Lean Sigma Healthcare
A New Model for CAH and Small Hospital
Quality and Performance Transformation
© SigmaMed Solutions 2011
all rights reserved
SigmaMed, the People
Jamie Martin, President & CEO
Six Sigma Black Belt from GE
20 years in Healthcare IT, EMR, Surgical Sales
6 years Applying LSH to HIT Workflow in CAHs & Clinics
Instructor in CEU/CME rated courses
Commercial Pilot with over 1,000 hrs in Light Aircraft
Wray Paul, VP Professional Services
MSEE and BSChemE, PMP
Master BB, 35+ years of LSS PI
Rural Hospital Director
EMR/PACS implementation Consulting
Design, development of PACS/EMR (5+ years on the
“Dark Side”)
Contract Healthcare Black Belts, including Nurses, PCMH
and Quality Directors, and EMR Implementation Experts
© SigmaMed Solutions 2011
all rights reserved
SigmaMed, the Company
Focus on Small and Rural Healthcare Facilities
Generalized PI and QI in all departments
EMR Deployment and Meaningful Use Process Redesign
Lean PCMH and ACO - Lean Core Process Redesign
Contracted Lean Six Sigma Provider for:
Colorado Rural Health Center
CORHIO and CO-REC
Contracted work for Wyoming PCA
Teach CE and CME rated Courses on LSH for:
Colorado AHEC
CU College of Nursing HIT Leadership Program
HRSA
Hospital and Practice Management Groups
© SigmaMed Solutions 2011
all rights reserved
Key (Unconventional) Ideas
Lean Sigma Healthcare is not an additional project
Rather, it’s a way to optimally complete projects you are doing
anyway, while simultaneously building internal capacity
You don’t need to master all of Lean Six Sigma to
be successful… learn a few tools and get going
We teach a version called Lean Sigma Healthcare, which is a
subset of LSS specific to healthcare
LSH doesn’t require huge commitment of time or
money
The most effective transformations begin with results
LSH teaches proper project management
LSH done right can be revenue positive in a very short timeframe
Change Leadership and Project Management are as
important as LSH tools/technique…we teach all
© SigmaMed Solutions 2011
all rights reserved
Why Lean Sigma Healthcare in Rural HC?
By Most Estimates, 40-70% of healthcare spending
is Pure Waste!
External Demands for PCMH, MU, JC, and payor
models are making our care provision processes
much more complex
HIT Isn’t Mature Enough to Help with
Complexity…and in fact make it worse!
Resource Constraints in Rural Areas Limit our
Options….can’t just throw money or people at problems
If we don’t take a proactive approach to designing care
processes things will only get worse as HIT is layered
on…
Safety-Quality-Cost-Patient & Staff Satisfaction
© SigmaMed Solutions 2011
all rights reserved
The Lean Sigma Healthcare Equation
Start with a Healthcare Specific Subset of Lean Six
Sigma…
Lean (Toyota Production System) adapted for a
Complex service industry…eliminate waste, improve flow
Six Sigma (Motorola and GE) adapted for a Defectprone service industry…focus on perfecting process
Work on the Right Project(s), Scoped Properly
With the Right Team
add… Change Leadership
plus… Process-focused Project Management
= LSH…A Simpler Methodology for Healthcare
© SigmaMed Solutions 2011
all rights reserved
Errors Reduced on Outpatient Services
• Substantial Reduction of A/R
• Eliminated 1+ FTE in Billing Department
Yuma District Hospital and Clinics, 2012
© SigmaMed Solutions 2011
all rights reserved
Cheyenne Health and Wellness Center
•
•
•
•
Increased Patient Visits past point of Break Even in 3 months
Greatly Improved Staff and Patient Satisfaction
Developed Internal Capacity to Continue Leading LSH
Redesigned Care Delivery Processes to Meet PCMH Level 1 & 2
© SigmaMed Solutions 2011
all rights reserved
CAH and FQHC Results with LSH
Decreased insurance defects at clinic admission by 100x
(50% defects to 0.5% defects) - Rio Grande Hospital, Del Norte
Increased customer satisfaction on test results notification
from 60% to 80%+ (red to green trending up,)
Increased patient visits 47% yr/yr in 3 months and Intake
appts. 83% within 5 months at WY FQHC
Reduced rework required on outpatient procedure orders
from 20% to less than 0.6%
Reduced patient waiting time for ortho surgery from 14
weeks to 31 hours (first call to surgery)—Theda Care,
Wisconsin1
1 From
“Lean Hospitals” Mark Graban, 2008
© SigmaMed Solutions 2011
all rights reserved
So Why Doesn’t Everybody Use LSS?
