Jönköping County Council and Health care services
advertisement

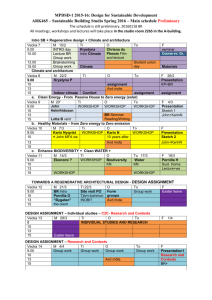
06/11/2012 "Designing and managing care integration in the County of Jönköping Welcome to Jönköping County Council and Health care services 24 October Pernilla Söderberg Qulturum Jönköping Sweden Sweden Norway Jönköping County UK Jönköping Jönköping district Germany Eksjö Eksjö Highland district To meet the future or to create the future Welcome to Qulturum Jönköping County Council France Italy Spain Värnamo Värnamo district Europe Jönköping County: Population: 330 000 13 cities/municipalities Mission Best possible care all the time How to create a culture where everyone is inspired to give the best possible care all the time. And also to create an evironment of curiosity for how to make today’s work even better tomorrow. The true journey of discovery is not to search for new sites, but to see the old, familiar one with new eyes. Marcel Proust 1871- 1922. French Novelist 1 06/11/2012 Put on different lenses Drive the train at 200 km/h . . . and lay the rails for the future And look closely at the microsystem. . . Every one looking at the same thing at the same time Very close Some examples of lenses Economic, political, anthropological, information, psychological, mechanical/physical, sociological and biological To think about…. • Equal care is NOT that all employees CAN do the same thing… • Equal care means that all employees both SEE and DO the same thing! • • • • If something works – do not break it Do more of what works If something does not work – do it differently If it is too slow – go slower 2012-11-06 Pernilla Söderberg 2 06/11/2012 Improvement in Our Heart WILL with the patient’s perspective -Attitudes -Driving force IDEAS -Conrete ideas about how something could be better. Inspiration from good examples -Methods and tools EXECUTION Science + context = result -Go from word into action Our GPS -Measure results and make it visible Ref; IHI Tom Nolan To develop a culture of improvement : From “theory” to “praxis”… and back again Better patient, population outcome Better professional development You have two jobs: to do your job and to improve it! Professional knowledge Improvement knowledge - Professional knowledge - Personal skills - Values, ethics - System - Variation - Psychology - Knowledge Everyone Our GPS Improving diagnosis, treatment, care, rehabilitation and follow-up Better system performance Our GPS Ref; Paul Batalden + Improvement in processes and systems in health care Increased Value for the Patients Paul Batalden Batalden et al. Simple Rules • Health care always emanates from the patient’s value, need and whishes • We protect the patients and ourselves • It is the system’s result that counts • We share the results from our development and improvement work with others • Either solve the problem or take responsibility for the handing over to next step Our GPS • Feedback to the step before • Work with guidelines Imagine yourself as a learner! In a time of drastic change, it is the learners who inherit the future. The learned find themselves equipped to live in a world that no longer exists Eric J. Hoffer Social Writer: 1902 –1983 3 06/11/2012 The P’s M5ik roof sythe stemicrosystem mets fem P LEAN Purpose Purpose /syfte Patienter Patients • What value shall we Vilket värde accomplish? • Who Vilkaare är they? de? ska vi åstadkomma? • How well do we know Hur their väl känner needs?vi deras behov? • How do we involve them more? Hur involverar vi dem mer? People/ People/colleagues medarbetare • How do w e use and take Hurcare nyttjar och of the tillvaratar ofviour competence medarbetarnas colleagues in the best wkompetens ay? på bästa • sätt? How do w e involve them Hurmore involverar in the vi improvement dem mer i w ork? • utvecklingsarbetet? How do w e increase our colleague’s Hur ökar vi understanding of our medarbetarnas mission? förståelse för sin uppgift? Processer/ Processes flöden • How do we Patterns/ Patterns mönster • How do we learn more about evaluate Hur the variations in the utvärderar vi clinical work? variationer i det kliniska arbetet? our Hur lär vi oss processes? mer om våra • How do we use processer? the result? • How Hur do använder we vi oss av improve our coresultatet? operation? Hur blir vi bättre på länkning/samv erkan? Att out, kartlägga, reflektera, och försöka systematiskt förbättra To map reflect, discuss samtala and try to systematically improve Ref: Godfrey, Nelson,Batalden Ref; Henriks, Nilsson, Bojestig, Edvinsson, Berger Every system is perfectly designed to achieve the results it gets Tools and Methods Donald Berwick Ref:Caroline Fruberg 4 06/11/2012 Activity is not always change Breast cancer process Surgeon Time in the old days 42 days. Punction och cytology 2-3 hours Mammography and ultrasound This IS change • Increase phonetimes • Change schedule based on needs • 5 S pharmacy stock • Feedback (measures) an compliance to standards • Reduce no of steps in a care process This is NOT Change • Planning • Having a meeting • Educate staff • Do a protocol • Point out a responsible person • Write on the intranet Surgeon Find the gap, analyze the problem, do tests To measure and analyze over time 2. 