Overview of Adolescent Substance Abuse & Treatment
advertisement
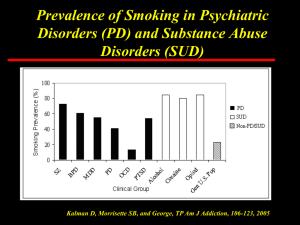
Overview of Adolescent Substance Abuse & Treatment Joan E. Zweben, Ph.D. Executive Director, EBCRP Clinical Professor of Psychiatry, UCSF PREP Program Training June 23, 2011 Adolescent Substance Use Critical time for onset of SUDS Experimentation is prevalent; most do not develop SUDS Prevalence rates in higher risk samples is approx 24% or higher Social factors, esp peer influence, are strongest determinants of initiation of use. Psychological factors and effects of the substances more closely linked to abuse. (Millin & Walker, 2011) Adolescent Substance Abuse Marijuana is the most prevalent, then alcohol. Polydrug use is the norm Tobacco: most smokers initiate during adolescence Prescription drug abuse is rising Adolescent brain more is susceptible to alcohol and other drugs Prevention efforts target salient risk and protective factors Protective Factors Positive temperament/self-acceptance Intellectual ability/academic performance Supportive family/home environment Caring relationship with at least one adult External support system that encourages prosocial values Law abidance/avoidance of delinquent peer friendships (Millin & Walker, 2011) Marijuana Impact on developing brain Distortions of self-concept due to disturbances of attention and concentration Conclude they are not intelligent, don’t like school; seek peer group with negative attitudes and behaviors Increased risk of psychotic illness Possible interference with medications (Zweben & Martin, 2009) Tobacco Most smokers initiate in adolescence; 1/3 are current smokers (Randall & Upadhyaya 2009) Early onset smokers more like to develop SUDS Approx 50% of the risk for nicotine dependence is genetic Effective pharmacological tx – little is known Adolescent smokers at significantly greater risk for relapse following tx (de Dios et al, 2009; Meyers & Prochaska, 2008) Relapse Low rates (50%) of continuous abstinence at 3 months following tx Common context: social situation, peer influence. (Adults: negative intra- or interpersonal states) PREP clients seen long term; this is an advantage Adolescent Treatment and Relapse Prevention Tailor to biopsychosocial level of development Family involvement necessary; improves outcomes Integrated treatment of comorbid conditions is crucial; prevalence of COD is higher than in other age group populations Comprehensive services, longer time in tx Pharmacotherapy for SUDS Usually used only for comorbid conditions, not SUDS Barriers Lack of safety and efficacy info Reluctance to use medications to treat SUD Recent RCTs using buprenorphine (for opiate dependence) show greater retention and abstinence Adolescent Treatment Approaches for SUDS Family therapy Multidimensional family therapy (MDFT) Brief strategic family therapy (BSFT) Multisystemic therapy (MST) Functional family therapy Behavioral family therapy Cognitive behavioral therapy Twelve-step approaches Therapeutic communities Community reinforcement/contingency management (Jaffe et al, 2009) Treatment Outcome Parameters (Adolescents) Attrition rates 20%-50% across program types Low motivation Don’t perceive AOD use as a problem Early therapeutic alliance increases retention and predicts better outcomes on drug use, internalizing and externalizing behaviors BASIC ISSUES (AOD) Capsule Definition of Addiction Addiction is behavior that is compulsive, not under dependable control, and persists despite adverse consequences Behavior is voluntary during the initiation stage, but becomes compulsive over time Importance of physical dependence has evolved to concepts of dyscontrol, salience, and neuroadaptation. BUT Any amount of alcohol/drug use is undesirable in persons with cooccurring disorders, and should be recognized and addressed Compulsive Drug Seeking is Initiated Outside Consciousness “cues are registered and acted upon by evolutionary primitive regions of the brain before consciousness occurs” Set in motion by nucleus accumbens (limbic structure, “animal brain”) Sets in motion a pattern of learned compulsive behavior Difficult to override even when negative consequences are recognized (Sellman 2009) Role of Genetic Heritage Heritability estimates range from 40% - 60%. Varies with different drugs. No single gene, or even a handful of genes Complex interaction between genes, especially those that influence temperament, and environmental factors Current model is interactive, “nature via nurture” Co-occurring Disorders (COD) are the Norm, not the Exception We still design our treatment systems around our own limitations Addiction treatment system is the default for almost everyone except those with SMI Attitudes towards medications have changed in the addiction treatment system Clinicians endorse the idea of integrated treatment, but research lags behind Criteria for many addiction research studies exclude people with COD, particularly SMI And, criteria for SMI studies exclude