Benefits
Cost
Satisfaction
Quality
Safety
Perceived Barriers
Investment cost
Too many other
“big changes”
Not enough staff
resources
What are some
others?
© SigmaMed Solutions 2011
all rights reserved
Models for LSS – the Big Bang…
Big Idea
Big Implementation
Hire consultants
Train everyone
Start lots of projects
Big bet…
Leadership has too many
projects to provide needed
attention
$$ makes everyone
impatient
Hard to show results fast
enough to justify $$
Fire consultants
Not Realistic for CAHs
© SigmaMed Solutions 2011
all rights reserved
Models for LSH – Organic Growth
Big Idea
Small Implementation
Start with one project
Train one team
Leadership support for that
one project
Grow your capabilities
Small Bet…
One Project = Low Risk
Something you have to do
anyway
$$ often under the radar
Grow excitement from
results
Plan LSH growth from there
© SigmaMed Solutions 2011
all rights reserved
Successful Change Begins with Results
Activity Focus -- many organizations cite the number of
trained LSS resources, the number of projects, etc. as
evidence of success of program
Results Focus -- the only really meaningful measure of PI
success is tangible results, bottom line impact
Without tangible financial benefits, organizations lose
patience and pull back before effort has gained steam
By starting small, visibly, and meaningfully word of
project success may permeate an organization and create
the internal pull necessary to spread throughout
Change is greeted with open arms when it is proven to
generate positive benefits and is not seen as another
“flavor of the month” change program
This generates “internal pull” vs. shoving an unwanted
program down an organization’s “throat”
This is from Schaffer & Thomson’s 1992 Classic, “Successful Change Programs
Begin with Results,” in the Jan-Feb Harvard Business Review
© SigmaMed Solutions 2011
all rights reserved
Keys to LSH Transformation Success
Successful LSS Implementations
Committed Leadership
Use of Top Talent
Supporting Infrastructure
Formal Project Selection Process
Formal Project Review Process
Dedicated Resources
Financial System Integration
Not So Successful LSS Implementation
Supportive Leadership
Use of Whoever was Available
No Supporting Infrastructure
No formal project selection, review process, not integratged
© SigmaMed Solutions 2011
all rights reserved
SMS Virtual LSH Project Model
1. Train and Mentor Execs in Requirements for Leading a
Successful LSH Transformation
2. Assist in Picking the Right Project, the Right Team, Scoping
Correctly, and Keeping on Track
First project can be key to a successful LSH launch
3. Just-in-Time LSH training for Teams – “Learn & Use”
immediately increases retention
4. Intensive 1-on-1 Mentoring of Team Leaders in LSH
methodology and Project Leadership
5. Virtual Project Facilitation by SMS BB’s to advise teams
and make mid-course corrections
6. Always-available, “Asynchronous” Online LSH Training for
Teams and YB Certification Program for Team Leaders
7. Ongoing mentoring in LSH roll-out to maintain momentum
and assist in overcoming obstacles (that always appear!)
© SigmaMed Solutions 2011
all rights reserved
LSH Thoughtware
It’s the Process that’s broken not the People…
design perfect processes and people perform perfectly
(almost!)
The only people that can fix a process are those
that work in it every day (not managers)
Data is your ally….opinions are (nearly) always wrong
(otherwise the problem would have been fixed!)
You Must Plan Change in as much detail as you plan
for new implementation
Follow the DMAIC framework for all improvement
projects, great and small, to stay on track
Work can (and must) be done OTIFNE!
© SigmaMed Solutions 2011
all rights reserved
The Change Effectiveness Formula
E f (Q*A)
(E) Change Effectiveness
The Effectiveness of any change initiative is a
function of the Quality of the technical solution
“times” its Acceptance by the culture.
Courtesy of Destra Consulting, LLC
© SigmaMed Solutions 2011
all rights reserved
What do the Numbers Say?
With Effective OCM, Change Investment ROI =143%
That’s a gain of 43% with Effective OCM
Characteristics of Successful OCM
Senior and Middle Managers and Frontline Employees all were
involved
Reasons for the project were understood and accepted
throughout the organization
Everyone’s Responsibilities were clear
With Poor OCM, Change Investment ROI = 65%
That’s a loss of 35% without OCM
Reasons for the Failures
Lack of commitment and follow through by senior executives
Defective project management skills among middle managers;
Lack of training and confusion among frontline employees
(Source: McKinsey & Co)
© SigmaMed Solutions 2011
all rights reserved
Kotter’s Change Model
Kotter found that 2/3 of all Transformation efforts fail.