3. vecka Plan small tests (goal, measure and time) 5 P to understand your setting. antal dagar Väntetider sjukgymnastik 18 5 antal dagar do test Describe the process from the patient’s perspective. study results decide – new test? Fishbone Define the problem Ask why, why, why Brainstorm Sort and group Multi-vote • • • • • Act Plan Study Do 20 18 16 14 12 10 8 6 4 2 0 v 20 where are the largest gaps? How do we measure? v 20 v 35 TEST fr o m v 26 Havregrynsgrötsfrukost HYPOTES Ökad effektivitet på dagtid ger kortare väntetid v 35 1. vecka Most problems are found in processes not in people antal dagar Väntetider sjukgymnastik v 34 v 32 v 30 v 28 v 26 v 24 20 18 16 14 12 10 8 6 4 2 0 v 22 18 10 2 8 14 5 14 6 20 4 11 17 3 9 15 5 v 20 v 20 v 21 v 22 v 23 v 24 v 25 v 26 v 27 v 28 v 29 v 30 v 31 v 32 v 33 v 34 v 35 antal dagar vecka vecka TEST fr o m v 26 Havregrynsgrötsfrukost HYPOTES Ökad effektivitet på dagtid ger kortare väntetid 5 06/11/2012 Success is achieved through meeting the needs of those we serve You must be the change you want to see in the world Ghandi Defining Quality Background/Project application The study presented in the report "A national cancer strategy for the future" - SOU 2009:11 Their aim is to go from words into action. Regional Colon Cancer Project. In their improvement work, the region aims to focus on ’the patient’s pathway through health care’’ ”More patient-centered and more cohesive cancer treatment” The approach covers the entire health care chain; from colon cancer prevention to the palliative care, in order to create a whole from the different parts. RCC’s promises to the patients • All patients with cancer in the region should receive treatment within four weeks • All patients with cancer should be offered diagnosis and treatment of Best Practice • All patients with cancer should be informed and involved throughout the entire healthcare chain • All patients with cancer in palliative care should receive equally good palliative care services no matter where they live • All patients with cancer should be offered the best possible health promotion measures and efficient screening program • Regional Cancer Centre South East should prioritize patient-oriented research in oncology Symptoms of the individual Diagnosis Die of cancer Live with cancer Measures Treatment decisions Healthy Symptom Diagnostics=good basis for decision Healthy Involvement, making own decisions, feeling safe, being informed, symptomatic relief Getting worse Identifying current patient Relaps/Generalising Prevention within the population 6 06/11/2012 Method • • • Research Approach Three multi-disciplinary teams from each county council were formed in order to, together with the patients and relatives representatives, develop and improve the process of colon cancer treatment. The improvement work integrates an interactive learning approach for systematic monitoring i.a. through the existing data records in the open quality registries The learning part throughout the process begins with listening to the experiences of the patient and relatives and ends with examining the actual needs. The researchers contribute with the feedback analysis, the theory and methods for the improvement work. Both quantitative and qualitative data will be used The Value Compass will be the measuring instrument throughout the work. Impact Analysis for a good colon cancer treatment ©IHI Action plan An action plan has been developed with the following focus areas: • Overall/General • Development of measurements and performance indicators • Patient Involvement • Primary, secondary and tertiary prevention • Early detection • Investigation, treatment and rehabilitation • Multidisciplinary collaboration • Palliation Primary Impact ’’What’’ Secondary Impact ’’How’’? Will be given an adequate treatment within the four weeks’ time Investigation / Treatment Goal / Objective Will be offered the diagnosis and treatment of 'best practice' Will be well-informed and involved in the entire health care chain Our promises to the patients with a colon cancer In the end of their life will be given equally good palliative care regardless of place of residence Good Care Each area of the Action Plan has a number of objectives and actions identified. Will be offered the best possible health promotion measures and effective screening programs Regional cancer center will prioritize patient-oriented research in Oncology Promise 1 – Will be given an adequate treatment within the four weeks’ time Early detection Investigation phase Patient involvement Investigation / Treatment