- Neurology Exchange: Exploring the Latest Advances in
advertisement

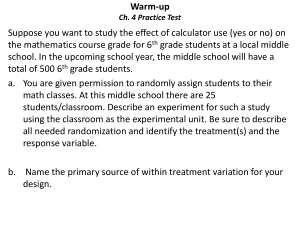
Welcome! • Please remove the Pre-activity Survey located at the front of your syllabus packet. Please fill it out and pass forward prior to the beginning of the lecture. • It is important that you do this prior to the talk, as we will repeat these questions at the end of the program to gauge the effectiveness of the activity. These tests are not graded, but are used to build CME that suits your needs. Your participation is greatly appreciated. Disclosures • The relevant financial relationships reported by faculty that they or their spouse/partner have with commercial interests is located on page 5 of your syllabus • The relevant financial relationships reported by the steering committee that they or their spouse/partner have with commercial interests is provided on page 5 of your syllabus • The relevant financial relationships reported by the nonfaculty content contributors and/or reviewers that they or their spouse/partner have with commercial interests is located on page 5 of your syllabus Off-label Discussion Disclosure This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the Food and Drug Administration. PCME does not recommend the use of any agent outside of the labeled indications. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications and warnings. The opinions expressed are those of the presenters and are not to be construed as those of the publisher or grantors. Educational Objectives At the conclusion of this activity, participants should be able to demonstrate the ability to: • Select the most appropriate DMD therapies that can be used to initiate treatment earlier in the disease course • Develop individualized treatment plans to optimize adherence and improve outcomes in patients with MS • Describe how emerging biomarkers and newer MRI measures to improve the accuracy of diagnosis and monitoring of MS disease activity Multiple Sclerosis: An Immuno-genetic Disease Genetic Predisposition Environmental Factors -Twins studies Demographics/Epidemics -HLA-DR2 (DRß1*1501) (antigen presentation) Microbial Agents EBV -IL-2Ra (regulatory T-cells) Vitamin D Smoking -IL-7Ra (memory T-cells) GWAS (>100 alleles) Dhib-Jalbut S. 2013. Salt Immune Dysregulation MS Immunopathogenesis of MS Inflammatory Processes Occurring Early in MS Lead to Demyelination and Axonal Loss Inflammation Regeneration Onset of Disease Time Inflammation Compston A et al. Lancet. 2008;372:1502-1517. Paolillo A et al. J Neurol. 2004;251:432-439. Demyelination Axonal loss Kuhlmann T et al. Brain. 2002;125:2202-2212. Trapp BD et al. Curr Opin Neurol. 1999;12:295-302. Dublin Revision 2011 • For DIS: At least one T2 lesion in two of the following locations: – Periventricular – Juxtacortical – Infratentorial – Spinal cord • For DIT: Any new lesion on any follow-up scan after a baseline scan done anytime after onset of CIS DIS=Dissemination in space; DIT=Dissemination in time; CIS= Clinically isolated syndrome Polman et al. Ann Neurol. 2011;69:292-302. McHugh et al. Mult Scler. 2008;14:81-85. Single Early MRI • In CIS, a single MRI, even in first 3 months, with Gad enhancing lesion(s) and T2H has high specificity for development of CDMS CDMS = clinically definite MS Polman et al. Ann Neurol. 