of GnRH antagonists could further
decrease the incidence of OHSS in high-risk
patients when replacing hCG by a GnRH
agonist to trigger ovulation.
A recent prospective study found a lower
pregnancy rate in patients in whom GnRH
agonists were used to trigger ovulation.
There was no statistically significant
difference between rhCG vs uhCG
regarding the incidence of OHSS.
Al-Inany, Cochrane Database 2005
A multicenter double-blind study
revealed that new recombinant human
LH can be as effective as hCG in
inducing the final follicular maturation in
IVF treatment with a lower incidence of
OHSS.
European Recombinant LH Study Group 2001
The odds of OHSS were more than 2-fold higher
with treatments involving hCG than with
progesterone alone (OR 3.06, 95% CI 1.59 to
5.86).
Comparing routes of progesterone
administration, reductions in clinical pregnancy
rate with the oral route, compared to the
intramuscular or vaginal routes, did not reach
statistical significance, but there was evidence
of benefit of the intramuscular over the vaginal
route for the outcomes of ongoing pregnancy
and live birth.
Daya, Gunby, Cochrane Database 2004
Due to the abundance of follicles in the
ovary, PCOS patients present an
excellent clinical opportunity for the
retrieval of unstimulated immature eggs
and do In Vitro Maturation.
The immature oocytes are retrieved from
antral follicles of unstimulated (or minimally
stimulated) ovaries via the transvaginal
approach.
The oocytes are subsequently matured in
vitro in a special formulated culture
medium for 24-48 h. The mature oocytes
are fertilized, usually by intracytoplasmic
sperm injection (ICSI), and the selected
embryos are transferred to the uterus 2-3
days later.
Because no expensive gonadotropin
stimulation and no extensive monitoring
scans are required, the cost of IVM
treatment is lower than that of IVF.
The IVM treatment schedule is shorter,
causing less stress, and it is not necessary to
wait for 2 to 3 months between treatment
cycles because no stimulation is involved.
The risk of OHSS can be avoided by IVM
treatment, especially in women with
Child, Obstet Gynecol 2002
PCO/PCOS.
ART Service
Paris
Montreal Taipei
Helsinki
Seoul
Seoul
Cycles (n)
138
254
68
239
203
419
Oocytes
retrieved
12.1
11.9
22.5
8.0
15.5
16.4
Maturation
rate (%)
61.7
78.8
74.2
58.6
55.3
73.2
Fertilization
rate (%)
62
69.2
72.8
51.3
75.1
79.0
Transferred
embryo
2.4
3.4
3.8
5.0
4.3
Clinical
Pregnancy
rate(%)
24.5
24.0
33.8
21.9
32.7
26.6
Tan SL, et al. In vitro Maturation of Human Oocytes, 2007
Clinical pregnancy rate 35% per cycle
Implantation rate 15% per embryo
Al-Sunaidi, Fertil Steril 2007
Metformin has been studied and mostly
shown to restore menstrual cycles and
confirm ovulation in anywhere between
25 - 90% of cases.
A recent analysis of 13 randomized
controlled trials showed that metformin
increased the ovulation rate almost four
times compared to placebo when it was
administered in combination with
clomiphene citrate.
No metformin (n=159)
Metformin (n=128)
Age
34.8
33
BMI
27.2
27.8
HMG ampoules
37.1
41.1
Oocytes retrieved
23.8
18.8
Embryos tranferred
2.8
3
Clinical pregnancies
37.6
30.5
20
1
Moderate and severe OHSS*
Khattab, Reprod Biomed Online, 2006
Metformin (n=52)
Placebo (n=49)
Cancellation %
9.6
4.1
Nr of eggs
17.3
16.2
2
2
Clinical preg rate %
38.5
16.3*
Live birth rate %
32.7
12.2*
Severe OHSS %
3.8
20.4*
Nr of embryos transferred
* p< 0.05
Tang, Human Reprod, 2006
First described and applied by Sher et al
in 1993
hCG administration postponed until the
patients serum E2 level decreases to a
safer zone.