However, Successful Change Follows a Pattern
• Create Shared Sense of Urgency
• Remove Obstacles to the New Vision
• Systematically Plan and Create Short-term Wins
• Develop a Powerful Guiding Coalition
• Create a Vision
• Over-Communicate The Vision by a Factor of Ten – Yes 10X!
• Don’t Declare Victory Too Soon!
• Anchor the Changes in Organizational Culture
When these 8 factors are addressed, change efforts are highly
likely to succeed!
© SigmaMed Solutions 2011
all rights reserved
19
Human Elements of Change
Groundbreaking Thinking in “Switch…”,
2010, by Dan and Chip Heath
When you ask people to change you are Tinkering
with Behaviors that have Become Automatic
“Self control is Needed to Override Behaviors that
have Become Habits
However, People’s Self-control is Finite and they
can Only Handle so much Change
People Aren’t Closed to Change, Just Exhausted by
the Effort Required for Head to Over-ride Habits!
From “Switch…”, 2010, by Dan and Chip Heath
© SigmaMed Solutions 2011
all rights reserved
“How to Make A ‘Switch’
Direct the Rider – Rational
Follow the Bright Spots – clone what’s working
Script the Critical Moves – specific behaviors
Point to the Destination – vision, big picture
Motivate the Elephant – Emotional
Find the Feeling – make people feel something
Shrink the Change – make it manageable
Grow Your People – cultivate sense of identity
Shape the Path – Process
Tweak the Environment – change situation
Build Habits – habits are “free”
Rally the Herd – behavior is contagious, help it
spread
From “Switch…”, 2010, by Dan and Chip Heath
© SigmaMed Solutions 2011
all rights reserved
Essential Ideas for Change
Developing a Change Plan is just as Important as Using
Tools/Methodologies like Lean Six Sigma
An Early Win on a Visible Project is Necessary to Build the
Hope and Belief Necessary for Change
Leading Change is About Engineering Hope and Working with
Teams to Build a Path
Your Change Plan must Appeal to Peoples’ Heads (logic)
and Hearts (emotions) for Change to Last
People are Generally Not Unwilling to Change, Rather,
They are Exhausted by the Extra Effort!
© SigmaMed Solutions 2011
all rights reserved
Value and the Voice of the Customer
You are in Business to Deliver Value – good care – for
Patients
Steps in Your Process not Delivering Value Create Waste
Your Survival Depends upon Making Customers
(Patients) Happy every chance you get
View Your Processes from the Patient’s Perspective
We mistake our view of the process for the customer’s
The customer doesn’t care about our process
GE Concept of “Wing-on-Wing”
Projects need to have a clear connection to customer
needs expressed by the customer
These are called CTQ’s – Critical to Quality – or CTs
An good project improves top Customer CTQ’s (as determined by
a VOC, ie patient surveys, focus groups)
© SigmaMed Solutions 2011
all rights reserved
Needed - A Process View
People do a “bad job” because they are
working in a “bad Process”
What is wrong with HC Processes?
They were generally never “designed”, they just
happened. When they didn’t work, they got “patched”
There is usually not a standard process—people just
modify (on a whim)
Few indicators of Process performance get measured
We use measures broad outcomes (infections)
Usually don’t measure leading indicators (adherence to
sterile process for central lines)
© SigmaMed Solutions 2011
all rights reserved
What is the Result of “Bad” Process?
Wasted Time…
In end to end processes (Clinic door to door, ED door
to door, surgery appointment to discharge) 75% or
more of the time is wasted.
Time = money and patient satisfaction
Defects…
Healthcare Business processes often run at 50%
defect levels
Defects (like insurance information) often have to be
fixed. 25% plus of the billing department are often
working on fixing Admissions Defects
Defects = money, patient safety & satisfaction
Net result is 40-70% of what we do is pure
waste!
© SigmaMed Solutions 2011
all rights reserved
The Universal Complaint (UC)
“If [Department X] would just do their job,
then we [Department Y] could do our job
better, easier, faster, cheaper…”
Sometimes (rarely) it is the people, but far
more often it is the Process that is Broken
• 1% of the people in an organization should probably
be in another line of work…
• But that means that the other 99% can be very
effective—If we get the Process(es) right.
