Mesenchymal Stem Cells
advertisement

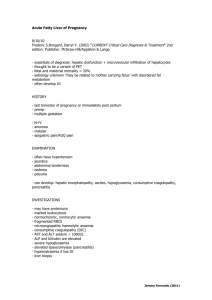
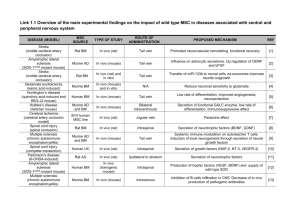
XXV Convegno A.I.R.T. Torino, 3-4 aprile 2014 Cellule staminali epatiche: realtà attuale e sviluppi futuri Renato Romagnoli Chirurgia Generale 2 U - Centro Trapianto Fegato “E.S.Curtoni” Direttore : Prof. M. Salizzoni A.O.U. Città della Salute e della Scienza di Torino Università degli Studi di Torino Chirurgia Trapianto Fegato: Prof. M. Salizzoni R. Romagnoli D. Patrono N. Gilbo P. Strignano A. Brunati Radiologia: D. Righi G. Isolato C. Gazzera MBC LAB: Prof. G. Camussi M. B. Herrera Malattie Metaboliche: S. Bruno M. Spada F. Collino V. Fonsato CRRT Piemonte: C. Cavallari Prof. A. Amoroso M.C. Deregibus Oncoematologia Pediatrica: F. Antico Fresenius Medical Care: Prof. C. Tetta Prof.ssa F. Fagioli Hepatocyte Transplantation A ‘proof of concept’ for cell therapies in: • inherited metabolic liver diseases • acute liver failure • acute-on-chronic liver failure Hepatocyte Transplantation in inherited metabolic liver diseases Technique Isolation and cryopreservation of mature hepatocytes from deceased donor organs Repeated infusions of hepatocyte suspensions in portal vein (portal catheterization) Average quantity of cells per infusion: 100 X 106 / kg Number of infusions per trial: 2 6 Hepatocyte Transplantation in inherited metabolic liver diseases Technique Isolation and cryopreservation of mature hepatocytes from deceased donor organs Repeated infusions of hepatocyte suspensions in portal vein (portal catheterization) Average quantity of cells per infusion: 100 X 106 / kg Number of infusions per trial: 2 6 Results 40 patients treated (1998-2012) urea cycle disorders: - CPS deficiency - OTC deficiency - ASS deficiency - ASL deficiency type I glycogenosis type I Crigler-Najjar hypercholesterolemia Metabolic correction Possible ‘bridge’ to organ transplant No portal thrombosis reported Hepatocyte Transplantation Drawbacks and Limits • mature hepatocytes DO NOT proliferate in culture • scarce availability and yield (cells usually isolated from low quality livers, discarded from organ transplantation) • poor viability and quality of cryopreserved cells • need of immunosuppressive therapy • limited durability of engrafted cells: 3 12 months (for rejection or natural cell exhaustion and loss) • need of repeated infusions Properties of Stem Cells • Cells capable of dividing and renewing (proliferation and self-renewal) • Cells that have the potential to give rise to specialized cell types (differentiation) • Cells that have the capacity to “repair” damaged tissues (regeneration) Types of Stem Cells • Embryonic Stem Cells (ESC): derived from 4-5 day-old blastocyst • Adult Stem Cells (ASC): identified after accomplished organogenesis in many organs and tissues, such as bone marrow, muscles, peripheral blood, umbilical cord blood, amniotic fluid, blood vessels, skin, fat, teeth, heart, gut, liver, kidney, ovarian epithelium, testis, etc • Induced Pluripotent Stem Cells (iPSC): fibroblasts could be reprogrammed by viral transfection into a pluripotent state similar to that observed in ESC through ectopic expression of four genes (Oct3/4, Sox2, c-Myc, and Klf4) Stem cells in liver diseases ESC Expansion and/or iPSC ASC Bioartificial liver device Differentiation Transplant Stem cells in liver diseases ESC Expansion and/or iPSC ASC Bioartificial liver device Differentiation Transplant Mesenchymal Stem Cells (MSC) in acute liver injury • Bone marrow MSCs • Mesenchymal stem cell-derived molecules reverse fulminant hepatic failure. Parekkadan B et al. PLoS One, 2007; 2 (9): e941 • Immediate intraportal transplantation of human bone marrow mesenchymal stem cells prevents death from fulminant hepatic failure pigs. Li J. Hepatology, 2012; 56: 1044-1052 • Amniotic fluid MSCs • Therapeutic potential of a distinct population of human amniotic fluid mesenchymal stem cells and their secreted molecules in mice with acute hepatic failure. Zagoura DS et al. Gut, 2012; 61 (6): 894-906 • Amniotic-fluid-derived mesenchymal stem cells overexpressing interleukin-1 receptor antagonist improve fulminant