Blue Ribbon SI Powerpoint b19
advertisement

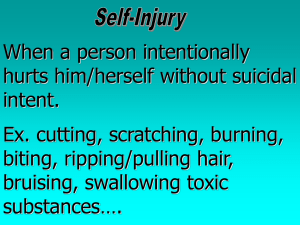
Understanding and Addressing SelfInjury in Schools Sara Burd Behavioral Health Coordinator Reading Public Schools sara.burd@reading.k12.ma.us Self- Care for Today Our topic is sensitive and at times participants may feel uncomfortable or experience difficulty processing information. Please take care of yourself and feel free to step out of the room, take a break, grab a drink, etc. as needed to care for your needs. Different Terms • • • • • • • • • Self-harm Self-injury Self-mutilation Repetitive Self-Mutilation Syndrome (RMS) Para Suicidal behavior Cutting Self-abuse Self-inflicted violence (SIV) Self-injurious behavior Definition Self-injury is a volitional act to harm one’s body without intention to die as a result of the behavior. (Favazza, 1996, 1987; Simeon & Favazza, 2001) The deliberate, impulsive mutilation of the body, or body part, not with the intent to commit suicide, but as a way of managing emotions that seem too painful for words to express. While self-injury is generally not about suicide, the behavior comes at the cost of: • Bodily harm • Potential scarring • Social stigma Methods of Suicidal Behaviors • High lethality behaviors that frequently pose risk to life and may result in death include: • • • • Use of gun Suffocation ( hanging) Poisoning (overdose, carbon monoxide) Jumping from a height Caution! • While suicide and self-injury are separate and distinct behaviors, they can occur in the same individual. • Ongoing assessment should focus not only on self-injury but also on suicidal thoughts, plans and behaviors. Methods • • • • • • • • • • Cutting • Constricting the flow of air passages Scratching • Limiting the blood supply Burning to body parts Preventing the skin from • Cutting off body parts healing Bruising or breaking bones Head banging Biting Hair pulling Punching self or objects Hitting the body with objects Self-Harm Behaviors Direct • Suicide attempts • Major self-mutilation • Stereotypic self-injury • Moderate/superficial self-injury Indirect • • • • • • • • • Substance abuse Eating Disorders Physical risk-taking Situational risk-taking Sexual risk-taking Unauthorized discontinuance or misuse of psychotropic medications Incidence and Prevalence • • • • • • • • Varying statistics 1% of population (National Mental Health Website) 4% in a community sample of adolescents (Garrison, et al. 1993) 13.9% of adolescents in more recent school samples (Ross & Heath, 2002) Incidence and Prevalence • Age of onset is usually age 12-14 • More females than males, however, significantly present in both genders. • All races and socio-economic groups Myth Busting • • • • • Cutters are suicidal Self-decoration is self-injury All have been physically or sexually abused Self-injuring adolescents have borderline personality disorder These kids need to be hospitalized (see myth vs fact handout) Possible Motivators Self-injury is seen as a maladaptive coping mechanism • To reduce intense feelings such as anxiety, depression, anger, sadness, tension, contempt, guilt and shame • To relieve too little emotion or states of dissociation/numbness Why People Self-Injure To communicate something: • • • • • For acknowledgement (please acknowledge I am upset) To punish (look what you’ve done to me) To change behavior of others To produce withdrawal (now you’ll give me space) To coerce ( if you break up with me, I’ll hurt myself) To elicit a response from caregivers, family members or significant others: • Competition for scarce resources (squeaky wheel) • Anticipation of aversive consequences (If I hit you I get suspended, if I cut myself I don’t) Students Report They Harm to: • • • • • • • • relieve tension feel alive inside gain control numb themselves vent anger re-associate relieve emotional distress or overwhelming feelings • gain euphoria • stop bad thoughts • purge out bad feelings • • • • • • • • • hurt and/or control others feel the warm blood see “red” to release emotional pain because their friends all do it scars show battles won self punishment for ritualistic nature to replace emotional pain with physical pain • immediate release for anger Experiences that May Trigger SelfInjury • • • • • • • Recent loss Peer or family conflict Intimacy problems Body alienation or dissociation related to abuse Impulse control problems Drug or alcohol use Trauma Risk Factors • Having friends who self-injure and communicate about the behavior extensively • Being prone to intense emotional distress with limited abilities to manage it • Episodic anxiety, depression • Spending time on websites, message boards or chat rooms dedicated to self-injury • Being pre-occupied with music, stories, art, about self-injury • Performance problems or stresses in areas of school, work, athletics or extracurricular activities Physical Signs • • • • Inappropriate clothing for the weather Blood stains on clothing Unexplained scars, bruises, or cuts Possession of sharp implements (razor