2011;69:292-302. Radiologically Isolated Syndrome 5-year Risk for an Initial Clinical Event from a Multinational Cohort (RISC) • Retrospective analysis of 20 databases from 5 countries • >430 patients (largest cohort examined to date) • 5-year observed conversion rate to first clinical event: 34% • In multivariate model, several factors significantly associated with conversion: – Age (younger > older) – Gender (M > F) – Presence of spinal cord lesions RISC = Radiologically Isolated Syndrome Consortium Okuda D et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract PL01.002. RIS: Management Implications • Potential for misdiagnosis • High probability of benign MS • “Wait and watch” approach may be best • Future challenges: – How to identify high-risk RIS group – Standardized MRI – Combining MRI with other predictors – Population-based prospective study RIS = Radiologically Isolated Syndrome Okuda D et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract PL01.002. “I look to the future because that’s where I’m going to spend the rest of my life.” — George Burns Predicting the Course of MS • Clinical features of onset bout – Motor worse than sensory – Polyregional worse than monosymptomatic – Early bladder involvement poor prognosis • Incomplete recovery from initial attack • Short interval between attacks MRI and MS Prognosis • Initial MRI EDSS > 3 70 – T2 lesion numbers – 3 or 4 Barkhof criteria moderate correlation with EDSS at 5 years 60 % patients – Median EDSS at 20 years = 6 for ≥10 T2 lesions EDSS ≥ 6 50 40 30 20 10 0 0 1-3 4-9 # of brain lesions Fisniku LK. Brain. 2008;131:808-817. ≥10 “The future ain’t what it used to be.” Lawrence Peter “Yogi” Berra Assessing Risk • Patients need to be informed and involved in decisionmaking process • Need to steer patients to a limited number of options based upon disease severity • Patient risk tolerance to adverse events • Patient disease tolerance to neurologic dysfunction Defining Breakthrough Disease • 1 moderate/severe clinical relapse over 1 year • 2 mild clinical relapses over 2 years • 1-2 Gd enhancing brain lesions over 1 year • 2 T2 lesions over 2 years • A functionally significant worsening in cognition, ambulation, upper extremity function • Need to account for time for medication to work optimally • Follow-up MRI 6-12 months after treatment initiation Existing and Emerging MS Therapies Ofatumumab Ocrelizumab Daclizumab Ampyra® (4-amino pyradine) Mastinib Betaseron® Nuedexta® Tysabri® (IFNβ-1b) (dextromethorphan/ quinidine) (natalizumab) Avonex® Laquinimod Plegridy® Extavia® (IFNβ-1a) (IFNβ-1b) (IFNβ-1a) Cladribine* Lemtrada® Copaxone® (alemtuzumab) (glatiramer acetate) Gilenya® Aubagio® (fingolimod) Novantrone® (teriflunomide) (mitoxantrone) Tecfidera® (dimethyl fumarate) Rebif ® (IFNβ-1a) 1995 2000 2005 Approved therapies 2009 Approval date 2010 2011 Phase III completed *In March 2011, the FDA did not approve cladribine and requested Merck KGaA provide an improved understanding of its safety risks and overall benefit-risk profile 2012 2013 2014 Estimated launch date In Phase III ADVANCE Phase III Trial of PEGylated IFNb-1a in RRMS • PegIFN has longer t1/2 and results in prolonged exposure (AUC, Cmax) than standard formulations • Pts (n=1512) randomized to placebo, pegIFNb-1a 125 mcg q2wk, or q4wk