Patient involvement Patient and family experiences Multidisciplinary collaboration Palliation Prevention Interactive research approach in several aspects of the project Palliative phase Prevention Research Functional status / health status Patientupplevt funktionellt status vid första besök efter operation i samband med koloncancer resultat av enkätsvar Sydöstra sjukvårdsregionen 2011 - 2012 100% Quality of life 90% 80% Agitation / anxiety 70% 60% 50% appetite 40% Survival 30% Jag klarar av mina huvudsakliga aktiviteter (andel svar Ja, helt och hållet) 20% Aptit (andel svar 0-3, 0=bästa möjliga aptit, 10=ingen aptit) Oro/ångest (andel svar 0-3, 0=ingen oro/ångest, 10=värsta tänkbara oro/ångest) 10% Livskvalitet (andel svar 0-3, 0=bästa möjliga livskvalitet, 10=sämsta tänkbara livskvalitet) 0% Coverage ratio It is important that we identify the improvement areas locally and that we make sure that they are improvements and not just changes. jan-jun 2011 (n=15) jul-dec 2011 (n=21) jan-jun 2012 jul-dec 2012 main activities Clinical Status Patient/Customer’s needs Welcoming attitude Complications Good care Colon cancer Involvement Information Stage after diagnosed Resources / Costs competence hospitalization lead time investigation costs 7 06/11/2012 Patients’ experience Patients with colon cancer Results of the survey related to visits following diagnosis and starting treatment, the proportion of answers: yes, completely South East health district 2011-2012 Coverage/Ratio in a Colon Cancer Registry The percentage of planned colon cancer surgery reported in INCA within five months after surgery 2011-2014 Results of the survey related to the visits following diagnosis and surgery of colon cancer South East healthcare region 2011-2012 Percentage of post operative MDK-colon cancer(non-emergency surgery) From INCA-registry South East Health District 2012-2012 Ur rapport nr 3 från Kolorektalcancerregistret, perioden jan – apr, 2012 Percentage of post-operative MDK-colon cancer (elective and emergency surgery) From INCA-registry South East Health District From diagnosed cancer to the treatment (Diagnosis to the start of treatment) Medianen Östergötland Jönköping Kalmar 80:e perc. 22 22 22 Medianen 47 41 43 Östergötland Jönköping Kalmar 80:e perc. 25 16 18 50 31 38 8 06/11/2012 Reflections of a 59 year-old woman. From diagnosed cancer to the treatment (Diagnosis to the start of treatment) Antal dagar från diagnos till behandlingsstart Koloncancer (n=137 patienter), Östergötlands län, Diagnosår 2011 Colon cancer (n=patients), Ostergotland County Council, year of diagnosis 2012 • ’’It was a very long waiting time for the x-ray results; I 100 90 80 70 60 50 80:e percentilen=50 dagar 40 30 Median=25 dagar 20 10 0 Jan Feb Patient’s individual preferences Mars April Maj Juni Juli Aug Sept Okt Nov Dec Patient’s process Patient’s context First symptom Patientens Patientens sammanhang sammanhang Patient’s context Första Första symtom symtom First contact Första Första kontakt kontakt Patientens Patientens sammanhang sammanhang Patienters individuella preferenser Undersökning bedömning uppföljning Information Behandling/ åtgärd Kompetens Symtom Patient Patientcentrerad processkartläggning för ____________________________________ Patientens Patientens sammanhang sammanhang Patientcentrerad processkartläggning för ____________________________________ Första Första symtom symtom Patientens Patientens sammanhang sammanhang Första Första kontakt kontakt Patientens Patientens sammanhang sammanhang Patient Patientcentrerad processkartläggning för ____________________________________ Utredning Utredning Patientens Patientens sammanhang sammanhang Beslut Beslut om om åtgärd åtgärd Patientens Patientens sammanhang sammanhang Behandling/åtgärd Behandling/åtgärd Patientens Patientens sammanhang sammanhang Uppföljning Uppföljning Patientens fysiska, psykiska, sociala och existentiella behov Undersökning bedömning uppföljning Information had to wait 4-5 weeks • ’’I’ve met many different physicians • This can be very confusing • Maybe it would be more efficient if I could have registered a day before the surgery and just stayed at the hospital.’’ • Once I should have had my surgery in the morning but I didn’t leave the hospital until 5 pm. It’s quite tough to be without food for such a long time.’’ Patientens Patientens sammanhang sammanhang How to support these processes In our region we have 8 process leaders • Palliative care • Prostate cancer • Head and neck cancer • Brain tumor • Breast cancer • Gynecological cancer • Lung cancer • Malignant lymphoma Behandling/ åtgärd Kompetens vilka vilkaytterligare ytterligare kompetenser kompetenser behövs behövsiidetta detta steg? steg? Symtom Patient Patient Patient Patient Patient Patient Support • Coaches • Education – process leader program • Learning by doing Thank you! Pernilla Söderberg Qulturum Jönköping Sweden 9