hepatic failure. Zheng YB et al. PLoS One, 2012; 7 (7): e41392 • Umbilical Cord MSCs • Systemic administration of a novel human umbilical cord mesenchymal stem cells population accelerates the resolution of acute liver injury. Burra P et al. BMC Gastroenterology, 2012; 12: 88 Problems inherent to MSC-based therapy The heterogeneity of MSC populations may render difficult: • the evaluation of the potency of different MSC preparations • the comparison of different clinical trials Potential complications: • the intravenous administration of MSCs may induce formation of pulmonary emboli or infarctions • tumorigenesis and maldifferentiation Problems inherent to MSC-based therapy Maldifferentiation in experimental animal models: - MSCs injected in the ischemic heart may in the long-term differentiate into bone Breitbach et al. Blood 2007 - In the anti-Ty-1-induced glomerulonephritis, MSCs in the longterm differentiate into adipocytes favoring development of a chronic renal failure Kunter et al. J Am Soc Nephrol 2007 - After lung irradiation, MSCs favor fibroblast and myofibroblast accumulation in focal pulmonary areas Epperly MW Am J Respir Cell Mol Biol 2003 The blue stars indicate sites at which there are high numbers of peribiliary glands, the stem cell niches of the biliary tree Adapted from Turner R et al, Hepatology, 2011; 53: 1035-1045 Intrahepatic maturational lineages Adapted from Turner R et al, Hepatology, 2011; 53: 1035-1045 Stem cells in human liver Human biliary tree stem cells (hBTSCs): a multipotent cell lineage capable of differentiating in cholangiocytes, hepatocytes and pancreatic islets; EpCAM+, NCAM+, CD105-, CD133+, CK19+(?), AFP-, ALB- Human hepatic stem cells (hHpSCs): liver resident precursors of hepatoblasts; EpCAM+, NCAM+, ICAM-1-, CD105-, CD133+, CK19+, AFP-, ALB± Hepatoblasts: isolated by MACS (Magnetic-activated cell-sorting) mostly from fetal and neonatal livers, but present also in adults; a bipotential cell lineage capable of differentiating into both cholangiocytes and hepatocytes; EpCAM+, NCAM-, CD105-, CD133+, CK19+, AFP+, ALB+ Human adult Liver derived Stem Cells (HLSCs): adult liver resident MSCs; EpCAM-, NCAM-, CD105+, CD133- , CK19-, AFP+, ALB+ The discovery a-MEM/EBM + 10% FCS + hEGF + hFGF Enzymatic dissociation Hepatocytes 15 days Human Liver Stem Cells Stem cell population from adult human liver Hepatic markers ? YES albumin α FP CK8 Mesenchymal Stem Cell markers ? YES CK18 vimentin nestin musashi Haemopoietic markers ? NO Embryonic Stem Cell markers ? YES nanog SSEA4 pax2 octa4 Herrera et al., STEM CELLS 2006 Differentiation capabilities Osteogenic differentiation Calcium deposits osteopontin osteocalcin Insulin-secreting cells NO adipogenic differentiation Endothelial cells Mature Hepatocytes Herrera et al., STEM CELLS 2006 Differentiation of HLSC into mature hepatocytes Monolayer or +HGF/FGF4 15 days α FP CK8/CK18 Cytochrome P450 Incorporation and complete release of Indocyanin green albumin urea Herrera et al., STEM CELLS 2006, Fonsato et al., TISSUE ENG 2010 US patent number: 2010/0003752 Publications Urea cycle disorders – Rare diseases glutamate Acetyl-Coa N-acetylglutamate NH3 HCO3 Orotic acid + 2 ATP CPS carbamoylphosphate 2 ADP L-ornithine UREA OTC citrulline ASS L-arginine Arginino-succinate ASL EU orphan designation Investigational Medicinal Product Dossier (IMPD) The Investigational Medicinal Product Dossier is the basis for approval of clinical trials by the competent authorities in the E.U. An IMPD is requested whenever the performance of a clinical study in any one of the EU Member States is intended. The IMPD includes information related to the • quality • manufacture • control of the Investigational Medicinal Product • data from non-clinical studies and from its clinical use • an overall risk-benefit assessment • critical analyses of the non-clinical and clinical data in relation to the potential risks and benefits of the proposed study Pre-clinical studies for IMPD In vitro PHARMACODYNAMICS To assess the pharmacological effect of HLSC in liver damage In vivo PHARMACOKINETICS In vivo To evaluate the biodistribution of HLSC after