Complication Rates for Fluoroscopic Guided Interlaminar
advertisement

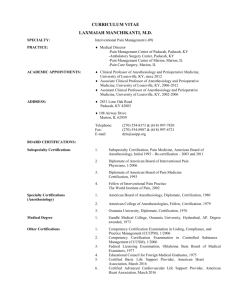
Complication Rates for Fluoroscopic Guided Interlaminar Lumbar Epidural Steroid Injections: Certified Registered Nurse Anesthetists and Physicians Dr. Donald E. Beissel, DNP, CRNA, DAAPM Southwest Interventional Pain Specialists Objectives -Discuss the prevalence of chronic spine related pain in the USA -Discuss financial and logistical impediments to access to chronic pain care for rural and elderly patients -Describe the study method of the topic at hand -Describe the complication rates of CRNAs and Physicians when providing fluoroscopic guided LESIs -Describe the implications of this research on rural and elderly patients in need of chronic pain care and the providers who are willing to provide that care -Describe the direction of future research Why study this? What SB 682 Meant No Fluoroscopy guidance for CRNAs… No Kyphoplasty… No Radio Frequency Ablation… No Implanted devices… until August 28, 2016- Sunset We were given 4 years to get evidence and education programs in order. Review of the Literature The Cost of Low Back Pain Back pain is the leading cause of disability in the world (Crow and Willis, 2009). Respiratory illness is the only complaint that accounts for more missed work time. Two thirds of of people will experience low back pain (LBP) in their lives. LBP costs $100 billion/year in the USA (Pizzo & Clark, 2012). Providers There are fewer than 4,000 physician pain management providers in the USA (Pizzo and Clark, 2012). Multiple physician specialties and advanced practice RNs (including Certified Registered Nurse Anesthetists) have billed Medicare for fluoroscopy guided pain management procedures since at least 1998 (Manchikanti, 2004). “Providing acute and chronic pain management and treatment is within the professional scope of practice of CRNAs. CRNAs employing pain management techniques is neither new nor unusual and has long been a part of CRNA practice. By virtue of education and individual clinical experience, a CRNA possesses the necessary knowledge and skills to employ therapeutic, physiological, pharmacological, interventional, and psychological modalities in the management and treatment of acute and chronic pain. The AANA believes that it is incumbent upon the individual CRNA to assure his or her competency when delivering anesthesia services, including pain management and treatment.” (AANA, 1994) Manchikanti Study Manchikanti, et al. studied complication rates for 10,000 consecutive fluoroscopic guided injections near the spine in 2012. Fourteen hundred and fifty of these were interlaminar LESIs. Low complication rate. Basis of comparison for this study. Published Complication Rates There are no complication rate studies for CRNAs providing fluoroscopic guided pain procedures. American Society of Anesthesiologists closed claims study. One hundred and fourteen epidural steroid injection complications-total performed unknown (Fitzgibbon, et al.) McGrath, Schaefer, & Malkamaki (2011) found a complication rate of 0.6%, but only studied 123 Lumbar Epidural Steroid Injections (LESIs). Access and Cost The Lewin Group examine four case studies of rural pain patients in 2012. They compared the cost of care by a local CRNA to traveling to a physician for injections, having surgery, and having no care at all. They found that cost saving and increased quality of life were associated with treatment by the local CRNA over the other options. Purpose What did this study do? I explored whether or not CRNAs have complication rates similar to physicians when performing fluoroscopic guided interlaminar LESIs. I studied one procedure to establish the methods to study all fluoroscopic guided procedures in the future. This procedure was chosen because it is commonly performed by both CRNAs and physicians (Manchikanti, 2004; Manchikanti, Helm, Singh, & Hirsch, 2014). I also studied cost by determining distance from the CRNA participants to the closes physician pain provide. I tracked participant satisfaction to determine if the providers were satisfied with the data collection process. Study Design and Methods Recruitment Participants were recruited from across the USA via online pain management discussion boards with over 1,000 members. Twenty-seven expressed interest. Nineteen enrolled. Thirteen completed all phases of data collection. Demographics Participants were surveyed about