blades, thumb tacks, knives, etc.) • Secretive behavior - spending unusual amounts of time in bathroom, other isolated areas Emotional Signs • • • • • • • Unable to cope with strong emotions Excessive anxiety and fears Excessive rage, depression Poor self-esteem or self-loathing Not connected with positive support system Increased isolation and withdrawal Art and writing displaying themes of pain, sadness, physical harm • Changes in social interactions or interests Can Be Ritualistic in Nature • Certain times • Certain rooms • Certain objects Co-morbid Disorders • • • • • • • Anxiety Depression Bi-Polar PTSD Eating Disorders Substance Abuse Borderline Personality Protective Factors • • • • • Healthy emotion regulation skills Ability to self-soothe A strong support network A positive body image Positive thoughts and beliefs Cognitive Behavioral Therapy Examples of distortions in thinking: 1. Self-injury is acceptable 2. One’s body and self is disgusting, and deserving of selfpunishment 3. Overt action is needed to tolerate unpleasant feelings and communicate feelings to others 4. Self-injury doesn’t hurt anyone 5. It’s the only way to know people care 6. It keeps people away 7. If I don’t have it, I will kill myself. It’s the only thing that works. 8. I can’t control it. Other Types of Therapy • • • • • • • Family therapy Addiction treatment Trauma/abuse treatment Medication Dialectical Behavioral Therapy Combination of above Group therapy not recommended usually Therapist Recommendations • Many therapists not well-trained in areas of self- inflicted violence • Much secrecy surrounding the behavior • Goals of therapy should be related to underlying cause of pain Examples of Positive Coping Strategies • • • • • • • • • Communication strategies Exercise programs Relaxation, stress management Mindful Breathing (Kabat-Zinn, 1990) Meditation, Visualization Art therapy Journaling TALK TO SOMEONE!!! Students should be in school during treatment - respond well to structure, normalcy, safety S.A.F.E (Self-Abuse Finally Ends) 1-800-DON’T CUT • • • • Inpatient and out patient services for serious self-injury When self-injury is interfering with ability to function Person must self refer Insurance is accepted Mobile Crisis Unit • Eliot Community Human Services • 24/7 Prompt team response to behavioral health crisis • 1-800-988-1111 • www.eliotchs.org • Donna Kausek, Program Director School Best Practices What School Mental Health Can Do • Provide awareness and knowledge • Educate students to report self and others • Educate school staff • Use a team approach, when necessary • Assess for safety, co-morbid disorders and suicide • Develop safety plan • Notify and collaborate with parents • Collaborate with community support • Control the contagion effect Awareness and Knowledge It is our professional & ethical obligation to: • Practice within the boundaries of our competence • Be able to identify students who self-injure • Differentiate self-injury from suicide attempts • Know that it is not “just attention getting” behavior • Understand the contagion effect • Know our community resources to make appropriate referrals • Understand our legal & ethical obligation to report Educate Students to Report • Report all dangerous behaviors to an adult who can help. • Do not use awareness campaigns about this topic or describe behaviors to students. SOS: Signs of Suicide ACT- Acknowledge Care Tell Educate School Staff • Educate them about the warning signs • Understand self-injury as coping attempt not suicide attempt • Train staff to identify and appropriately respond to these students • Staff should not just tell the student to “stop” • Report behavior to school mental health personnel Responding to the Student Do • Approach the student in a calm and caring way • Accept him/her even though you do not accept the behavior • Let the student know that you care about them and believe in their potential • Understand that self-injury may be their way of coping with emotional distress • Understand that self-injury is usually not about suicide • Refer the student to the counselor, social worker, nurse • Offer to go with the student to see the professional helper • Remember that the teachers role is not to solve the problem but to refer the student to a trained professional Responding to the Student Don’t • Say or do anything to cause the student to feel guilt or shame • Act shocked or appalled by their behavior • Talk about their self-injury in front of the class or around peers • Lecture them as to what you think they should do • Judge them or conclude they are doing it just for attention • Promise the student to keep the self-injury confidential under any circumstances • Use punishment or negative consequences if a student selfinjures • Make deals in an effort to get the student to stop self-injuring Assess for Co-morbidity and Suicide • Check for signs of other co-morbid disorders such as depression or drug use. • Assess for suicidal ideation • Be direct with questioning about topics