Does placement of an MRI in the ED increase utilization and
advertisement
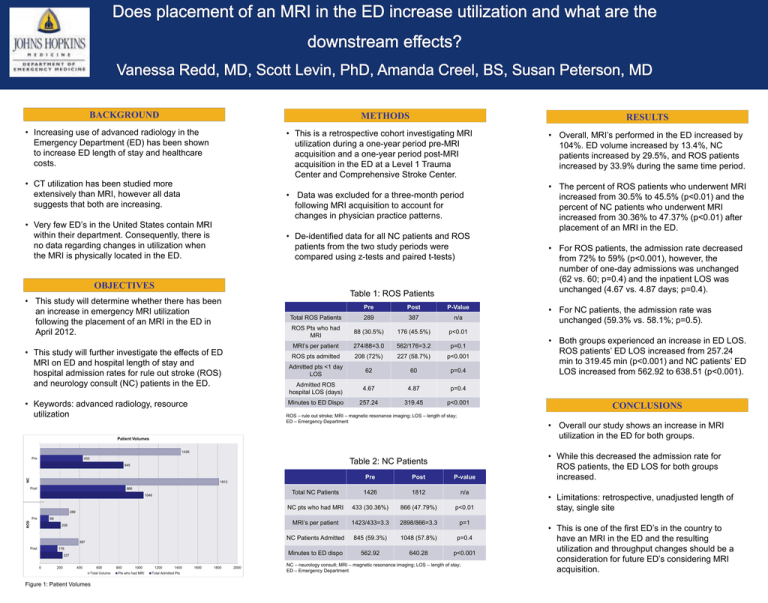
BACKGROUND METHODS • Increasing use of advanced radiology in the Emergency Department (ED) has been shown to increase ED length of stay and healthcare costs. • CT utilization has been studied more extensively than MRI, however all data suggests that both are increasing. • Very few ED’s in the United States contain MRI within their department. Consequently, there is no data regarding changes in utilization when the MRI is physically located in the ED. RESULTS • This is a retrospective cohort investigating MRI utilization during a one-year period pre-MRI acquisition and a one-year period post-MRI acquisition in the ED at a Level 1 Trauma Center and Comprehensive Stroke Center. • Overall, MRI’s performed in the ED increased by 104%. ED volume increased by 13.4%, NC patients increased by 29.5%, and ROS patients increased by 33.9% during the same time period. • Data was excluded for a three-month period following MRI acquisition to account for changes in physician practice patterns. • The percent of ROS patients who underwent MRI increased from 30.5% to 45.5% (p<0.01) and the percent of NC patients who underwent MRI increased from 30.36% to 47.37% (p<0.01) after placement of an MRI in the ED. • De-identified data for all NC patients and ROS patients from the two study periods were compared using z-tests and paired t-tests) OBJECTIVES Table 1: ROS Patients • This study will determine whether there has been an increase in emergency MRI utilization following the placement of an MRI in the ED in April 2012. • This study will further investigate the effects of ED MRI on ED and hospital length of stay and hospital admission rates for rule out stroke (ROS) and neurology consult (NC) patients in the ED. • Keywords: advanced radiology, resource utilization Pre Post P-Value Total ROS Patients 289 387 n/a ROS Pts who had MRI 88 (30.5%) 176 (45.5%) p<0.01 MRI’s per patient 274/88=3.0 562/176=3.2 p=0.1 ROS pts admitted 208 (72%) 227 (58.7%) p<0.001 Admitted pts <1 day LOS 62 60 p=0.4 Admitted ROS hospital LOS (days) 4.67 4.87 p=0.4 Minutes to ED Dispo 257.24 319.45 p<0.001 ROS – rule out stroke; MRI – magnetic resonance imaging; LOS – length of stay; ED – Emergency Department 1426 433 Table 2: NC Patients NC 845 Pre Post P-value Total NC Patients 1426 1812 n/a NC pts who had MRI 433 (30.36%) 866 (47.79%) p<0.01 MRI’s per patient 1423/433=3.3 2898/866=3.3 p=1 NC Patients Admitted 845 (59.3%) 1048 (57.8%) p=0.4 Minutes to ED dispo 562.92 640.28 p<0.001 1812 Post 866 1048 289 Pre ROS 88 208 387 Post 176 227 0 200 400 600 Total Volume Figure 1: Patient Volumes 800 1000 Pts who had MRI 1200 1400 Total Admitted Pts 1600 1800 2000 • For NC patients, the admission rate was unchanged (59.3% vs. 58.1%; p=0.5). • Both groups experienced an increase in ED LOS. ROS patients’ ED LOS increased from 257.24 min to 319.45 min (p<0.001) and NC patients’ ED LOS increased from 562.92 to 638.51 (p<0.001). CONCLUSIONS • Overall our study shows an increase in MRI utilization in the ED for both groups. Patient Volumes Pre • For ROS patients, the admission rate decreased from 72% to 59% (p<0.001), however, the number of one-day admissions was unchanged (62 vs. 60; p=0.4) and the inpatient LOS was unchanged (4.67 vs. 4.87 days; p=0.4). NC – neurology consult; MRI – magnetic resonance imaging; LOS – length of stay; ED – Emergency Department • While this decreased the admission rate for ROS patients, the ED LOS for both groups increased. • Limitations: retrospective, unadjusted length of stay, single site • This is one of the first ED’s in the country to have an MRI in the ED and the resulting utilization and throughput changes should be a consideration for future ED’s considering MRI acquisition.