injection Disease models Healthy models (SCID mice) (SCID and nude mice and rats) TOXICOLOGY To find a safe first dose, to identify potential target organs for toxicity and to assess potential tumorigenicity Good manufacturing practice (GMP)-grade production of HLSC • GalN/LPS induced mouse model of hepatic failure • N-Acetyl-p-aminophen induced mouse model of acute liver injury Different administration routes: • Intravenous • Intra-parenchyma • Intra-portal In vivo Different doses and modality of administration Pharmacodynamics Regenerative potential of HLSC in a model of acute liver injury (induced by N-acetyl-p-aminophen) in SCID mice 7 days 35 days Human HLA-I Human HLA-I Mouse β-μglob Human HLA-I Human HLA-I FISH Human HLA-I Control serum 35 days FISH 35 days Not injured liver + HLSC Herrera al, STEM CELLS, 2006 Pharmacodynamics T=0 GalN/LPS after 30’ 2x106 (6x0.33) sacrifice • • • • • 7 hours 24 hours 3 days 7 days 21 days 0.2-0.5 x106 Herrera et al., HEPATOLOGY 2013 Pharmacodynamics Herrera et al., HEPATOLOGY 2013 Pharmacodynamics APOPTOSIS PROLIFERATION Herrera et al., HEPATOLOGY 2013 Pharmacodynamics In vivo differentiation of HLSC Timepoint n° HLA+ cells/hpf % of HLA+/CK8+ CK18+ cells 24 hours 20.1±16.1 2.5% 7 days 16.8±8.9 88% 21 days 12.6±3.3 48% Herrera et al., HEPATOLOGY 2013 Pharmacokinetics BIODISTRIBUTION model N-Acetyl-p-aminophen species SCID mice with FHF Healthy SCID mice GalN/LPS SCID mice with FHF Rats Healthy animals SCID mice Nude mice dose and route n° animals 0.2x106 i.v. 6 PBS i.v. 6 0.2x106 i.v. 6 2x106 i.v. 9 PBS i.v. 9 0.2x106 i. par. 4 0.5x106 i. par. 14 1x106 i. par. 4 PBS i. par. 2 1.8x106 i.v. (OI) 8 PBS i.par. 1 5x106 i.par. (OI) 5 PBS i.v. 2 1.8x106 i.v. (OI) 10 PBS i.par. 3 1x106 i. par. (OI) 10 Pharmacokinetics BIODISTRIBUTION: i.v. injection of CFSE labeled HLSC Liver 24 h 7d 21 d Spleen Lung Pharmacokinetics BIODISTRIBUTION: intra-parenchymal injection of HLSC Liver Spleen Lung 6d 14 d HLA HLA+ 35 cells 30 25 20 HLA 15 10 5 0 1.000.000 500.000 6D 200.000 500.000 500.000 14 D 21 D BIODISTRIBUTION: Optical Imaging (OI) Pharmacokinetics Toxicology Aims: To find a safe first dose for dose escalation studies in man To identify potential target organs for toxicity To exclude the development of tumors Toxicology To find a safe first dose for dose escalation studies in man To identify potential target organs for toxicity model GalN/LPS specie SCID mice with FHF dose and route results 1x106 i.v. From the highest to lowest dose, one single injection resulted in animal death by pulmonary occlusion. 0.75x106 i.v. 0.5x106 i. v. 0.35x106 i.v. x 6 No signs of toxicity recorded after 48 hours, 7 and 21 days 10x106 intra-portal The surgical procedures is feasible. Liver necrosis in small regions and signs of thrombosis indicate that probably the amount of injected cells should be reduced and heparin should be added 5x106 intra-portal All rats appeared in good health conditions . Macroscopic observation of collected organs (liver spleen lung) did not show signs of necrosis or vascular thrombosis. Histological evaluation of liver, lung, spleen sections showed a normal morphology 5x106 i.par. All rats appeared in good heath conditions without signs of suffering. Macroscopic observation of collected organs (liver spleen lung) did not show signs of necrosis or vascular thrombosis. Histological evaluation of liver, lung, spleen sections showed a normal morphology. 0.5x106 i.par. x 2 Steatosis was observed in all samples, probably due to anaesthetics and to the operation procedure. AST and ALT levels in the blood showed similar liver functions in all mice 14 days after the second injection. Rats Healthy animals SCID mice 0.25x106 i.par. x 2 Toxicology To exclude the development of tumors n° of nude mice cells n° of cells injected Duration of monitoring 10 HLSC 1x107 sub-cut 16 weeks 10 HeLa (POSITIVE CTR) 1x107 sub-cut 16 weeks 5 DPBS (NEGATIVE CTR) 0.2 ml 16 weeks Validity The test resulted VALID The test is valid if: • at least 90% of the positive control group develops growing tumors • none of the negative control group develops growing tumors HLSC did not cause tumour