© SigmaMed Solutions 2011
all rights reserved
Decoding the Universal Complaint (UC)
Processes usually go wrong at the interfaces and
handoffs. Therefore the UC is caused by:
The Process actually is designed well, but Depts X
and Y don’t have a single view of how the process
works so they don’t interface correctly (Rarely).
OR (more likely) The process never worked right &
even if X and Y “did their jobs”, they would still be
frustrated and Defects and Waste would rule the day.
Therefore if you put good people into a bad
process, they will perform badly.
Bottom Line: If you are have a problem, put 99% of
your effort on changing the process, 1% on changing
the people.
© SigmaMed Solutions 2011
all rights reserved
How Can LSH Help?
It provides tools and methods to:
See where Waste is happening
Find the Root Cause of Defects
Redesign the Process to dramatically reduce
both
It engages the staff to:
Apply their intelligence and “profound
knowledge” of the Process to fix global problems
If they help design it, they have ownership of
the Process
It gives the organization principles to make
effective change and lead LSH expansion
© SigmaMed Solutions 2011
all rights reserved
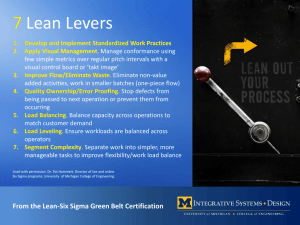
The LSH Equation
Give people the Tools to Lead Change and Lead
Projects
Work on the 20% that cause 80% of your Problems!
Redesign High Defect or Time Inefficient Processes
Get processes to 99.5% “good service” and high
Time efficiency
Data and statistics get easier
Minimize the number of LSS tools and learn to use the
“vital few”
Simple Process and Value Stream mapping
Six Sigma DMAIC project management methods
Fishbone and the 5 Whys for getting at Root Cause
Fail Early and Cheaply…
© SigmaMed Solutions 2011
all rights reserved
“OTIFNE” Work
Work is defect free ONLY if it is:
On Time – the next process step doesn’t have to
wait for it
In Full – completely finished so nobody
downstream in the process has to “fill in the blanks”
No Errors – there are no defects that somebody
downstream has to fix or the customer will see.
Simple Process Redesign Can Get You There
© SigmaMed Solutions 2011
all rights reserved
LSH Defect Goals
Manufacturing aims for 6 Sigma performance,
or 3.4 defects per million opportunities…
But, Healthcare isn’t Manufacturing. They are
way ahead of us!
Healthcare should start with a goal of ~4.5
Sigma, or 5 defects per 1000 opportunities
If we do something 1000 times, we should expect
no more than 5 OTIFNE errors (more on this later)
Don’t design new processes that can’t meet that goal.
Design Safety Critical processes so they are
“failsafe”
Design all others to meet this “Lean” Goal
Lean Sigma Healthcare will get you There
© SigmaMed Solutions 2011
all rights reserved
Defects are Just Symptoms…
BUT…You Can’t fix Symptoms
You Can Only Fix Root Causes!
Example “Shortness of Breath”
Is only a symptom. To fix it, the ED Doc has to find the
Root Cause
Root Causes of “SOB” (a few of 100 or so)
Altitude induced pulmonary edema
Pneumonia
Heart disease
COPD
All of those Root Causes require different
treatment!
© SigmaMed Solutions 2011
all rights reserved
Tools 1 -- DMAIC
Define – what do we want to do?
Measure – how can we see what we do now
and set an improvement goal
Analyze – see what our data tells us and
find the Root Cause of our issues
Improve – design an new process, try a
pilot of the new process, debug, improve,
train & scale
Control – select a few key metrics that tell
us whether we have actually improved
things. Use them to control the process in
operation.
© SigmaMed Solutions 2011
all rights reserved
DMAIC Solves Four Big Problems
Answers 4 Key Questions Before we Start
Are we working on the Right Stuff (in the
Right Way)?
Do Management/Leadership &
Stakeholders approve of what we are doing?
Who should be on the Team?
When will we be done?
It answers the fear-inducing question:
What do we do next?
© SigmaMed Solutions 2011
all rights reserved
Tools (2 of 4)—Process Mapping
We see too much
of this…
Problems
Hard to see who
does what
Very hard to see
Waste
Problems at
handoffs not
obvious
Can’t figure out
what to do next.
© SigmaMed Solutions 2011
all rights reserved
Better Process Mapping - Swimlanes
Much better to do
this…
Advantages
Easy to see who
does what
Easy to see Waste
Defects/Inspection/
Rework
Overprocessing
Handoffs explicit
(messages)
Easy to figure out
what to do next.
