osmoregulation
advertisement

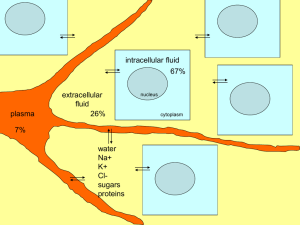
intracellular fluid 67% plasma extracellular fluid 26% 7% water Na+ K+ Clsugars proteins nucleus cytoplasm Definitions • • • • • • • Solute Solvent Osmosis Osmotic Pressure Osmolarity Hyperosmotic Hypoosmotic Solutes are dissolved particles in solution (any type) • Osmotic pressure depends on the number of solutes/unit volume (rather than chemical nature of solutes) Osmotic flux of water: --which way will the water move? -- Why is there net water flux tothe right? As this column rises higher, it will exert increasing pressure. At some point that hydrostatic pressure will reach an equilibrium, at which point no more net water will move across the semi-permeable membrane. This pressure is the ‘osmotic pressure’ of the starting solution on the right. Solutes are dissolved particles in solution (any type) isosmotic (osmotic pressure is equal) Solutes are dissolved particles in solution (any type) hypersmotic (higher osmotic pressure) hyposmotic (lower osmotic pressure) Water always moves from an area of low osmotic pressure to an area of high osmotic pressure osmotic pressure: the pressure of water to enter, given the solute concentration Hyposmotic (lower osmotic pressure) Hyperosmotic (higher osmotic pressure) Osmosis: movement of water from an Area with lower osmotic pressure to Higher osmotic pressure Osmotic pressures are generally described in osmolar units: Osmolarity = concentration of solutes in a solution Osmolarity vs. Molarity: 150 mMol sucrose = 150 mOsm sucrose 150 mMol NaCl = 300 mOsm NaCl Definitions • • • • • • • Solute: Dissolved particles in a solution Solvent: What the particles are dissolved in movement of water from an area with lower Osmosis: osmotic pressure to higher osmotic pressure Osmotic Pressure: the pressure of water to enter, given the solute concentration Osmolarity: Concentration of solutes in a solution Hyperosmotic: Higher osmotic pressure Hypoosmotic: Lower osmotic pressure The Mammalian Kidney Active movement of Na+ Passive movement of water Distal tubule Proximal tubule LOW Collecting duct Bowman’s capsule Na+ glomerulus H2O To bladder Extracellular Na+ conc. Loop of Henle HIGH What it actually looks like Distal tubule Proximal tubule Bowman’s capsule glomerulus Collecting duct Loop of Henle Hypovolemia Osmotic Imbalance Causing an increase in secretion and release of VP Baroreceptors in arteries of the heart VP 2 major effects: 1. Vasoconstriction 2. Water retention in kidney Passive movement of water Proximal tubule Distal tubule Collecting duct Bowman’s capsule glomerulus H2 O To bladder Loop of Henle The water pore is a protein called: aquaporin 2 (AQP2) Collecting Duct Cell n Collecting Duct: n filtrate Extracellular space Lower Na+ Basal side of cell apical side of cell Higher Na+ to bladder Collecting Duct: n n H2O Lower Na+ basal aquaporins H2O Aquaporin 2 No Vasopressin: Add Vasopressin: H2O Higher Na+ to bladder Collecting Duct: n n H2O Lower Na+ basal aquaporins H2O Aquaporin 2 Add Vasopressin: H2O Higher Na+ to bladder Collecting Duct Cross-Section Cells labeled with fluorescent antibodies made to the water channel n Collecting Duct: n Collecting Duct: Collecting Duct: Stain for aquaporin 2 (no vasopressin): Collecting Duct: Stain for aquaporin 2 (no vasopressin): Add Vasopressin: Collecting Duct: Stain for aquaporin 2: Add Vasopressin: Collecting Duct: 2 major effects of vasopressin: 1. Vasoconstriction 2. Water retention in kidney: V1a receptor V2 receptor Smooth muscle cell In arteries/capillaries Collecting Duct Cell VP DAG PLC Gq IP3 V1a receptor: localized to vascular smooth muscle cells V2 receptor: localized to the kidney Hypovolemia Control of Aldosterone Secretion IN THE BLOOD Renin ANGIOTENSINOGEN Made in the liver Secreted in response to low blood pressure ANGIOTENSIN I angiotensin converting enzyme (ACE: secreted by the lungs) ANGIOTENSIN II Adrenal gland (cortex) aldosterone Cells in the capillary walls ALDOSTERONE: Increases uptake of sodium from filtrate -Increases sodium in the blood -Decreases sodium in urine Active movement of Na+ Distal tubule Proximal tubule Collecting duct Bowman’s capsule Na+ glomerulus Extracellu lar Na+ conc. To bladder Loop of Henle Aldosterone and Angiotensin II production IN THE BLOOD Made in the liver ANGIOTENSINOGEN Renin from glomerulus ANGIOTENSIN I angiotensin converting enzyme (ACE: secreted by the lungs) Stimulate