Therapy Considerations for the Ulnar Nerve

Innervations of the Ulnar Nerve
Sieg & Adams, Illustrated Essentials of Musculoskeletal Anatomy (1996)
Etiology
High Lesion: Proximal to elbow
Recovery of intrinsic function rare due to long distance from site of injury
Trauma
Laceration
Compressive
Cubital Tunnel Syndrome
Other
Peripheral Neuropathy (i.e.
Diabetes)
Charcot-Marie-Tooth disease Gunshot/stab wound Prolonged or repetative compression at Guyon’s Canal
(i.e. bicycling, tennis)
Fracture/dislocation Tumor
Compression at Guyon’s Canal
sportinjuriesandwellnessottawa.blogspot.com
Muscle Loss
Low: Intrinsic musculature
Palmar Interossei
Dorsal interossei
3 rd and 4 th Lumbricals
Adductor Pollicis
Flexor Pollicis Brevis (deep head)
Flexor Digiti Minimi
Opponens Digiti Minimi
Abductor Digiti Minimi
High: Intrinsic + Extrinsic musculature
Flexor Digitorum Profundus of Ring and Small
Flexor Carpi Ulnaris
Muscle Loss: Presentation
Claw hand
low nerve palsy only
Froment’s Sign
Jeanne’s Sign
Swan Neck
Boutonniere Deformity
Functional Loss
Decreased grip strengthoften as much as 60-80%
Key Pinchas much as 70-80%
Relies on the adductor pollicis, 1 st dorsal interossei, and flexor pollicis brevis for stability and strength
Froment’s Sign
Hyperflexion of the thumb IP joint during pinch
Jeanne’s Sign
Hyperextension of the thumb MP joint during pinch
Dell, P et al, JHT (2005)
www.studyblue.com
Froment’s Sign
www.ehealthstar.com
Jeanne’s Sign
Boutonniere and Swan Neck
www.merckmanuals.com
Sensory Loss
Ulnar ½ of Ring Finger,
Small finger, hypothenar eminence, and similar on dorsum of hand
Dorsal sensory branch of the ulnar nerve originates approximately 7 cm proximal to ulnar styloid www.rch.org.au
Pre-Operative Therapy
Objectives
Prepare patient, physically & psychologically, for surgery
Enable patient to be as functional as possible prior to surgery
Splinting for Function
Objectives:
Reduce MP joint hyperextension due to normal function of the EDC unopposed by the intrinsic flexors
Stability of thumb for key pinch
Hand Based:
Dorsal Knuckle Bender
Figure 8 or Lumbrical Bar
Hand based thumb spica for pinch
Thumb MP stabilizer for Jeanne’s sign
Oval 8 for Froment’s sign
Dorsal Knuckle Bender
ncmedical.com
Figure 8 or Lumbrical bar
Hand based thumb spica
MP blocking fingers & thumb
Thumb MP stabilizer
Oval 8 for IP stabilization
Splint for function
Forearm Based: if high ulnar nerve lesion may need to stabilize forearm
Ulnar gutter allegromedical.com
Splinting to Prevent or
Correct Deformity
Objective:
Prevent or reduce PIP joint contractures of ring and small fingers
Prevent or reduce Boutonniere & Swan Neck deformities
Reduce pain in thumb due to imbalance in pinch
Serial Casting
To reduce PIP contractures prior to surgery www.msdlatinamerica.com
Silver Ring Splint
For Boutonniere and Swan Neck
Functional
Adaptations/Modifications
Increase ability to complete tasks with weak pinch
Use of adaptive equipment
Elastic shoelaces
Adaptive light switch
Compensation
Modified writing position
Adaptive key pinch for car
Interventions
Maintain full PROM for involved joints
Manual Muscle Testing
Electrical Stimulation
Persistent pain management/education
Patient Education regarding realistic expectations related to function, timing, and rehab needs
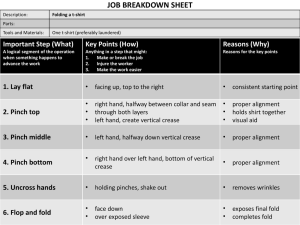
Specific Transfers and Indications
Goal to Regain From: Donor Tendon
(working)
To: Recipient
Tendon (deficient)
Adductor pollicis Thumb Adduction FDS, ECRB or ECRL, EIP, or
Brachioradialis
Finger Abduction
(index most important)
APL, ECRL, or EIP 1 st dorsal interossei
Reverse Clawing effect
FDS, ECRL (must pass volar to transverse metacarpal ligament to flex proximal phalanx)
Lateral bands of ulnar digits www.orthobullets.com
Tendon Transfers:
Thumb Adduction
Use of ECRB or ECRL w/ free tendon graft (usually Palmaris Longus) to restore Adductor Pollicis function
Advantage:
Strong motor component and avoids sacrificing finger flexor
Good excursion
Disadvantage:
Doesn’t reproduce same line of pull
Dell, P. JHT (2005); http://www.msdlatinamerica.com/ebooks/HandSurgery/sid731790.html
Tendon Transfer:
Finger Abduction
Objective: provide more stability to index during pinch than strength
Transfers typically provide 25-
50% of normal pinch strength
Dell, P. JHT (2005); http://www.msdlatinamerica.com/ebooks/HandSurgery/sid731790.html
Tendon Transfer:
Reduce clawing effect
Procedure Concept
Bunnell Release of A1 & A2 pulleys to allow flexors to bowstring, often combined with tightening of volar capsule
Zancolli Volar plate advanced proximally to produce flexion contracture of
MP
Stiles-Bunnell Splits FDS (usually MF) and transfers to radial lateral bands of RF/SF
Zancolli lasso FDS of MF, passed through A1 pulley and sutured onto self
Fowler Active tenodesis w/ 2 tendon grafts sutured to lateral bands
Must have active wrist flexion to elicit tightening for MP flexion and
IP extension
Brand ECRB or ECRL to radial lateral bands
Dell, P. JHT (2005)
Tendon Transfer:
Reduce clawing effect
Flexor digitorum superficialis (FDS) tendon transfers for correction of clawing.