formation Toxicology Karyotype and Tumorigenicity Skin Genetically stable: 2 months 14th passage Growth in agar Liver No tumour formation 6 months after s.c. inoculum in SCID mice Banking in Areta International (GMP) 1. Feasibility studies: HLSC from 3 different adult liver biopsies • • • Isolation Expansion Characterization: FACS analysis (CD73, CD29, CD105, and Albumin), and Potency test in RCCS (rotary cell culture system ) for 4 days 2. Production: • • • isolation, expansion and characterization of HLSC for creation of a master cell bank (MCB) MCB production (isolation and expansion) MCB characterization (FACS analysis and Potency test) MCB release (Sterility test, tumor in vivo formation and karyotype analysis) 3. Validation: • • • First validation run Second validation run Third validation run Validation run: defrost a HLSC vial containing 50x106 HLSCs for freezing in bags Where are we now in Turin ? Orphan Drug designation granted by EMA to HLSC in OTC and CPS (urea cycle disorders) and in Acute Liver Failure First Clinical Protocol Final Authorization for 3 patients HLSC in patients suffering from inborn liver metabolic diseases causing lifethreatening neonatal onset of hyperammonemic encephalopathy Study code: HLSC 01-11; EudraCT: 2012-002120-33 Principal Investigator: Dr. Marco Spada Co-Investigators: Dr. Renato Romagnoli – Dr. Dorico Righi ISS and AIFA (Rome) : June 2013 COMITATO ETICO (Turin) : December 2013 ACTIVE ENROLMENT FEASIBLE: February 2014 Piemonte – Valle d’Aosta : 4.500.000 abitanti - 40.000 neonati/anno TORINO Clinica Pediatrica, Università di Torino – Ospedale Infantile Regina Margherita Azienda Ospedaliera Città della Salute e della Scienza di Torino Unità Operative: - Malattie Metaboliche Ereditarie - Epatologia Pediatrica - Nefrologia pediatrica dialisi CVVHD nel neonato - Terapia Intensiva Pediatrica - Laboratorio Terapie Cellulari in Ematologia Pediatrica - Centro Trapianti di Fegato pediatrico e dell’adulto - Radiologia Interventistica «epatica» - Immunologia dei Trapianti - Laboratorio Biochimica Metabolica (esami 2° livello) TRAPIANTO DI CELLULE STAMINALI EPATICHE Origine delle cellule Frammenti di tessuto epatico prelevati dall’equipe chirurgica da fegati che vengono utilizzati per trapianto Nessun danno anatomico e funzionale all’organo trapiantato (macrobiopsie) Donatori d’organo classificati a “rischio standard”, ovvero casi in cui dal processo di valutazione non emergano fattori di rischio per malattie trasmissibili TRAPIANTO DI CELLULE STAMINALI EPATICHE NELLE MALATTIE METABOLICHE EREDITARIE Vantaggi clinici attesi Possibilità di produzione GMP e banking di cellule perenne disponibilità di cellule ABO-compatibili rapidamente trapiantabili Utilizzo di organi “standard” rispetto al trapianto di epatociti Terapia immunosoppressiva non prevista dal protocollo (attività immunomodulante delle HLSC come le MSC) Stabilizzazione metabolica e clinica dei pazienti, con possibilità di dilazionare o addirittura evitare il trapianto d’organo Where are we now in Turin ? Orphan Drug designation granted by EMA to HLSC in OTC and CPS (urea cycle disorders) and in Acute Liver Failure First Clinical Protocol Final Authorization HLSC in patients suffering from inborn liver metabolic diseases causing lifethreatening neonatal onset of hyperammonemic encephalopathy Study code: HLSC 01-11; EudraCT: 2012-002120-33 ISS and AIFA (Rome) : June 2013 COMITATO ETICO (Turin) : December 2013 ACTIVE ENROLMENT FEASIBLE: February 2014 Second Clinical Protocol in preparation HLSC in patients with acute liver failure arising in a previously healthy liver Final remarks The ‘stem cell bench’ is stepping into the clinic, especially in diseases without architectural distortion of the liver Nearly every field of hepatology will be touched in the mid-term, but solid organ transplantation as destination therapy for cirrhosis will still hold its place for a while Multidisciplinarity in translational research is a valuable and essential model for progress Funding remains a major issue. In this context, creation of European multinational Consortia should be encouraged Grazie per l’attenzione !