Tantrums: Not Just the Terrible Twos
advertisement

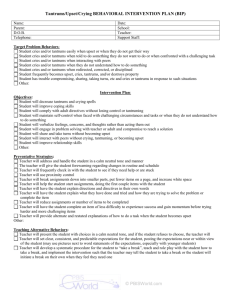
Tantrums: Not Just the Terrible Twos Rachel J. Valleley, Ph.D. Assistant Professor, Munroe-Meyer Institute Licensed Psychologist Behavioral Health Concerns in Primary Care Behavior problems ranked #1 by pediatricians (Arnorfer et al., 1999) Established link between medical and behavioral concerns (Wertleib et al., 1988) ADHD evaluations increased three-fold in 1990s (Hoagwood et al.,2000) In 24% of pediatric visits, behavior concern raised. Increases visit length from 11 to 17 minutes Tantrums What are tantrums? – – – – Screaming, crying, kicking Pleading Pointing fingers Pouting You are the meanest mommy in the world! Tantrums Duration can be seconds to minutes typically Most common for ages 2 to 4 but can occur at any age (80% of children) Tantrums Why do kids throw tantrums? – Frustrated with a task – To get what they want – Trying to develop independence skills, do things on their own Tangible Parental attention To get out of what they don’t want to do I want, I want, I want Pay Attention To Me I can’t hear you so I don’t have to do it! Tantrums Occur anytime, any place – – – At home Store Car How parents feel after tantrums When to be concerned about temper tantrums? Lasts for long periods of time Involves aggression Occurs frequently Causes distress to family Interferes with daily living Tantrums Can lead to or be a sign of more serious difficulties – – Oppositional Defiant Disorder ADHD Oppositional Defiant Disorder Enduring pattern of uncooperative, defiant, and hostile behavior toward authority figures that does not involve major antisocial violations. Frequently gets confused with ADHD. Can have both. Oppositional Defiant Disorder: DSM-IV Criteria Loses temper Argues with adults Actively defiant or refuses to comply with adults’ requests or rules Deliberately annoys people Blames others for his or her mistakes or misbehavior Touchy or easily annoyed by others Angry and resentful Spiteful or vindictive Oppositional Defiant Disorder Most common diagnosis given in our clinics in pediatric practices. Can be setting specific Occurring more with parents or other caregiver Difficulties with sleeping, eating, and toileting. Increased risk for other problems Dropping out, Abuse Coercive Family Process Oppositional Defiant Disorder Misconception that “He’ll grow out of it”. – 67% at age 3 still have problems at age 9 Often leads to Conduct Disorders or antisocial personality disorder. Effective early intervention leads to long-term positive outcomes No medication that will effectively work Oppositional Defiant Disorder Empirically-Supported Treatments: – Parent Training: Forehand & McMahon – Parent-Child Interaction Therapy: Hembree-Kigin & McNeil Treatment for ODD: Parent Training 1. Encourage/increase appropriate behavior Differential Attention Child’s Game Sticker Charts/Grab Bag Prizes Treatment for ODD: Parent Training Differential attention – – Attend to average behavior Praise exceptional behavior Treatment for ODD: Parent Training The Child’s Game: A relationship-building activity that makes children want to earn your POSITIVE attention. Treatment for ODD: Parent Training DO – – – – – Describe Reflect Imitate Praise Touch DON’T – – – Command Reprimand Question Goal is to like each other again Treatment for ODD: Parent Training Sticker Charts/Grab Bag Prizes: – – – – – Bedtime routine, morning routine Daily for overall behavior Magic circle chart Dot-to-dot’s Grab Bag Prizes Treatment for ODD: Parent Training 2. Decrease inappropriate behavior Time out Treatment for ODD: Parent Training What is time out? – Time out is the removal of attention, tangibles, or anything interesting to the child for a brief amount of time. Treatment for ODD: Parent Training Common mistakes parents make – – – – Talking to child in time out Having time out be too long Not having child do what is expected following the time out Not expecting extinction burst Treatment for ODD: Parent Training Common uses for time-out – – – – Noncompliance Aggression Rule infractions Tantrums Summary Tantrums can be very distressing to parents Good idea to assess for tantrums, noncompliance – – – – – How often? How long? What causes tantrums? How does the parent respond? Is this behavior distressing to the parent? If problem exists, good idea to refer to behavior therapist Early intervention results in best outcomes