© SigmaMed Solutions 2011
all rights reserved
Tools (3 of 4)—Fishbone
World’s best
brainstorming
tool
Advantages
Aims directly at
Root Cause(s)
Avoids
patching
symptoms
Pareto voting
narrows the
investigation of
potential Root
Causes
© SigmaMed Solutions 2011
all rights reserved
Fishboning turns Symptoms into
Root Cause(s) of Defects
If you’re fixing a Defect problem, at first you only have the
Symptom (the Defect).
“300/1000 [=30%] of our Radiology orders have Defects”
If you throw “solutions” at it, they will probably won’t fix the
problem and will add Complexity to your process and Create
Waste!
People who actually work on the process have a lot of
ideas about what might Cause the Defect.
Fishbone Diagrams are a structured brainstorming
technique to get their ideas out.
Once you get all of the ideas out, you can Pareto the ones
you want to work on.
In our work, we almost always find that the Team correctly
identifies the Root Cause with a Fishbone Diagram.
The beauty of Root Cause is it saves you from
working on the 80% of the “issues” that won’t solve
the problem
© SigmaMed Solutions 2011
all rights reserved
Deep Dive on Causes…The “5 Whys”
Why do we create Defects on the
“rooming form” (1)?
Because we feel rushed
Why do you feel rushed (2)?
Because we only have 5 minutes
Why do you only have 5 minutes (3)?
Because the Provider is Waiting and Impatient
Why is the provider waiting (4)?
Because there are a lot of patients in the exam
rooms
Why are there lots of patients in exam rooms (5)
Root Cause = Because we send them back
whether we are ready for them or not….
The real Root Cause of a problem is often at the bottom of the 5 Why chain.
Everything above that is a symptom, not a cause.
© SigmaMed Solutions 2011
all rights reserved
Tools (4 of 4)—Graphing
Visualize your
data 1
Advantages
People draw
conclusions from
graphs, fall asleep
looking at data
tables.
95% of the time,
don’t need much
statistical
analysis.
1) Needless to say, you have to make
Process measurements in the first place
© SigmaMed Solutions 2011
all rights reserved
Selecting the Right Project
Good Projects
Clear Objectives
Directly connected to customer needs
Project is Scoped Correctly
Able to Complete within 3-4 months
Fixing Problem is Relevant to the Business
Fixing the Problem is Part of Team Leader’s (GB’s)
job responsibility
Makes life much easier
Data is easily available
Benefits are easy to calculate
Have a high likelihood of Success
© SigmaMed Solutions 2011
all rights reserved
Good Projects have SMART Objectives
Specific
Is it obvious what we want to do (and what’s out of
scope (bounds))?
Measureable
Can we count defects and measure time, money,
and other important variables?
Aggressive (but Achievable)
Is it a little bit of a “stretch” but still possible?
Realistic
Can we do it with the people, skills, time, and money
we have available?
Timebound
Have we specified when we plan to get it done?
© SigmaMed Solutions 2011
all rights reserved
LSH Projects Ideas on New Initiatives
Build It Right the First Time
Processes that take less time, reduce cost, AND give
you the results you need
Coming Down the Pike…or already on you!
PCMH/ACO/VBP
ICD-10/JC
EMR MU, etc…
Tend to add cost, because we layer them on over
already-stressed Processes
© SigmaMed Solutions 2011
all rights reserved
The path forward…what we need to do
Life is Short…Eat Dessert First
Change our thinking
We can't solve problems by using the same
kind of thinking we used when we created
them.” Albert Einstein
Set new goals
5 defects/1000
50%+ Flow Time Efficiency
Use new Tools
Lean Sigma Healthcare to eliminate Defects and
Wastes of time and human potential
© SigmaMed Solutions 2011
all rights reserved
LSH Services through WY ORH
eMaster Black Belt Services (eMBB)
Project Oriented Team Training, Mentoring, Facilitation
Virtual eMBB – high value, effective projects
Combo Virtual and On-site – SMS resource leading on-site partly
Single and Dual Project MBB – for facilities
Facility PI/QI/Data Analytics Redesign
Green/Black Belt Project Mentoring
LSH Practitioner Certification Services
Mentored Green or Black Belt certification in LSH
Online Training
Yellow Belt Certification Course – 4o Hrs of detailed training for
team Leaders
Team Training Course – 4 hrs of basic training for team members
Multi-Platform Data Reporting and Analytics
Software sales, implementation, and PS
© SigmaMed Solutions 2011
all rights reserved