PEGIFNB-1A Q2WK PEGIFNB-1A Q4WK 35.6%* 27.5%* Accrual of disability 38%* 38%* T2 lesions 67%* 28%* Gd-enhancing T1 lesions 86%* 36%* ENDPOINT (reduction compared with placebo at 1 year) ARR • Neutralizing Abs seen in <1% of patients in both IFN groups • Adverse events similar to known IFN profile (ISRs, pyrexia, flu-like symptoms, hepatic enzyme elevations) • ATTAIN: long-term extension study from ADVANCE ongoing * Statistically significant finding PEG=polyethylene glycol; AUC=area under the curve; ARR=annualized relapse rate; IFN=interferon; Abs=antibodies; ISRs=injection site reactions Calabresi P et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S31.006. Glatiramer Acetate Low-frequency Administration (GALA): Phase III Study Primary Endpoint: ARR 34.4% reduction, P < 0.0001 ARR ± SEM 0.5 0.4 0.3 0.505 0.2 0.331 0.1 7 Enlarging T2 Lesions (n) 0.6 Secondary Endpoint: Cum. No. of New/Enlarging T2 Lesions 34.7% reduction, P < 0.0001 6 5 4 3 5.592 2 3.65 1 0 0 Placebo (n = 461) GA 40 mg tiw (n = 943) Placebo (n = 441) ARR = annualized relapse rate; SEM = standard error of mean Khan O et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S01.005. GA 40 mg tiw (n = 884) Lymphocyte Trafficking Inhibition Implications for Multiple Sclerosis Therapy Leukocyte Chemoattractant signal a4b1 (VLA-4) Blood Vessel Lumen Leukocyte infiltration and brain inflammation Endothelial Cells Tissue VCAM-1 Leukocyte Chemoattractant Signal a4b1 (VLA-4) Blood Vessel Lumen Endothelial Cells Tissue VCAM-1 O’Connor P. Expert Opin Biol Ther. 2007;7:123-136. Reduced leukocyte infiltration and brain inflammation Natalizumab v Placebo Affirm Study 0.81 Annualized Relapse Rate (95% CI) 1.0 P<0.0001 0.9 0.8 0.7 0.6 68% 0.5 0.4 0.26 0.3 0.2 0.1 0.0 Placebo n=315 Polman C et al. N Engl J Med. 2006;354:899-910. Natalizumab n=627 Natalizumab Use in the Post-marketing Setting and PML Risk Overall Exposure ≥ 18 Months ≥ 24 Months ≥ 30 Months ≥ 36 Months ≥ 42 Months ≥ 48 Months 72,400 60,300 3 50,300 2.95 41,400 2.5 33,500 2.33 2 26,100 19,600 1.5 Patients Incidence per 1,000 patients ≥ 12 Months 104,300 224,718 patient-years of natalizumab exposure 2.79 2.63 2.63 2.23 2.32 1.94 1.90 1.76 1.54 1.38 1 0.82 0.5 0.11 0.02 0 Post Marketing 0.61 0.45 0.05 1–12 13–24 25–36 37–48 49–60 Number of infusions *As of October 22, 2012: 298 cases of natalizumab-associated PML have been reported; of these, 62 patients have died (22%) Vermersch P et al. Presented at ECTRIMS 2012; October 9-13, 2012; Lyon, France. [Abstract 173]. Estimated Incidence of Natalizumabassociated PML Stratified by Risk Factors Anti-JCV Antibody Status Negative Positive 0.1/1000 95% CI: 0.1-0.35 Prior IS Use? Sorenson P et al. Mult Scler. 2012;18:143-152. No Yes Natalizumab exposure No Prior IS Use Prior IS Use 1–24 months 0.7/1,000 patients 1.8/1,000 patients 25–48 months 5.3/1,000 patients 11.2/1,000 patients 49–72 months 6.1/1,000 patients Insufficient data Anti-JCV Antibody Index Distribution in Anti-JCV Ab+ non-PML and pre-PML Patients with No Prior IS Use Plavina T et al. Use of anti-JC virus antibody index to further define risk of PML in anti-JCV antibody-positive TYSABRI-treated patients with MS. Platform presentation presented at 23rd Annual Meeting of European Neurological Society, June 9, 2013; Barcelona, Spain. PML Risk Estimates by