Hand-over Process - Zacharek
advertisement

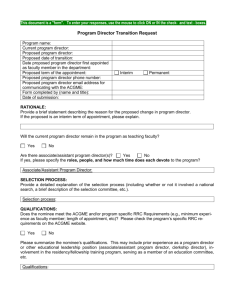
The Otorhinolaryngology Hand-Off: Pursuing Excellence in Patient Care and Safety Mark A. Zacharek, MD, FACS, FAAOA Associate Professor Associate Residency Program Director Department of Otorhinolaryngology Michigan Sinus Center University of Michigan Health System ACGME Common Program Requirements “Sponsoring institutions must ensure and monitor effective, structured hand-over processes to facilitate both continuity of care and patient safety. Programs must ensure that residents are competent in communicating with team members in the hand-over process.” ACGME 2011 CPR www.acgme.org Halstead on Surgical Residency “It will be objected that this is too long an apprenticeship, that the young surgeon will be stale, his enthusiasm gone before he has completed his arduous term of service. These positions are not for those who soon weary of the study of their profession, and it is a fact that the zeal and industry of these young assistants seem to increase as they advance in years and as their knowledge and responsibilities become greater.” The Otorhinolaryngology Hand-off ACGME standards promote teamwork. “Residents must work effectively as a member or leader of a health care team or other professional group.” “Residents are expected to work in interprofessional teams to enhance patient safety and improve patient care quality.” “Residents should have representation on hospital quality improvement committees.” ACGME 2011 CPR www.acgme.org Residents have Duty Hour Restrictions With a focus on restricted duty hours, the importance of communication between teams and individuals is of the utmost importance. Bo Schembechler (1983)“The Team, The Team, The Team!” The “handoff” (“handover” “signout” ) is part of the continuity of care when one resident is no longer in the hospital for a continuous period of time. Definition: Transitions of Care ACGME 2011 CPR www.acgme.org Programs must design clinical assignments to minimize the number of transitions in patient care. Responsibility for each patient may be transferred between 2 or more residents within a 24 hour period. “Sponsoring institutions and programs must ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety. Programs must ensure that residents are competent in communicating with team members in the handover process.” Can we standardize the otorhinolaryngology “handoff”? Handoffs may occur asynchronously without person to person/face to face interaction. Reduction in errors due to fatigue should not be offset by an increase in errors due to poor communication/improper information transfer. Multiple types of Handoffs Post-op Ambulatory Inpatient consult Outpatient/clinic Primary Oto inpatient service Primary Oto SICU patient in closed ICU system (General Surgery Staff and Resident) Different Otolaryngology Services (Neurotology, Head and Neck, VA, Pediatric) Multiple Hospitals (Home Call vs In House) Program Director Strategies: Supervision and provision of feedback Coaching (Senior resident and faculty observation of junior handoffs) Objective skills-based examinations Simulation of practice handoff skills Metrics in Portfolio for “Interpersonal Skills and Communication” Using a checklist? What do other professionals do? Causes of Error in Teaching Hospitals Between 1979-2001, closed malpractice claims data 240 errors in teaching settings - errors in judgement 72% - problems with teamwork 70% - lack of technical competence 58% Singh H et al. Medical errors involving trainees: a study of Closed malpractice claims for 5 insurers. Arch Intern Med. 2007;167(19):2030-2036 Transitions of Care in the Training Environment: ACGME Standards Dr. Bradley Marple, MD Dr. Marple is Professor and Vice Chairman of the Department of OtorhinolaryngologyHead and Neck Surgery at the University of Texas Southwestern. Additionally, he is the Chair of the ACGME Otolaryngology Residency Review Committee. Patient Handoffs: A Cognitive Systems Engineering Perspective Emily Patterson, PhD Dr. Patterson is an assistant professor at Ohio State University in the Health Information Management and Systems Division of the School of Allied Medical Professionals in the College of Medicine. She is an expert in the field of cognitive systems engineering with interests in health informatics and macro-cognitive communication. Patient Hand-offs: A Medical Education Perspective Ingrid Philibert, PhD MBA Senior Vice President, Department of Field Activities at the ACGME. Dr. Philibert is responsible for the Council's 31 MD and PhD accreditation field representatives as well as the 2000 site visits conducted annually. She is one of the editors of the ACGME's recent monologue regarding Duty Hour Standards "The ACGME 2011 Duty Hour Standards: Enhancing Quality of Care, Supervision, and Resident Professional Development".