Lidocaine and the Prevention of Emergence Phenomena
advertisement
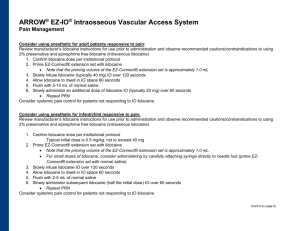
Lidocaine and the Prevention of Emergence Phenomena Ian Lynch & Daniel Parker Gonzaga University Providence Sacred Heart Medical Center March 20, 2014 Statement of Problem • A common goal of anesthesia providers is to have a smooth emergence during extubation without coughing • Emergence from anesthesia is managed differently by each anesthesia provider • Traditional methods of EP prevention including: deep extubation, IV lidocaine, LTA, and lidocaine ointment/jelly on ETT cuff • New methods of topical tracheal anesthesia may prove beneficial for reducing EP Emergence Phenomenon (EP) A phenomenon that includes coughing, sore throat, or dysphonia, or a combination of all three, as a result of an endotracheal tube cuff irritating the tracheal mucosa during emergence Purpose Statement The purpose of this study was to assess, through survey, the current professional practice among CRNAs regarding their treatment modalities for reducing emergence phenomenon (EP) for general endotracheal anesthesia in the operating room Guiding Research Questions 1. What are surveyed CRNAs doing to prevent EP? 2. To what degree are practitioners familiar with the use of lidocaine filled endotracheal tube cuff (ETTC)? 3. How does an ETTC filled with lidocaine compare to other treatment modalities? 4. What are the risks and benefits of various treatment modalities for EP? Review of the Literature • Emergence Phenomena • Postoperative sore throat is the most common complaint after endotracheal intubation (Estebe et al., 2004) • Presumed mechanisms of EP include irritation or stretch stimuli directly to the trachea from an ETT or cuff (Fegan et al., 2000) • Current treatments to avoid EP include local anesthetics via a variety of different delivery methods (Minogue, Ralph, & Lampa, 2004) Review of the Literature • Current Emergence Phenomenon Reduction Strategies • IV lidocaine 60-90 seconds prior to intubation • 1 and 1.5 mg/kg IV decreases sore throat and cough (Takekawa, Yoshimi, and Kinoshita, 2006) • 2 mg/kg IV complete cough suppression (Yukioka et al.,1985) • Superior to LTA at attenuating CV response to intubation (Youngberg, Graybar, and Hutchings, 1983), Hamill, Bedford, Weaver, and Colohan, 1981) • Prevents increases in ICP while LTA did not (Hamill, Weaver, and Colohan, 1981) Bedford, Current Emergence Phenomenon Reduction Strategies • LTA: Topical anesthesia applied prior to intubation has little to no effect on prevention of coughing during extubation (Diachun, Tunink, & Brock-Utne, 2001) • LTA: surgeries <2 hours • Decreased cough by 26% prior to extubation compared to saline spray control (Minogue, Ralph, and Martin, 2004) • LITA: Administration of four percent lidocaine via LITA, 30 minutes prior to extubation results in a significant reduction in ETT induced coughing during emergence Review of the Literature • Current Emergence Phenomenon Reduction Strategies • Lidocaine 1mg/kg down ET vs. IV three minutes prior to extubation • ET significantly decreased cough while IV did not (Jee and Park, 2003) • Lidocaine spray • Additives caused postoperative sore throat and hoarseness (Hara and Maruyama, 2005) • Jelly • Complete ET obstruction with sheet-like film (Uehira, Tanaka, Mitsugu, Oda, and Sato, 1981) • Sore throat worse than saline (85 vs 62%) (Klemola, Saaenivaara, and Yrjola, 1988) Review of the Literature • Alkalized Lidocaine filled ETTC • Time: 60 minutes or longer of alkalized lidocaine filling the ETT is required for noticeable cough suppression (Fagan et al., 2000) • Addition of Sodium Bicarbonate: By increasing the pH of a solution, you can predictably increase the percentage of the