involving danger to self or others Develop a Safety Plan • Short term plan serves to help stabilize student until community support can begin • Do not emphasize expectation that student is not to selfinjure; to stop behavior • Help students to identify the triggers for the behavior and possible physical cues • Help to understand the function of the behavior • Encourage student to talk to someone before cutting - give help line phone numbers • Remove objects, etc. when possible No Harm Contracts • What is a no-harm contract? • Not recommended as a strategy for working with these students in schools without other intervention Reporting Self-Injurious Behavior Three situations in which the school mental health provider is obligated to share confidential student/client information: 1. When student requests it. 2. Situation involving danger to the student or others (duty to protect). 3. When there is a legal obligation to testify in a court of law. Ethical Considerations NASW, NASP and APA • Do no harm • Provide services within competency and enlist assistance of others • Inform of limits to confidentiality • Promote parental participation in designing services provided to children • Referral for service Other Considerations for Limits to Confidentiality • Important differences from therapist-client relationship • Permission needed for psychological treatment in schools • School district policy Parent Notification • • • • • Notify and involve parents Ascertain whether parents already know of behavior What is already in place to support student? Gather additional history Document your parent contact Collaborate with Community Support • Get a release to communicate with student’s therapist • Understand the treatment goals and techniques in order to reinforce in the school environment • Our observations and feedback can often be helpful to therapists Controlling the Contagion Effect Assess factors that may be contributing: • Direct modeling influence • Disinhibition • Competition • Peer hierarchies • Desire for group cohesiveness • Pseudo-contagion episodes (Walsh, 2005) Controlling the Contagion Effect Strategies for managing and preventing contagion: • Identify the primary status peer models • Communicate with them that they are hurting their peers by communicating about self-injury • Encourage them to communicate with school supports, family, or therapist • Ask them not to appear in school with visible wounds or scars • In rare cases, students may have to be dealt with in a discipline manner (Walsh, 2005) Personal Reactions to SelfInjury • • • • Violent nature of self-injury can be unnerving. Watch for anger, disgust or sadness responses. Growth and change can be slow. Requires a large emotional investment. Watch for helplessness, guilt or betrayal responses. • Over-empathy or over-reaction. • Watch for “attention-seeking”response Practice Find a partner… You are a teacher of Karen’s. On Monday morning Karen pulls you aside with tears in her eyes and tells you she had a very bad night. Karen lifts her sleeves up and reveals bandages covering cuts that were made recently. Karen tells you that she is going to need some time to recover and asks that you be lenient and not call on her in class today. Karen turns to walk away. • You are a teacher of Ron’s. Ron is a leader in his classes and a great student. On Wednesday you notice that Ron hasn’t taken off his coat for hours despite the fact that the heat is pumping hard and everyone is sweltering. His coat is wide open and it appears he has short sleeve on underneath. You begin to observe more closely and notice that Ron is constantly pulling his sleeves down to cover his hands. • You are Jamie’s counselor. Jamie has just shared with you that she self-injures by burning large portions of her skin with her hair straightener. Jamie does not feel she is able to stop or slow her behavior right now and is particularly stressed and triggered by her recent breakup. Jamie does not want you to tell anyone. • You are Karen’s counselor. Remember Karen? Karen was referred to you by her classroom teacher and has shared with you the details of her self-injurious behavior. You are about to call her parents. Karen is worried her parents will overreact or punish her. Mindfulness • • • • Outside- In Leaves on a river Raisin reflection The Guest House Poem Yoga 4 Classrooms • • • • • • • • • • • Balloon Breath Ocean Breath Bumblebee Breath Power Breath Rock the Baby Monkey Arms Chair Pose Eagle Pose King Dancer Tree Half Sun Salute • • • • • • Warrior Loosen the knots Magic Massage Washing Machine Positive Opposites Change the Channel Resources SELF-INJURY:Awareness and Strategies for School Mental Health Providers Linda Kanan, PhD, Jennifer Finger, MSW, LCSW New Developments in Understadning and Treating Self-Injury Barent Walsh, Executive Director: The Bridge of Central Massachusetts, Inc SOS: Signs of Suicide Middle and High School Suicide Prevention Program Yoga 4 Classrooms: Tools for Learning, Lessons for Life. Lisa Flynn