education, experience, and their practice situations. Procedural Complications Six month collection period on an Excel spreadsheet. Number of procedures. Incidence of 20 different complications. Participant Satisfaction Participants were asked to respond to: “the data was easy to collect while performing clinical duties”, “the study was the right length of time”, “the study has value for CRNA pain management practice”,” it was easy to contact the lead researcher with questions about the study” and “I am willing to be a subject/collect data for future studies of a similar nature.” Results Participant Demographics *Skewed by the 3 practices in urban areas. Mean is 9,164 after the urban sites are removed. **Mean distance to physician provided injections is 97.5 miles when the 3 urban participants are removed. Other Results 8 providers have Master’s Degrees 5 Providers have Doctoral Degrees (DNP, DNAP, PhD, or EdD) 3 Providers performed the procedures in an office, 1 was in a pain clinic, 8 were in hospitals, and 1 provider worked in both a hospital and a surgery center. There were 3 female CRNAs and 10 male CRNAs. Complication Rates Participant Satisfaction Limitations What? It wasn’t perfect? I could not obtain the definitions that Manchikanti, et al. (2012b) used in their study. I used standard, widely accepted definitions of complications. Complication rates between groups in this study may be due to differences in definitions. This procedure only examines one of many fluoroscopic guided injections performed near the spine. That study comes next! Direction of Future Research The Future… A bigger study with all of the fluoroscopic guided injections. Application for AANA Post-Doctoral Fellowship Creation and maintenance of a complications database for CRNAs doing fluoroscopic guided procedures. Use of this data to define safety to guide legal and policy discussions around procedures and patient safety. Steps to advance access to CRNA provided pain care Council on Accreditation of Nurse Anesthesia Programs Fellowship in Chronic Pain Management at Hamline University AANA Professional Practice Guidelines for CRNAs Providing Chronic Pain Care NBCRNA Non Surgical Pain Management Specialty Certification This dissertation and future complication studies. Discussion What about… Three participants practice in large metropolitan areas, skewing population and distance results. When discussing rural access, these distance numbers should be excluded. Differences in rates between physicians and CRNAs are likely due to differences in definition, but it is impossible to know. Vasovagal reaction differences may be due to lack of or provision of sedation during procedures. This variable should be included in the next study. Provider Diversity The physician group was made up of three anesthesiologists who all practice in the same group. The CRNA participants had diverse levels of education, CRNA experience, pain injection experience, injection performance frequency, and practice setting. None of the complications were correlated with any of the CRNA demographics. This refutes claims that CRNAs have higher complication rates due to training and education (Manchikanti, 2012a). What about “Paralysis and Death” There were no episodes of patient paralysis or death in either study group. There were 3,238 combined procedures by both groups of providers in this study. This suggests that this procedure is safe when performed by members of either profession. Implications for Practice How do we apply this? This project addressed the ethical issue of access to and distribution of care. The current pain management system is primarily comprised of physician providers in populated urban areas and non-physician providers, including CRNAs, practicing primarily in rural areas with financially disadvantaged patients. (The Lewin Group, 2012). Rural and disadvantaged patients have difficulty traveling to, or paying for physician provided pain care. Because this study found that CRNAs providing fluoroscopic guided LESIs do not have a higher complication rates than physicians on 18 of 20 complications, and physicians have published low fluoroscopic guided injection complication rates (Botwin, et al, 2000, 2003, and 2006; Manchikanti et al., 2012b), we encourage providers to continue to offer CRNA provided fluoroscopic guided procedures, rather than forcing patients to choose between traveling great distances and going without care. We also encourage