The FDS can be sewn to the lateral band (A), to bone
(B), or on itself in the
Zancolli lasso (C).
http://www.msdlatinamerica.com/ebooks/HandSurgery/sid731790.html
Post Op Protocol
For Brand procedure:
3 ½ weeks post-op
Splint:
Volar routing: Dorsal Blocking splint with wrist in 30 degrees flexion, MP 60 degrees flexion, and IP neutral
Dorsal routing: Dorsal Blocking splint with wrist in 30 degrees of extension, MP blocked in 60 degrees of flexion, and IP extended
ROM
AROM w/ in splint 10 minutes every hour
Passive extension to PIP and DIP
Passive flexion-only if tendon inserted into bone; for insertion into lateral bands: no passive flexion until 6 wks due to risk of stretching out transfer
NMES to facilitate excursion
Scar Management
Indiana Hand Protocol (2001)
Post Op Protocol
6 weeks post-op
Splint
Reduced to MP block with palmar bar in 45 degrees of flexion to be worn at all times
If PIP extensor lag-continue with dorsal blocking splint
ROM
PROM to MPs, PIPs, and DIP joints
All completed within the restrains of the MP block
Indiana Hand Protocol (2001)
Post Op Protocol
7-8 weeks post-op
Dynamic flexion initiated prn
Monitor for PIP extensor lags
10-12 weeks post-op
MP blocking splint discontinued if hyperextension not present and minimal (<15 degrees) PIP extensor lag
Indiana Hand Protocol (2001)
Post Op Protocol
To ensure good excursion of long flexors, concentration on blocking exercises and use of NMES to restore flexion of FDS and FDP can be helpful
Indiana Hand Protocol (2001)
Ulnar nerve Transfers
Objective: Restore intrinsic muscle function for pinch strength, power grip, and dexterity
Options
Terminal branch of AIN to deep motor branch of ulnar nerve
Not synergistic but increases pinch/grip strength and decreases clawing
Branches of Posterior Interosseous Nerve (PIN), EDM and ECU branch, to ulnar nerve
Post-Operative Therapy
Nerve Transfer
Immobilization
Elbow/Forearm: 7-10 days
Post-op dressing
May change to splint as early as s/p 2-3 days
No further protection after 10 days due to no tension on nerve transfer
If tendon transfer at same time, protocol paradigm shift related to tendon
Moore et al, JHT (2014)
Precautions Post Operative
Tendon Transfer
Same as for Tendon repair
Nerve Transfer
Risk of increased tension on nerve repair site
Post Operative Therapy
Tendon and/or Nerve Transfer
Edema control
Scar management
Pain management
Range of Motion
Sensory Re-Education
Strengthening
Restore Function
Motor Re-education
Objective:
To correct recruitment and restoration of muscle balance and decrease compensatory patterns
Motor Re-education
Challenges:
Alterations in motor cortex mapping (i.e. neuro tag smudging)
Muscle imbalances due to weakness associated with dennervation
May persist due to compensatory movement patterns and persistent weakness of reinnervated muscles
Method:
Contract muscle from donor nerve/muscle with new muscle until motor pattern established
The more synergistic the action and based on original motor pattern, the more recruitment and establishment of muscle balance
Cortical Re-Mapping
Cortical Re-mapping
Graded motor imaging
Left/Right discrimination
Explicit Motor Imagery
Mirror Therapy
Patient Education
Sensory Re-education
VibrationClapping
StereognosisContact particles
Sensory Re-Education
Light to deep Touch blog.physiotek.com
Exercise
ROM
PROM
Place and Hold with visualization
AROM through full range
Opposition exercises
Light object pick-up
Marble cup
3 poker chips
Strengthening
Graded putty exercises
Button find
Pushing golf tees in putty
Tearing paper
Exercise
Strengthening
Putty Exercises for grip and pinch
Bibliography
Cannon, N, et al. Diagnosis and Treatment manual for Physician and Therapists. Upper Extremity Rehabilitation, 4 th edition.
Indianapolis. 2001.
Davis KD, Taylor KS, Anastakis DJ. Nerve Injury Triggers Changes in the Brain. Neuroscientist. 2011; 17 (4).
Dell PC, Sforzo CR. Ulnar Intrinsic Anatomy and Dysfunction.
Journal of Hand Therapy. April-June 2005; 2:198-207.
Hoard AS, Bell-Krotoskie JA, Mathews R. Application of
Biomechanics to Tendon Transfers. Journal of Hand Therapy. April-
June 1995; 115-123.
Moore AM, Novak CB. Advances in nerve transfer surgery. Journal of Hand Therapy. April-June 2014; 27: 96-105.
Bibliography
Moseley GL, Butler DS, Beames TB, Giles TJ. The Graded
Motor Imagery Handbook. Adelaide, Australia. Noigroup
Publications. 2012.
Sieg & Adams. Illustrated Essentials of Musculoskeletal
Anatomy, 3 rd Edition. Gainesville, Megabooks, Inc. 1996.
Sultana SS, MacDermid JC, Grewal R, Rath S. The effectiveness of early mobilization after tendon transfers in the hand: A systematic review. Journal of Hand Therapy. October 2013;
26: 1-21.
Wang JHC, Guo Q. Tendon Biomechanics and
Mechanobiology-A minireview of basic concepts and recent advancements. Journal of Hand Therapy. April-June 2012; 7:
133-140.