COD Addiction is a Chronic Relapsing Disorder Similar to diabetes, asthma, hypertension Key factors for all four: Adherence to treatment recommendations Family and social support Poverty factors Stigma influential in determining attitudes towards addiction (e.g, re-occurrence vs relapse) Research often based on acute care model (McLellan et al, JAMA, 2000) Different Treatments Produce Similar Outcomes Main Models: Motivational enhancement Cognitive-behavioral (CBT) Twelve-step facilitation Community reinforcement Modest effect sizes Therapeutic alliance not well studied in addiction treatment research; many studies elsewhere Inadequate understanding of key implementation factors What About the Therapeutic Alliance? Studies outside substance abuse show this accounts for a greater % of the variance than specific techniques Different “specific” therapies yield similar outcomes, but there is wide variability across sites and therapists More therapist education/experience does not improve efficacy (Adapted from W.R. Miller, Oct 06) Motivational Enhancement Motivation is amenable to clinical intervention (vs “come back when you are ready”) Assess stage of motivation and select intervention accordingly Remember that motivation is a variable state, not a fixed trait Combination of internal motivation and external pressure is helpful Treatment Should be Individualized and Comprehensive Addiction is a biopsychosocial disorder Emphasis on evidence-based treatments can lead to another version of cookie-cutter treatment Practical problems (legal, vocational) are important in addition to medical, psychiatric and family issues The community context is relevant Treatment Philosophies: Abstinence-Oriented abstain from drug of choice abstain from other intoxicants drug substitution role in precipitating relapse dependable control not possible; hence detach widest margin of safety Treatment Philosophies: Harm Reduction “Harm reduction is a set of strategies that encourage substance users and service providers to reduce the harm done to drug users, their loved ones and communities by their licit and illicit drug use.” The Harm Reduction Working Group & Coalition, 1995 Pitfalls of Abstinence-Oriented Treatment Failure to assess motivation level before pushing abstinence commitment Failure to understand factors promoting continued use Unrealistic timetables Power struggle vs clinical approach Failure to recognize fluctuating motivation Inappropriate termination of treatment Pitfalls of Harm Reduction Approach Inappropriately low expectations for what client can achieve Difficulty setting clear goals Reluctance to ask client to abstain completely Underestimate risks/lethality Clinician alcohol and/or illicit drug use Abstinence & Harm Reduction It’s a continuum, not a polarity Clients choose goals; professionals give clear recommendations and feedback Considerations differ for individuals and groups, and especially for residential treatment Self-Medication Theory Two versions: etiological - psychiatric disorder “causes” the person to develop substance abuse coping method - substances are used to cope with the psychiatric disorder VS: many factors initiate; those and others perpetuate Addressing the Client’s SelfMedication Perspective Acknowledge that drugs may work in the short run Use journal to get long term view “On balance, is your life getting better or worse since you started drinking/using? Interference with prescribed medications Offer alternatives to deal with social situations, emotional distress, etc. Role of the Spiritual Awakening Many recover without a dramatic spiritual awakening Must reorient to a healthy sense of purpose and meaning Higher power comes in many forms; can reframe to inner wisdom, higher consciousness, etc. Recovery-Oriented Systems of Care (ROSC) System must address a chronic (not acute) disorder Treatment plays an important role, but cannot meet all needs Communities of recovery play a key role in long term success; must have assertive linkages (William White, 2008) Key Ingredients of the Community Model Co-occurring disorders arise in a community context Identification of problems must include the community context Plans for recovery include building a healthy level of community support Successful treatment isn’t just clinical Post Treatment Recovery Environment Mutual aid system (aka self help) Family Social network Living environment Recovery homes, schools, support centers, churches, etc. Essential Elements of Treatment Start where pt is willing to begin Involve family members Structure, structure, structure Appropriate integration with treatment of psychiatric disorder(s) Participation in a community that supports the recovery process What is Recovery? Resolution of AOD problems Progressive achievement of physical, emotional and relational health Citizenship: life meaning and purpose, self-development, social stability, social contribution, elimination of threats to public safety (William White, 2009) www.ebcrp.org