E2 levels usually rise rapidly in the 48 h
following initiation of the coasting period,
then plateaued and began to fall 96-168
h after the gonadotropins were stopped.
Cochrane review identified 13 studies of
which only one trial met the inclusion
criteria.
There was no difference in the incidence
of moderate and severe OHSS and in the
clinical pregnancy rate between the
groups.
D’Angelo et al., Cochrane Library, 2002
A recent review of ten studies showed
that < 2% of women developed OHSS
while maintaining acceptable pregnancy
rates (36.5-63%) when coasting was
continued until serum estradiol levels fell
below 3000 pg/ml.
Levinson-Tavor, Human Reprod 2003
Study
E2 1st day
coasting (pg/mL)
Sher et al.1993
Sher et al.1995
Benadiva et al 1997
Tortoriello et al. 1998
Dhont et al. 1998
Lee et al.1998
Fluker et al. 1999
Egbase et al. 1999
Waldenstrom et al. 1999
Delvigne et al.2001
Al-Shawaf et al. 2001
>6,000
>6,000
3,803
4,015
3,834
5,167
5,077
10,055
6,292
8,877
4,400
Grochowski et al. 2001
Isik et al. 2001
Al-Shawaf et al. 2002
Ulug et al. 2002
Isaza et al. 2002
Chen et al. 2003
Tozer et al. 2004
Moreno et al. 2004
Garcia-Velasco et al. 2004
Ulug et al. 2004
>3,000
4,400
4,563
6,395
3,753
4,400
5,769
5,904
5,365
No.of days
coasting
2
3.05
1.9
2.8
2
4.9
4.3
3
3.4
3.5
4
3.6
2.9
4.2
1.5
4
3.6
3.8
2.7
Embryos
E2 day Hcg
No.of
transferre PR (%) IR (%)
(pg/Ml
oocytes
d
>3,000
>3,000
2,206
2,407
2,341
3,667
2,832
1,410
1,870
1,492
1,368
21
15
15.7
19.7
17.3
10.8
28.3
10
16
11
>3,000
3,000
2,718
2,613
2,181
4,528
1,433
2,852
3,312
3,113
18.3
13.1
17.5
19.6
21
12
18.1
19.5
19.8
5.4
4.9
2.3
3 max
3
2.7
2
2.1
Severe
OHSS(n)
35.2
0/17
41
58.8
44.5
37.5
40
36.5
33
51
25.5
18.1
0/51
1/22
3/44
1/120
4/20
1/63
3/15
1/65
0/157
1/50
2/112
24.2
19.0
22
9.6
20.3
19
24.8
28.8
1/89
4/207
0/15
3/31
0/22
0/132
5/159
4/233
3.2
2.1
4.2
2.6
5
1.8
46.5
32.3
50.5
35.4
50.7
52.9
32.1
33.3
2
3.5
42.4
56.8
16.9
20
14.3
31
Coasting < 4 days
(n=983)
Coasting >4 days
(n=240)
Age
30.2
29.9
Oocytes retrieved*
16.5
14.9
Mean no of embryos trans
2.99
3.03
Clin pregnancy rate*
52.0
35.9
Implantation rate*
26.3
18.2
Mansour, et al., Fertil Steril, 2005
Coasting is a good alternative that can
avoid cycle cancellation in high
responders, who have high risk of
developing severe OHSS
Even if OHSS develops after coasting
both its incidence and severity will be
diminished
No one gonadotropin is superior to others
for reducing the incidence of OHSS
Antagonist-low dose step up is the best
protocol available
Monitoring of the E2 and USG of follicles is
crucial
Luteal phase support with hCG increases
the incidence of OHSS.
Progesterone intravaginally or i.m. should
be used for the patients at risk of OHSS
IVM
is a novel method and must
be developed for better results
Coasting is an effective method
for preventing severe OHSS
No method has been developed
that will completely prevent
severe OHSS after ovarian
stimulation.
r FSH
u FSH
Bergh, Hum Reprod 1997
5.1
1.7
Out, Hum Reprod 1995
3.2
2.0