non-ionized fraction of the drug • Lidocaine Concentration: Low doses of lidocaine, even as low as 40 mg, with the addition of bicarbonate, showed better outcomes with EP prevention when compared to higher dose, non-alkalinized solutions (Estebe et al, 2005) • Efficacy and Safety: Lower concentrations of sodium bicarbonate are equally as effective as using the higher dose of 8.4% and are safer Methodology • Qualitative study • Survey created utilizing SurveyMonkey • Survey distributed to CRNAs via state associations of nurse anesthetists • Participating states: AZ, CA, CO, DC, ID, KS, KY, MA, MO, MT, OK, OR, RI, SC, TN, TX, UT, VA, WA • All 50 state associations were invited to participate Findings Findings Findings Findings Findings n=9 Findings Recommendations • ETTC filled with alkalized lidocaine has been shown to prevent EP more effectively that other techniques as well as be a safe alternative • Providers should use a manometer each time they fill the ETTC • Achieve correct occlusive cuff pressure using air • Remove and measure the amount of air required to reach said pressure and record this number • Add 2mls of 2% lidocaine • Add 1-2mls of sodium bicarbonate • Add as much NS as is required to match the cuff volume withdrawn to reach desired or occlusive pressure References • Diachun, C. A., Tunink, B., & Brock-Utne, J. G. (2001). Suppression of Cough During Emergence From General Anesthesia: Laryngotracheal Lidocaine Through a Modified Endotracheal Tube. Journal of Clinical Anesthesia, 13, 447-450. • Estebe, J. P., Delahaye, S., Le Corre, P., Dollo, G., Le Naoures, A., Chevanne, F., & Ecoffey, C. (2004). Alkalinization of intra-cuff lidocaine and use of gel lubrication protect against tracheal tube-induced emergence phenomena. British Journal of Anaesthesia, 92, 361-366. http://dx.doi.org/10.1093/bja/aeh078 • Estebe, J. P., Gentili, M., Le Corre, P., Dollo, G., Chevanne, F., & Ecoffey, C. (2005). Alkalinization of Intracuff Lidocaine: Efficacy and Safety. Anesthesia and Analgesia, 101, 1536-1541. • Fagan, C., Frizelle, H., Laffey, J., Hannon, V., Carey, M. (2000). The Effects of Intracuff Lidocaine on Endotracheal-Tube-Induced Emergence Phenomena after general anesthesia. Anesthesia and Analgesia, 91, 201-205. • Hamill, J. F., Bedord, R. F., Weaver, D. C., Colohan, A. R. (1981). Lidocaine before Endotracheal Intubation: Intravenous or laryngotracheal? Anesthesiology, 55, 578-581. References • Hara, K., & Maruyama, K. (2005). Effect of additives in lidocaine spray on postoperative sore throat, hoarseness and dysphagia after total intravenous anaesthesia. Acta Anaesthesiologica Scandinavica, 49, 463-467. • Jee, D., & Park, Y. (2003). Lidocaine sprayed down the endotracheal tube attenuates the airway-circulatory reflexes by local anesthesia during emergence and extubation. Anesthesia & Analgesia, 96, 293-297. • Klemola, U., Saaenivaara, L., Yrjola, H. (1988). Post-operative sore throat: effect of lignocaine jelly and spray with endotracheal intubation. European Journal of Anaesthesiology, 5, 391-399. • Minogue, S. C., Ralph, J., & Lampa, M. J. (2004). Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesthesia & Analgesia, 99, 1253-1257. • Takekawa, K., Yoshimi, S., & Kinoshita, Y. (2006). Effects of intravenous lidocaine prior to intubation on postoperative airway symptoms. Journal of Anesthesia, 20, 44-47. • Uehira, A., Tanaka, A., Mitsugu, O., Sato, T. (1981). Obstruction of an endotracheal tube by lidocaine jelly. Anesthesiology, 55, 598-599. • Youngberg, J. A., Graybar, G., Hutchings, D. (1983). Comparison of intravenous and topical lidocaine in attenuating the cardiovascular responses to endotracheal intubation. Southern Medical Journal, 76, No. 9, 1122-1124. Thank you for your time