drinking ANGIOTENSIN II Cause vasoconstriction Induce release of VP aldosterone Increases Na+ absorbtion in the kidney REVIEW: hypovolemia A Decrease in Blood Pressure: • Heart baroreceptors cause posterior pituitary to secrete VP – VP increases vasoconstriction – VP increases water pores in the collecting duct, increasing water absorbtion from filtrate • Cells in glomerulus secrete renin – angiotensin II • • • • Increases aldosterone Increases vasoconstriction Increases VP Stimulates drinking – aldosterone • Increase sodium retention What about an increase in blood pressure? • Baroreceptors in heart stop sending releasing signals to SON and PVN • Glomerulosa cells produce less renin • Under conditions of excessively high blood pressure: – The atria of the heart secrete Atrial Natriuretic Peptide (ANP) – ANP: • Shuts down secretion of VP, renin, and ALDO • Increases sodium excretion in the urine • Increases diuresis (water loss in urine) Osmotic Imbalance Osmoreceptors: -Present in cells in the hypothalamus -when dehydrated, cause secretion of VP from PVN and SON Neural cells in hypothalamus containing osmoreceptors VP 2 major effects: 1. Vasoconstriction 2. Water retention in kidney Vasopressin and Osmolality Angiotensin and Aldosterone? These cells are also sensitive to osmolality -under low osmolality they secrete renin -under high osmolality the shut down renin secretion Cells in the capillary walls Under conditions of high osmolality IN THE BLOOD Made in the liver ANGIOTENSINOGEN LESS Renin from glomerulus LESS ANGIOTENSIN I angiotensin converting enzyme (ACE: secreted by the lungs) less drinking LESS ANGIOTENSIN II less vasoconstriction less VP LESS aldosterone Decreases Na+ absorbtion in the kidney Osmotic Imbalance Review High blood osmolality causes: • Osmoreceptors in the brain to signal SON and PVN nuclei to increase VP secretion – VP increases water retention in the kidney • Glomerular cells decrease secretion of Renin – Decrease Aldosterone secretion – Decrease Angiotensin II levels Pathophysiology of Osmoregulatory processes • Adipsic hypernatremia – Dipsia is thirst, hypernatremia is high salt load – These patients do not have osmoreceptors in the brain, so they don’t respond to hyperosmolality of the blood No osmoreceptors in the brain –No osmoreceptors, no VP secretion in response to cellular dehydration –They need water, but they aren’t thirsty –They do, however, have functional baroreceptors, and respond normally to changes in blood pressure Pathophysiology of Osmoregulatory processes • Adipsic hypernatremia – Dipsia is thirst, hypernatremia is high salt load – These patients do not have osmoreceptors in the brain, so they don’t respond to hyperosmolality of the blood – No osmoreceptors, no VP secretion in response to cellular dehydration – They need water, but they aren’t thirsty • Diabetes Insipidus – Two types: • Neurogenic DI: • Nephrogenic DI: Neurogenic Diabetes Insipidus VP is made but not transported VP 1. no VP is secreted 2. Very little water is retained in the collecting duct Treatment with VP can alleviate the problem Nephrogenic Diabetes Insipidus Collecting Duct Cell Vasopressin is synthesized and secreted normally VP But there is a defect in the cellular mechanism that responds to VP Pathophysiology of Osmoregulatory processes • Adipsic hypernatremia – Dipsia is thirst, hypernatremia is high salt load – These patients do not have osmoreceptors in the brain, so they don’t respond to hyperosmolality of the blood – No osmoreceptors, no VP secretion in response to cellular dehydration – They need water, but they aren’t thirsty • Diabetes Insipidus – Two types: • Neurogenic DI: Problem with VP secretion • Nephrogenic DI: Problem with VP receptors in collecting duct • Malignant hypertension Pathophysiology of Osmoregulatory processes • Adipsic hypernatremia – Dipsia is thirst, hypernatremia is high salt load – These patients do not have osmoreceptors in the brain, so they don’t respond to hyperosmolality of the blood – No osmoreceptors, no VP secretion in response to cellular dehydration – They need water, but they aren’t thirsty • Diabetes Insipidus – Two types: • Neurogenic DI: Problem with VP secretion • Nephrogenic DI: Problem with VP receptors in collecting duct • Malignant hypertension – Causes a sudden and severe rise in blood pressure – Can lead to blindness, seizure, chest pain, heart failure Hypothalamus Posterior Pituitary A B C