Index Threshold in Anti-JCV Ab+ Patients with No Prior IS Use Plavina T et al. Anti-JCV antibody index further defines PML risk in TYSABRI-treated MS patients. Poster presented at CMSC 27th Annual Meeting, May 29-June 1 2013; Orlando, FL. Fingolimod (FTY720): Mode of Action S1P receptor T cell Prevents T cell invasion of CNS FTY720-P FTY720 results in internalization of the S1P1 receptor This blocks lymphocyte egress from lymph nodes while sparing immune surveillance by circulating memory T cells Cohen JA, Chun J. Ann Neurol .2011;69:759-777. LN FTY720 traps circulating lymphocytes in peripheral lymph nodes Fingolimod Efficacy FREEDOMS TRANSFORMS 0.6 P< 0.001 Adjusted Annualized Adjusted Annualized Relapse RelapseRate Rate 0.5 P<0 .001 P= 0.16 0.4 0.33 0.3 0.20 0.2 0.16 0.1 0.0 Interferon (N=4 31) Kappos L et al. N Engl J Med. 2010;362:387-401. Cohen JA, et al. N Engl J Med. 2010;362:402-415. Fingolimod, 0.5 mg (N=4 29) Fingolimod, 1.25 mg (N=4 20) Managing Fingolimod Patients • Prior to Treatment Initiation – Baseline CBC and hepatic panel – Ophthalmological examination – Cardiac status – Varicella immune status • Rx Initiation: 6-hour observation b/o bradycardia • On Treatment – CBC, hepatic panel – Ophthalmological exam at 3-4 months – Check BP Recent Additions to Fingolimod Prescribing Information First Dosing Monitoring Observe signs and symptoms of bradycardia for at least 6 hrs after first dose with hourly pulse and blood pressure measurement Obtain ECG prior to dosing and at the end of the observation period Monitor AV block until resolution if heart rate <45 bpm, or a new onset 2nd-degree or higher Pts at lowest post-dose heart rate at the end of observation period should be monitored until heart rate increases If symptomatic bradycardia, begin continuous ECG monitoring until symptoms have resolved • If pharmacological intervention required for bradycardia, continue ECG monitoring overnight in a medical facility, and repeat 1st-dose monitoring procedures for 2nd dose Patients who may be less tolerant of fingolimod-induced bradycardia are at higher risk of serious rhythm disturbance, or with prolonged QTc interval at baseline, or at any time during the observation period, should be observed overnight with continuous ECG monitoring Patients who have stopped taking fingolimod for more than 14 days and re-initialize treatment are advised to again follow these updated recommendations http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Label_ApprovalHistory#labelinfo. http://www.msrc.co.uk/index.cfm/fuseaction/show/pageid/1309. Teriflunomide A Selective Dihydro-orotate Dehydrogenase Inhibitor • A newly approved oral diseasemodifier for relapsing forms of MS (RMS) • Blocks de novo pyrimidine synthesis, reducing T- and B-cell proliferation and function in response to autoantigens • Preserves replication and function of cells (e.g. haemopoietic cells, memory T-cells) living on the existing pyrimidine pool (salvage pathway) Resting lymphocyte Blasting lymphocyte De novo pathway Nonlymphoid cells DHO-DH Teriflunomide Pyrimidine pools Salvage pathway CTP-, UTP-sugars Nucleotides CDP lipids Glycoproteins, Glycolipids RNA, DNA Phospholipids Cell-cell contact Adhesion and diapedesis Proliferation Ig secretion Cell membranes Second messengers DHO-DH, dihydro-orotate