Case Studies - Michigan Academy of Physician Assistants
advertisement
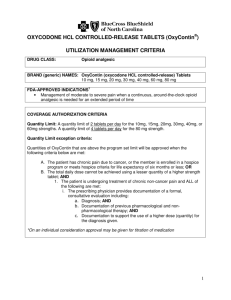
Opioid Case Studies: Putting Theory into Practice David A. Cooke, MD, FACP University of Michigan Health System Departments of Internal Medicine and Anesthesia Dr. Cooke has no financial interests relevant to this presentation. He has no relationships to the makers of any drugs discussed in his talks. Many thanks to Dr. Daniel Berland for his assistance and material contributed to this presentation Case 1 45 y/o man new to you, his former doc, Dr. Feelgood, recently “left practice” and he will soon need refills. History of fairly good health, but chronic headaches, neck pain and spasms 5 years after a MVA. No hx surgery or PT. Pain managed well on meds. He works parttime, smokes cigarettes. Asking for Soma 350 mg – 1 TID, OxyContin 80 mg BID and Vicodin 5/500 – 2 QID. Exam – NAD, friendly, non-specific exam. What would you do for him at this first visit? A) Prescribe the medications so that he doesn’t go through withdrawal. B) Prescribe the OxyContin, but not Soma. C) I would tell him “I don’t kiss on the first date.” D) I would rotate his opioids to methadone. What would you do for him at this first visit? A) Prescribe the medications so that he doesn’t go through withdrawal. B) Prescribe the OxyContin, but not Soma. C) I would tell him “I don’t kiss on the first date.” D) I would rotate his opioids to methadone. Before that first kiss: 1) 2) 3) 4) Check MAPS. Check urine toxicology. Check records. Establish use agreement and expectations. Current Regimen: • Soma 350 mg – 1 TID • OxyContin 80 mg BID • Vicodin 5/500 – 2 QID Which of the following is true? • A) Soma is functionally a barbiturate, and is commonly abused. • B) Soma has been proven effective for treatment of ACUTE back pain. • C) Soma has been proven effective for treatment of CHRONIC back pain. • D) B and C Which of the following is true? • A) Soma is functionally a barbiturate, and is commonly abused. • B) Soma has been proven effective for treatment of ACUTE back pain. • C) Soma has been proven effective for treatment of CHRONIC back pain. • D) B and C Current Regimen: • Soma 350 mg – 1 TID • OxyContin 80 mg BID • Vicodin 5/500 – 2 QID Which of the following are true? • A) Oxycontin provides superior pain control, relative to other long-acting opiates. • B) Oxycontin is cost-effective relative to other long-acting opiates • C) Oxycontin is a preferred long-acting opiate per the UM Chronic Pain guideline • D) B and C • E) None of the above Which of the following are true? • A) Oxycontin provides superior pain control, relative to other long-acting opiates. • B) Oxycontin is cost-effective relative to other long-acting opiates • C) Oxycontin is a preferred long-acting opiate per the UM Chronic Pain guideline • D) B and C • E) None of the above Monthly cost of opiates • • • • Morphine ER 60 mg BID – $51.83 Fentanyl ER 50 mEq/hr – $295.58 Methadone 5 mg TID – $13.58 Oxycontin 40 mg BID – $501.11 Drug prices 3/2013 at UMMC pharmacies What is the street value for the monthly supply of his OC 80 mg #60, Vic 5 #120 ? A) B) C) D) $ 240 $ 900 $ 1,800 $ 3,400 What is the street value for the monthly supply of his OC 80 mg #60, Vic 5 #120 ? A) B) C) D) $ 240 $ 900 $ 1,800 $ 3,400 Current Regimen: • Soma 350 mg – 1 TID • OxyContin 80 mg BID • Vicodin 5/500 – 2 QID “Breakthrough Pain” in Chronic Pain • A) is common, and patients should have PRN doses of short-acting opiates • B) is indicative of medication abuse • C) may not exist • D) should not require more than 5-10 PRN doses per month • E) C and D “Breakthrough Pain” in Chronic Pain • A) is common, and patients should have PRN doses of short-acting opiates • B) is indicative of medication abuse • C) may not exist • D) should not require more than 5-10 PRN doses per month • E) C and D Before you commit: • • • • • Is he really benefitting from the meds? Level of function? Any evidence of medication toxicity? Why no non-medication therapies? Psychological issues? Next Steps? • Stop Soma • Consolidate opiates; don’t prescribe scheduled Oxycontin + Vicodin • Enroll in PT • Slow medication taper; MAXIMUM of 120 mg/day morphine equivalent • Continue to monitor frequently Case 2 • 44 y/o M with a history of low back pain radiating to left leg, present since motorbike injury at age 24. • On opiates for approximately 20 years; now taking methadone 60 mg QID. • PMH significant for depression, anxiety, and substance abuse; denies current drug use. • Unemployed, lives with parents. No hobbies, volunteering, or social activities. Case 2 Continued • States at visit, “I feel like my body is falling apart. I hurt all over.” Pain is 6/10 at best, 10/10 at worse, 8/10 most of the time. • Exam: Appears tearful and depressed. Moves slowly. Diffusely tender to palpation over lower back and left leg. • MAPS shows no other prescribers • Urine tox shows prescribed medications What is the strongest indication to change his regimen? A) Total daily methadone dose of 240 mg/day B) 8/10 pain most of the time C) Prior history of drug abuse D) Signs of depression E) Low level of function What is the strongest indication to change his regimen? A) Total daily methadone dose of 240 mg/day B) 8/10 pain most of the time C) Prior history of drug abuse D) Signs of depression E) Low level of function Benefits must outweigh risks! • Patient is on a massive dose of methadone; maximum UM recommended dose 40 mg/day! • Diffuse pain suggests opiate-induced hyperalgesia • Despite extraordinary opiate doses, patient is almost completely nonfunctional. Ok, but now what? • Have an honest talk with the patient about risk and benefits from treatment • Be clear that intent is not punitive • Plan a gradual taper, with frequent followup • Set targets for increasing activities and socialization. • Mental health interventions Case 3 • 48 y/o F with chronic low back pain x 15 years following laminectomy, and fibromyalgia x 3 years, on methadone 10 mg TID, complains of worsening pain in back, as well as aching in arms, legs, and all of her joints. Symptoms worsening gradually over the past year. No fevers, sweats, or weight loss. • Exam shows diffuse lumbar tenderness to palpation, tenderness of muscles, and classic fibromyalgia “trigger points”. Normal strength, no muscle or joint abnormalities beyond pain, and no objective arthritis. • Complete rheumatologic workup including ANA, RF, ESR, CRP, TSH, and CK are entirely normal. At this point, which is most likely to improve this patient’s pain? A) Increase methadone dose B) Decrease methadone dose C) Start duloxetine D) Start nortriptyline E) Start gabapentin At this point, which is most likely to improve this patient’s pain? A) Increase methadone dose B) Decrease methadone dose C) Start duloxetine D) Start nortriptyline E) Start gabapentin Opioid-Induced Hyperalgesia (OIH): • Common and under-recognized long term complication of opioid use • Mechanisms unclear • Risk increases with dose and duration • May be confused with tolerance • May be focal, or can resemble fibromyalgia; ask whether on opioids at time of fibro dx Suspect OIH if: • Worsening pain complaints in absence of change in underlying disease • Fibromyalgia diagnosis or symptoms that develop after start of opioid therapy • High dose opioids • Long duration of opioid use • Poor pain control on opioid therapy • Physical evidence of hyperalgesia Management: • Taper or discontinue opioids • Consider switching to methadone • Consider switching to buprenorphine Take Home Points • • • • • • • Don’t kiss on the first date Avoid sedatives in chronic pain Avoid medication duplication Learn opioid equivalents Limit dosages to <120 MED Assess functional benefits Recognize when opioids fail Useful Reading • UM PAIN / OPIOID GUIDELINE med.umich.edu > For Health Professionals > Clinical Guidelines • WA INTERAGENY GUIDELINE on Opioid Dosing for Chronic Non-Cancer Pain http://www.bt.cdc.gov/coca/pdf/OpioidG dline%5B1%5D.pdf or “Google” it • A COMPREHENSIVE REVIEW OF OPIOID-INDUCED HYPERALGESIA. Lee et al., Pain Physician 14:145-161 (2011).