Health Equity
Ron Chapman, MD, MPH
Director and State Health Officer
California Department of Public Health
What causes health inequities?
“The social determinants of health are mostly
responsible for health inequities - the unfair and
avoidable differences in health status seen within
and between countries. The structural roots of
health inequities lie within education, taxation,
labor and housing markets, urban planning,
government regulation, health care systems, all
of which are powerful determinants of health,
and ones over which individuals have little or no
direct personal control but can only be altered
through social and economic policies and political
processes.”
WHO Commission on the Social Determinants of Health
“Social Determinants of Health”
Social-Physical-Economic-Services Determinants
Income & income inequality
Education
Race/ethnicity/gender & related discrimination
Built Environment
Stress
Social support
Early child experiences
Employment
Housing
Transportation
Food Environment
Social standing
What is the role of health care?
Public Health Agency of Canada: “there is
mounting evidence that the contribution of
medicine and health care is quite limited, and that
spending more on health care will not result in
significant further improvements in population
health. On the other hand, there are strong and
growing indications that other factors such as
living and working conditions are crucially
important for a healthy population.”
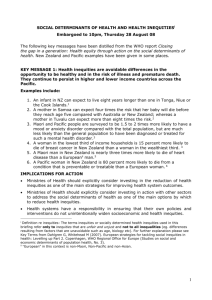
Estimated Deaths Attributable to Social
Factors in the US - 2000
Low education:
Racial segregation:
Low social support:
Individual level poverty:
Income inequality:
Area level poverty:
In comparison:
Acute MI:
Cerebrovascular disease:
Lung cancer:
245,000
176,000
162,000
133,000
119,000
39,000
192,898
167,661
155,521
Estimated Deaths Attributable to Social Factors in the US. Galea S et.al.
AJPH:June 16,2011;eprint.
Life Expectancy in the Bay Area
People who live in
West Oakland can
expect to live on
average 10 years less
than those who live in
the Berkeley Hills.
People who live in
Bayview/Hunters Point
can expect to live on
average 14 years less
than their counterparts
on Russian Hill
Residents of Bay
Point can expect to live
on average 11 years
less than people in
Orinda
Oakland, CA
Compared to a white child born in the Oakland
hills, a black child born in West Oakland is:
Likely to die almost 15 years earlier
5x more likely to be hospitalized with diabetes
2x as likely to die of heart disease
3x more likely to die of stroke
2x more likely to die of cancer
7x more likely to be born into poverty
4x less likely to read at grade level by grade 4
4 x as likely to live in a neighborhood with high
density of fast food and liquor outlets
5.6x more likely to drop out of school
Alameda County Department of Public Health
Inequities in Contra Costa County
Hospitalization rate for asthma for African American
children 5x that of White children
Latinas have a rate of births to teens more than twice that
of the county overall
Most of the homicide deaths in Contra Costa occurred
among African Americans
People living in San Pablo, Oakley, Richmond, Antioch,
Brentwood and Pittsburg, as well as African Americans and
men overall, are more likely to die from heart disease
Health Equity in California
Lowest Infant Mortality
Lowest Teenage Pregnancy
African Americans double
Hispanic teens double
Lowest Tobacco Use
Low income population double
How could income effect health?
Income directly shapes:
Parents’ income
shapes the next
Nutrition & physical activity
generation’s:
options
Education, which
Housing quality
shapes their
Neighborhood conditions
Working conditions
Social networks & support
(physical &
Stress due to inadequate
psychosocial) &
resources to face daily
Income
challenges
Medical care
Center on Social Disparities in
Health, UCSF
Children Raised in Poverty
Have lower levels of educational attainment
more likely to score lower on standardized tests, be held back
a grade, drop out of high school,
less likely to get a college degree
attend schools with fewer resources
suffer from poor nutrition, chronic stress, and other health
problems that interfere with their school work
change residences and schools frequently as their families
struggle to find affordable housing
Have lower earnings and are more likely to live
in poverty as adults
The Social Gradient in Health
* BARHII
Across racial and ethnic groups,
higher income*, more physically active adults
% of adults ages 25+ who are physically active*
45
40
35
<100% FPL
100%-199% FPL
200-299% FPL
300-399% FPL
≥400% FPL
30
25
20
15
10
5
0
Black, Non-Hispanic
* Similar by education
Hispanic
White, Non-Hispanic
NHIS 2001-2005 Age-adjusted
6.1 million Californians (16.3%) incomes <FPL
2.2 million Ca children (nearly ¼) in families <FPL
U.S.
• California
Health Impact of Resolving Racial
Disparities
1991 to 2000
Medical advances averted 176,633 deaths
Equalizing the mortality rates of Whites and
African Americans would have averted 886,202
deaths
“The prudence of investing billions in the
development of new drugs and technologies while
investing only a fraction of that amount in the
correction of disparities deserves reconsideration.
It is an imbalance that may claim more lives than
it saves.”
Wolff S. Satcher D., et.al. The Health Impact of Resolving Racial Disparities: An
Analysis of US Mortality Data. Am J Public Health. 2004;94:2078–2081
How could a neighborhood affect health?
Safe places to exercise
Access to healthy food
Exposure to targeted advertising of
harmful substances
Social networks & support
Norms, role models, peer pressure
Fear, anxiety, stress, despair
Violence and fear
Quality of schools
A PUBLIC HEALTH FRAMEWORK FOR REDUCING HEALTH INEQUITIES
BAY AREA REGIONAL HEALTH INEQUITIES INITIATIVE
UPSTREAM
SOCIAL
INEQUITIES
Class
Race/ethnicity
Immigration
status
Gender
Sexual
orientation
DOWNSTREAM
INSTITUTIONAL
POWER
Corporations &
businesses
Government
agencies
Schools
Laws &
regulations
Not-for-profit
organizations
LIVING CONDITIONS
Physical environment
Land use
Transportation
Housing
Residential segregation
Exposure to toxins
Social environment
Experience of class,
racism, gender,
immigration
Culture, incl. media
Violence
Economic & Work
Environment
Employment
Income
Retail businesses
Occupational hazards
Service environment
Health care
Education
Social services
RISK
BEHAVIORS
Risk Behaviors
Smoking
Poor nutrition
Low physical
activity
Violence
Alcohol & other
Drugs
Sexual behavior
DISEASE
& INJURY
Communicable
disease
Chronic
disease
Injury
(intentional &
&unintentional)
Individual health
education
Strategic
partnerships
Advocacy
Community capacity
building
Community organizing
Civic engagement
Health care
Case
management
POLICY
Emerging Public Health
Practice
Current Public Health
Practice
MORTALITY
Infant
mortality
Life
expectancy
Go Before You Show
Prenatal Campaign
First trimester prenatal care is key to
healthy birth outcomes.
In Solano County, 1st trimester prenatal
care was much higher for women on
commercial insurance vs. Medi-Cal.
Go Before You Show campaign created to
increase 1st trimester prenatal care in
Medi-Cal.
Results…
Office of Health Equity
Office of Multicultural Health
Office of Multicultural Services
Office of Women’s Health
Health in All Policies
Healthy Place Team