dehydrogenase; Miller A et al. Clinical and MRI outcomes from a Phase III trial (TEMSO) of oral teriflunomide in multiple sclerosis with relapses. Presented at AAN Annual Meeting, April 9-16, 2011, Honolulu, HI. Teriflunomide for RRMS (Phase III TEMSO Study) Key Clinical Outcomes Annualized Relapse Rate 0.6 0.5 RRR: 31.2% P=0.0002 RRR: 31.5% P=0.0005 0.539 EDSS 12 Week Sustained Change 30.0 25.0 0.4 23.7% P=0.0835 27.3 20.0 0.369 0.370 0.3 0.2 29.8% P=0.0279 21.7 21.7 20.2 7 mg (n = 365) 14 mg (n = 358) 15.0 10.0 0.1 5.0 0.0 Placebo (n = 363) 7 mg (n = 365) 14 mg (n = 358) Teriflunomide RRR = relative risk reduction O’Connor P et all. N Engl J Med. 2011;365:1293-1303. 0.0 Placebo (n = 363) Teriflunomide Teriflunomide Phase III TOWER Study Efficacy Outcome ARR (primary endpoint) Reduction vs placebo Placebo 0.501 12-week confirmed disability progression HR vs placebo Mean EDSS change (baseline to week 48) 0.089 *Statistically significant vs placebo. Miller A et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S01.004. Teri 7 mg Teri 14 mg 0.389* 22.3% 0.319* 36.3% 0.955 0.685* 0.042 -0.05* TOWER: Treatment-Emergent AEs Preferred term, % Headache Leading to discontinuation Placebo (n = 385) 10.9 0.3 Teriflunomide 7 mg (n = 409) 14.7 0 Teriflunomide 14 mg (n = 371) 12.4 0 Increased ALT Leading to discontinuation 8.3 1.6 11.2 2.9 14.0 2.4 Alopecia (hair thinning) Leading to discontinuation 4.4 0.3 10.3 0 13.5 1.6 Diarrhea Leading to discontinuation 7.3 0.3 12.0 1.0 11.1 0.8 Nausea Leading to discontinuation 8.8 0 8.3 0 10.2 0.8 Neutropenia Leading to discontinuation 2.9 0 7.1 1.0 9.4 2.2 ALT = alanine aminotransferase Miller A et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S01.004. Teriflunomide Counseling and Start-up • Pregnancy Category X • At Baseline: CBC with diff, LFTs, TB testing • Monthly x 6 months: AST/ALT • Every 6 months: CBC with diff, LFTs Proposed Mechanisms: Dimethyl Fumarate • An oral formulation of dimethyl fumarate • Inhibits the expression of adhesion molecules and proinflammatory cytokines • Induces a Th1 to Th2 shift • Decreases circulating T cells • Activates the Nrf2 pathway • >30 years of use of fumaric acids in the treatment of psoriasis (both topical and oral) Kappos L et al. Lancet. 2008;372:1463-1472. Gold R et al. N Engl J Med. 2012;367:1098-107. Gasperini C et al. Expert Opin Emerg Drugs. 2008;13:465-477. DMF: Integrated Efficacy Analysis of DEFINE and CONFIRM Endpoint (at 2 years) Annualized relapse rate (ARR) Reduction vs placebo Proportion of patients relapsed HR vs placebo Time to 12-week confirmed disability progression HR vs placebo Time to 24-week confirmed disability progression HR vs placebo *Statistically significant vs placebo Fox RJ et al. Presented at AAN; March 16-23, 2013; San Diego, CA. Abstract P07.097. Placebo (n = 771) DMF BID (n = 769) 0.37 0.19* 49% 0.57* 0.68* 0.71* Alemtuzumab MOA • Targets CD52 antigen expressed on B and T lymphocytes • FDA approved for leukemia • Phase II study comparing Campath vs Rebif in 334 patients – 12 mg/day for 5 days at month 0, 12, 24 – 24 mg/day for 5 days at month 0, 12, 24 • Three-year observation period with interim analyses Alemtuzumab vs Interferon-B1a: Care-MS Phase III Studies CARE – MS1 CARE – MS2 IFN-B1a Alemtuzumab (12mg) IFN-B1a Alemtuzumab (12mg) 0.39 0.18 0.52 0.26 Ann. relapse rate 54.9% (P<0.0001) Risk reduction Sustained disability (% pts) 11 Net EDSS change Cohen JA et al. Lancet. 