legislative and regulatory action to ensure access to these procedures for underserved patient populations. Acknowledgements Dr. Mary Mackenburg-Mohn, PhD, RN, PNP Friend, mentor, and invaluable advocate for this project. She encouraged me to pursue the DNP and to choose Brandman University. I have known Mary since I was a brand new EMT in 1991 and my life is richer for knowing her. Dr. Mary Mays, PhD-An invaluable resource on design and voice of this project with fantastic insight on how to tell the story. I speak for my entire cohort in thanking her for her guidance. AANA Foundation-This study was funded, in part, by a Doctoral Fellowship from the American Association of Nurse Anesthetists Foundation. References American Association of Nurse Anesthetists Board of Directors. (1994). AANA position statement 2.11, Pain Management. Retrieved from http://www.aana.com/resources2/professionalpractice/Pages/AANA-Position-Statements,-Advisory-Opinions,and-Considerations.aspx American Association of Nurse Anesthetists Board of Directors. (2011). AANA position statement 2.11, Pain Management. Retrieved from http://www.aana.com/resources1/professionalpractice/Pages/AANA-Position-Statements,-Advisory-Opinions,and-Considerations.aspx Botwin, K. P., Baskin, M., & Rao, S. (2006). Adverse effects of fluoroscopically guided interlaminar thoracic epidural steroid injections. American Journal of Physical Medicine and Rehabilitation, 85(1), 14-23. http://dx.doi.org/10.1097/01.phm. 0000184475.44853.82 Botwin, K. P., Castellanos, R., Rao, S., Hanna, A. F., Torres-Ramos, F. M., Gruber, R. D.,...Fuoco, G. S. (2003). Complications of fluoroscopy guided interlaminar cervical epidural injections. Archives of Physical Medicine and Rehabilitation, 84, 627-633. http://dx.doi.org/10.1016/S0003-9993(03)04863-1 Botwin, K. P., Gruber, R. D., Bouchlas, C. G., Torres-Ramos, F. M., Hanna, A., Rittenberg, J., & Thomas, S. A. (2001). Complications of fluoroscopically guided caudal epidural injections. American Journal of Physical Medicine and Rehabilitation, 80, 416-424. Crow, W. T., & Willis, D. R. (2009). Estimating cost of care for patients with acute low back pain: A retrospective review of patient records. Journal of the American Osteopathic Association, 109(4), 229-33. Dulisse, B., & Cromwell, J. (2010). No harm found when nurse anesthetists work without supervision by physicians. Health Affairs, 29(8), 1469-1475. Fink, G. E. (2009). Radiation safety in fluoroscopy for neuroaxial injections. AANA Journal, 77, 265-9. Fitzgibbon, D. R., Posner, K. L., Domino, K. B., Caplan, R. A., Lee, L. A., & Cheney, F. W. (2004). American Society of Anesthesiologists closed claims project. Anesthesiology, 100, 98-105. Institute of Medicine. (2011a). Relieving pain in America: A blueprint for transforming prevention, Care, education and research (). Washington, DC: Government Printing Office. Institute of Medicine. (2011b). The future of nursing: Leading change, advancing health (). Washington, DC: Government Printing Office. Manchikanti, L. (2004). The growth of interventional pain management in the new millennium: A critical analysis of utilization in the medicare population. Pain Physician, 7, 465-82. Manchikanti, L., Helm II, S., Singh, V., & Hirsch, J. A. (2013). Accountable interventional pain management: A collaboration among practitioners, patients, payers, and government. Pain Physician, 16, E635-E670. Retrieved from www.painphysicianjournal.com Manchikanti, L. M., Caraway, D. L., Falco, F. J., Benymin, R. M., Hansen, H., & Hirsch, J. A. (2012a). CMS proposal for interventional pain management by nurse anesthetists: evidence by proclamation with poor prognosis. Pain Physician, 15, E641-E664. Manchikanti, L., Malla, Y., Wargo, B. W., Cash, K. A., Pampati, V., & Fellows, B. (2012b). A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician, 15, 131-140. McGrath, J. M., Schaefer, M. P., & Malkamaki, D. M. (2011). Incidence and characteristics of complications from epidural steroid injections. Pain Medicine, 12, 726-731. Pizzo, P. A., & Clark, N. M. (2012, January 19, 2012). Alleviating suffering 101-Pain relief in the United States. The New England Journal of Medicine, 366, 197-199. Retrieved from http://www.nejm.org/doi/full.10.1056/NEJMp1109084? viewType=Print&viewClass=Print The Lewin Group. (2012). Cases: Cost of alternative pain management paths; Final report. Retrieved from http://www.lewin.com/ publications.publication.201208140454