2012;380:1819-1828. Coles AJ et al. Lancet. 2012;380: 1829-1839. 21.1 30% (P=0.22) Risk reduction Δ EDSS from baseline 8 49.4% (P<0.0001) - 0.14 - 0.14 12.7 42% (P=0.0084) 0.24 - 0.17 0.41 (P<0.0001) Extension Analysis of Care-MS Phase III Studies CARE-MS I CARE-MS II ARR 0.24 0.25 EDSS improvement 40% 45% Received alemtuzumab re-tx* 18% 20% *Criterion for re-treatment was 1 relapse or ≥ 2 new lesions on MRI Fox E et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S41.001. Safety Analysis of Care-MS Phase III Studies Autoimmune thyroid disorders • 19.4% in extension; 29.9% total study • Autoimmune thrombocytopenia (ITP):1.3%; nephropathy: 0.3% (n=3) Infections • More common with alemtuzumab compared with IFN (Incl. URI, UTI, sinusitis, and mucocutaneous herpetic and fungal infections) − Acyclovir prophylaxis seemed to reduce the risk of herpetic infection − Infections highest in mos 1 and 13 (after each alem course), − No evidence that neutrophil or lymphocyte counts before a treatment course predicted infection risk Fox E et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract S41.001. Wray S et al. Presented at AAN 2013; March 16-23, 2013; San Diego, CA. Abstract P01.172. Trials in Progressive MS • Secondary Progressive MS – ASCEND: Natalizumab vs Placebo – Siponimod vs Placebo • Primary Progressive MS – FREEDOMS: Fingolimod vs Placebo – ORATORIO: Ocrelizumab vs Placebo Choice of Therapy Aggressive Disease? Aggressive Disease? Yes JCV AB Positive? NTZ ? No JCV AB Negative Fingo DMF Safest NTZ GA IFN Pregnancy? Non-injection GA INSURANCE Teri ?DMF ?Fingo ?NTZ Immunopathogenesis of MS Fampridine K+ CD8 CTL Reg GA Olig o Glutamate CD8p IL-10 TGFb B7 CD28 MCP-1 MIP-1a IP-10 RANTES Th1 DC Th17 CCL20 IL-17 CCR6 Th17 Treg CD40 CD40L Foxp3 IL-6 Treg Foxp3 Th17 S1Pr IL-6 & IL1-ß Th0 Dhib-Jalbut S. 2013. Tr1 Th3 IFNB GA Treg Foxp3 IFNB BBB IFNg TNF S1Pr TGFß Fingolimod Rituximab VCAM-1 MMP-2/9 CD20 Natalizumab Th1 B VLA-4 IL-12 Th0 TF TCR B7-CD28 GA S1Pr Astrocyte ICAM-1 IL-23 EBV B IFNg TNF Neut Ab+C9neo PL RNO ROS TNF MMP BG-12 S1Pr CD8 FcR Epitope spreading Tr1 Th3 IL-4 IL-5 IL-10 IL-13 TGF-b GA Th2 TLR HLA Th0 APC Myelin Ag Microbial Ag BG-12 IL-4 IFN-ß BIOMARKERS Defining Interferon ß Response Status in MS • 15-year follow-up of pivotal MSCRG trial for weekly interferon • 172 patients in placebo-controlled IFN-ß1a trial x 2 years • In IFNb-1a group, disease activity predicted EDSS worsening: – Gadolinium-enhancing lesions (OR, 8.96; P<0.001) – Relapses (OR, 4.44; P=0.01) – New T2 lesions (OR, 2.90; P=0.08) • Conclusion: New MRI activity during IFN-ß1a treatment correlates with suboptimal response Rudick RA et al. Ann Neurol. 2004;56:546-555. Bermel RA et al. Ann Neurol. 2013;73:95-103. MRI as a Surrogate of Future Disease Activity • 370 patients underwent MRI at baseline and 1 year after beginning IFN • Followed for relapse or disability progression in years 1-4 • At year 1: ≥1 Gd enhancing lesion or ≥2 T2 lesions had same risk for worsening disease in years 1-4 and for a clinical relapse within the first year • MRI activity after starting IFN has similar implication as a relapse Prosperini L, Pozzilli C. Mult Scler J. 2013;2013:756564. Potential IFN-β Serum Biomarkers Responders Non-responders Increase in IL-10 IL-17F levels>200pg/ml Reduction in Th1 cytokines High baseline IFN-β levels Increased in neurotrophic factors Increased monocytes IFN-I secretion in response to TLR NAB Increase PSTAT1 and IFNR1 on monocytes at baseline Dhib-Jalbut S et al. J Neuroimmunology. 2013;254:131-140. Comabella M et al. Brain. 2009;132:3353-3365. Clinical Response to IFN-β Key Points • Relapses are reduced by one-third • Response is heterogeneous • No validated laboratory biomarkers • Persistent active MRI lesions at 6 mos predicts clinical activity • Persistent high titer neutralizing Ab could be a reason to switch therapy Killestein J, Polman CH. Nat Rev Neurol. 2011;7:221-228. GA-BIOMARKERS Glatiramer Acetate Binds to HLA Class II on Antigen Presenting Cells and Induces Type-2 APCs IL-4 IL-10 TGFB IL-12 TNF APC/type-2 Dendritic cells GA Th0 Th2 Treg Weber MS et al. Nat Med. 2007;13:935-943. Response by Haplotype Dhib-Jalbut S et al. MSARD. 2013;2:340-348. DR and DQ Haplotypes Predictors of Clinical Response to GA PROGNOSTIC PROFILE HAPLOTYPES NR / R (%R) Poor prognostic profile DR15 - DQ6 absent DR17 - DQ2 present 10 / 2 (16.7%) Neutral prognostic profile Good prognostic profile Dhib-Jalbut S et al. MSARD. 2013;2:340-348. DR15 – DQ6 present & DR17 – DQ2 present DR15 – DQ6 absent & DR17 – DQ2 absent DR15 – DQ6 present DR17 - DQ2 absent 17 / 11 (39.5%) 7 / 17 (70.8%) Summary of Potential GA-Biomarkers GA-RESPONDERS IL4/IFNg IL-17 IL-10 IL-18 BDNF Caspase-1 FOXP3+ DR15 DQ6 Dhib-Jalbut S. Presented at: ECTRIMS 2010. GA NONRESPONDERS DQ2 DR17 Black Holes NATALIZUMAB BIOMARKERS Defer G et al. J Neurol Sci. 2012;314:138-142. BIOMARKERS OF Rx COMPLICATIONS L-Selectin and Risk of PML in Natalizumab-treated MS Patients Schwab N et al. Neurology. 2013;81:865-871. Serum IL-21 and Autoimmunity Jones JL et al. J Clin Invest. 2009;119:2052-2061. Choosing Therapies—Biomarkers • Antibodies to aquaporin-4 • Immune markers – IL-17 and response to IFN – Alemtuzumab autoimmunity: serum IL-21 – Daclizumab: CD56Bright • Genetics/genomics (HLA): Response to GA • Neutralizing antibodies (NAB) (IFN-B, natalizumab) • JC virus exposure (natalizumab) Future Issues • Neuroprotection – how to recognize, measure, Rx • Pathologic-based phenotyping will be increasingly important for treating progressive disease, informed (targeted) repair • Biomarkers • Measures of improvement Patient Resource Tools • The National Multiple Sclerosis Society – www.nmss.org – An online resource of patient information • The American Academy of Neurology − http://patients.aan.com/go/brochures − Understanding Multiple Sclerosis (located mid-page) − Available as a downloadable PDF or printed copies can be ordered by contacting Missy Render (mrender@aan.com) Participant CME Evaluation • Please remove the Post-activity Survey and Evaluation from the back of your packet • If you are not seeking credit, we ask that you fill out the information pertaining to your degree and specialty, as well as the few questions in the Post-activity Survey measuring the knowledge and competence you have garnered from this program. • In order to receive CME credit, please complete the Evaluation Form, as well, and return to onsite staff. Your participation will help shape future CME activities. Thank You!